Osteoarthritis: Difference between revisions
m →Signs and symptoms: linked joint locking |
→Alternative medicine: added balneotherapy cochrane review concl |
||
| Line 223: | Line 223: | ||
A [[Cochrane review]] of [[low level laser therapy]] found unclear evidence of benefit.<ref>{{cite journal|last1=Brosseau|first1=L|last2=Welch|first2=V|last3=Wells|first3=G|last4=DeBie|first4=R|last5=Gam|first5=A|last6=Harman|first6=K|last7=Morin|first7=M|last8=Shea|first8=B|last9=Tugwell|first9=P|title=Low level laser therapy (Classes I, II and III) for treating osteoarthritis.|journal=Cochrane Database of Systematic Reviews|date=2004|issue=3|pages=CD002046|pmid=15266461|doi=10.1002/14651858.CD002046.pub2}}</ref> Another review found short term pain relief for osteoarthritic knees.<ref>{{cite journal|last1=Bjordal|first1=J|last2=Johnson|first2=M|last3=Lopes-Martins|first3=R|last4=Bogen|first4=B|last5=Chow|first5=R|last6=Ljunggren|first6=A|title=Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials.|journal=BMC Musculoskeletal Disorders|date=2007|issue=1|pages=51|doi=10.1186/1471-2474-8-51|volume=8}}</ref> |
A [[Cochrane review]] of [[low level laser therapy]] found unclear evidence of benefit.<ref>{{cite journal|last1=Brosseau|first1=L|last2=Welch|first2=V|last3=Wells|first3=G|last4=DeBie|first4=R|last5=Gam|first5=A|last6=Harman|first6=K|last7=Morin|first7=M|last8=Shea|first8=B|last9=Tugwell|first9=P|title=Low level laser therapy (Classes I, II and III) for treating osteoarthritis.|journal=Cochrane Database of Systematic Reviews|date=2004|issue=3|pages=CD002046|pmid=15266461|doi=10.1002/14651858.CD002046.pub2}}</ref> Another review found short term pain relief for osteoarthritic knees.<ref>{{cite journal|last1=Bjordal|first1=J|last2=Johnson|first2=M|last3=Lopes-Martins|first3=R|last4=Bogen|first4=B|last5=Chow|first5=R|last6=Ljunggren|first6=A|title=Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials.|journal=BMC Musculoskeletal Disorders|date=2007|issue=1|pages=51|doi=10.1186/1471-2474-8-51|volume=8}}</ref> |
||
Further research is needed to determine if [[Balneotherapy|balnotherapy]] for osteoarthritis (mineral baths / spa treatments) improves a persons quality of life or ability to function.<ref>{{Cite journal|last=Verhagen|first=A. P.|last2=Bierma-Zeinstra|first2=S. M. A.|last3=Boers|first3=M.|last4=Cardoso|first4=J. R.|last5=Lambeck|first5=J.|last6=de Bie|first6=R. A.|last7=de Vet|first7=H. C. W.|date=2007-10-17|title=Balneotherapy for osteoarthritis|url=|journal=The Cochrane Database of Systematic Reviews|volume=|issue=4|pages=CD006864|doi=10.1002/14651858.CD006864|issn=1469-493X|pmid=17943920|via=}}</ref> |
|||
==Epidemiology== |
==Epidemiology== |
||
Revision as of 16:35, 30 January 2018
| Osteoarthritis | |
|---|---|
| Other names | Degenerative arthritis, degenerative joint disease, osteoarthrosis |
 | |
| The formation of hard knobs at the middle finger joints (known as Bouchard's nodes) and at the farthest away finger joint (known as Heberden's node) are a common feature of osteoarthritis in the hands. | |
| Specialty | Rheumatology, orthopedics |
| Symptoms | Joint pain, stiffness, joint swelling, decreased range of motion[1] |
| Usual onset | Over years[1] |
| Causes | Previous joint injury, abnormal joint or limb development, inherited factors[1][2] |
| Risk factors | Overweight, legs of a different length, job with high levels of joint stress[1][2] |
| Diagnostic method | Based on symptoms[1] |
| Treatment | Exercise, efforts to decrease joint stress, support groups, pain medications, joint replacement[1][2][3] |
| Frequency | 237 million / 3.3% (2015)[4] |
Osteoarthritis (OA) is a type of joint disease that results from breakdown of joint cartilage and underlying bone.[5] The most common symptoms are joint pain and stiffness.[1] Initially, symptoms may occur only following exercise, but over time may become constant.[1] Other symptoms may include joint swelling, decreased range of motion, and when the back is affected weakness or numbness of the arms and legs.[1] The most commonly involved joints are those near the ends of the fingers, at the base of the thumb, neck, lower back, knee, and hips.[1] Joints on one side of the body are often more affected than those on the other.[1] Usually the symptoms come on over years.[1] It can affect work and normal daily activities.[1] Unlike other types of arthritis, only the joints are typically affected.[1]
Causes include previous joint injury, abnormal joint or limb development, and inherited factors.[1][2] Risk is greater in those who are overweight, have one leg of a different length, and have jobs that result in high levels of joint stress.[1][2][6] Osteoarthritis is believed to be caused by mechanical stress on the joint and low grade inflammatory processes.[7] It develops as cartilage is lost and the underlying bone becomes affected.[1] As pain may make it difficult to exercise, muscle loss may occur.[2][8] Diagnosis is typically based on signs and symptoms, with medical imaging and other tests occasionally used to either support or rule out other problems.[1] In contrast to rheumatoid arthritis, which is primarily an inflammatory condition, in osteoarthritis, the joints do not typically become hot or red.[1]
Treatment includes exercise, efforts to decrease joint stress, support groups, and pain medications.[1][3] Efforts to decrease joint stress include resting and the use of a cane.[1] Weight loss may help in those who are overweight.[1] Pain medications may include paracetamol (acetaminophen) as well as NSAIDs such as naproxen or ibuprofen.[1] Long-term opioid use is generally discouraged due to lack of information on benefits as well as risks of addiction and other side effects.[1][3] If pain interferes with normal life despite other treatments, joint replacement surgery may help.[2] An artificial joint typically lasts 10 to 15 years.[9]
Osteoarthritis is the most common form of arthritis affecting about 237 million (3.3%) of the population.[4][10] Among those over 60 years old, about 10% of males and 18% of females are affected.[2] It is the cause of about 2% of years lived with disability.[10] In Australia, about 1.9 million people are affected,[11] and in the United States, 30 to 52.5 million people are affected.[12][13] It becomes more common in both sexes as people become older.[1]
Signs and symptoms

The main symptom is pain, causing loss of ability and often stiffness. The pain is typically made worse by prolonged activity and relieved by rest. Stiffness is most common in the morning, and typically lasts less than thirty minutes after beginning daily activities, but may return after periods of inactivity. Osteoarthritis can cause a crackling noise (called "crepitus") when the affected joint is moved, especially shoulder and knee joint. A person may also complain of joint locking and joint instability. These symptoms would affect their daily activities due to pain and stiffness.[14] Some people report increased pain associated with cold temperature, high humidity, or a drop in barometric pressure, but studies have had mixed results.[15]
Osteoarthritis commonly affects the hands, feet, spine, and the large weight-bearing joints, such as the hips and knees, although in theory, any joint in the body can be affected. As osteoarthritis progresses, movement patterns (such as gait), are typically affected.[16] Osteoarthritis is the most common cause of a joint effusion of the knee.[17]
In smaller joints, such as at the fingers, hard bony enlargements, called Heberden's nodes (on the distal interphalangeal joints) or Bouchard's nodes (on the proximal interphalangeal joints), may form, and though they are not necessarily painful, they do limit the movement of the fingers significantly. Osteoarthritis of the toes may be a factor causing formation of bunions,[18] rendering them red or swollen.
Risk factors
Damage from mechanical stress with insufficient self repair by joints is believed to be the primary cause of osteoarthritis.[19] Sources of this stress may include misalignments of bones caused by congenital or pathogenic causes; mechanical injury; excess body weight; loss of strength in the muscles supporting a joint; and impairment of peripheral nerves, leading to sudden or uncoordinated movements.[19] However exercise, including running in the absence of injury, has not been found to increase the risk.[20] Nor has cracking one's knuckles been found to play a role.[21]
Primary
A number of studies have shown that there is a greater prevalence of the disease among siblings and especially identical twins, indicating a hereditary basis.[22] Although a single factor is not generally sufficient to cause the disease, about half of the variation in susceptibility has been assigned to genetic factors.[23]
As early human ancestors evolved into bipeds, changes occurred in the pelvis, hip joint and spine which increased the risk of osteoarthritis.[24] Additionally genetic variations that increase the risk were likely not selected against because usually problems only occur after reproductive success.[25]
The development of osteoarthritis is correlated with a history of previous joint injury and with obesity, especially with respect to knees.[26] Since the correlation with obesity has been observed not only for knees but also for non-weight bearing joints and the loss of body fat is more closely related to symptom relief than the loss of body weight, it has been suggested that there may be a metabolic link to body fat as opposed to just mechanical loading.[27]
Changes in sex hormone levels may play a role in the development of osteoarthritis as it is more prevalent among post-menopausal women than among men of the same age.[28][29] A study of mice found natural female hormones to be protective while injections of the male hormone dihydrotestosterone reduced protection.[30]
Increased risk of developing knee and hip osteoarthritis was found in those who:[6]
- work with manual handling (e.g. lifting)[6]
- have physically demanding work[6]
- walk at work[6]
- have climbing tasks at work (e.g. climb stairs or ladders)[6]
Increased risk of developing hip osteoarthritis over time was found among those who work in bent or twisted positions.[6]
Increased risk of knee osteoarthritis was found in those who:[6]
- work in a kneeling or squatting position[6]
- experience heavy lifting in combination with a kneeling or squatting posture[6]
- work standing up[6]
Secondary
This type of osteoarthritis is caused by other factors but the resulting pathology is the same as for primary osteoarthritis:
- Alkaptonuria
- Congenital disorders of joints
- Diabetes doubles the risk of having a joint replacement due to osteoarthritis and people with diabetes have joint replacements at a younger age than those without diabetes.[31]
- Ehlers-Danlos Syndrome
- Hemochromatosis and Wilson's disease
- Inflammatory diseases (such as Perthes' disease), (Lyme disease), and all chronic forms of arthritis (e.g., costochondritis, gout, and rheumatoid arthritis). In gout, uric acid crystals cause the cartilage to degenerate at a faster pace.
- Injury to joints or ligaments (such as the ACL), as a result of an accident or orthopedic operations.
- Ligamentous deterioration or instability may be a factor.
- Marfan syndrome
- Obesity
- Joint infection
Pathophysiology
While osteoarthritis is a degenerative joint disease that may cause gross cartilage loss and morphological damage to other joint tissues, more subtle biochemical changes occur in the earliest stages of osteoarthritis progression. The water content of healthy cartilage is finely balanced by compressive force driving water out and hydrostatic and osmotic pressure drawing water in.[33][34] Collagen fibres exert the compressive force, whereas the Gibbs–Donnan effect and cartilage proteoglycans create osmotic pressure which tends to draw water in.[34]
However, during onset of osteoarthritis, the collagen matrix becomes more disorganized and there is a decrease in proteoglycan content within cartilage. The breakdown of collagen fibers results in a net increase in water content.[35][36][37][38][39] This increase occurs because whilst there is an overall loss of proteoglycans (and thus a decreased osmotic pull),[36][40] it is outweighed by a loss of collagen.[34][40] Without the protective effects of the proteoglycans, the collagen fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration. Inflammation of the synovium (joint cavity lining) and the surrounding joint capsule can also occur, though often mild (compared to the synovial inflammation that occurs in rheumatoid arthritis). This can happen as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them.[citation needed]
Other structures within the joint can also be affected.[41] The ligaments within the joint become thickened and fibrotic and the menisci can become damaged and wear away.[42] Menisci can be completely absent by the time a person undergoes a joint replacement. New bone outgrowths, called "spurs" or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces in the absence of the menisci. The subchondral bone volume increases and becomes less mineralized (hypomineralization).[43] All these changes can cause problems functioning. The pain in an osteoarthritic joint has been related to thickened synovium[44] and subchondral bone lesions.[45]
Diagnosis
Diagnosis is made with reasonable certainty based on history and clinical examination.[46][47] X-rays may confirm the diagnosis. The typical changes seen on X-ray include: joint space narrowing, subchondral sclerosis (increased bone formation around the joint), subchondral cyst formation, and osteophytes.[48] Plain films may not correlate with the findings on physical examination or with the degree of pain.[49] Usually other imaging techniques are not necessary to clinically diagnose osteoarthritis.
In 1990, the American College of Rheumatology, using data from a multi-center study, developed a set of criteria for the diagnosis of hand osteoarthritis based on hard tissue enlargement and swelling of certain joints.[50] These criteria were found to be 92% sensitive and 98% specific for hand osteoarthritis versus other entities such as rheumatoid arthritis and spondyloarthropathies.[51]
Related pathologies whose names may be confused with osteoarthritis include pseudo-arthrosis. This is derived from the Greek roots pseudo-, meaning "false", and arthr-, meaning "joint", together with the ending -osis used for disorders. Radiographic diagnosis results in diagnosis of a fracture within a joint, which is not to be confused with osteoarthritis which is a degenerative pathology affecting a high incidence of distal phalangeal joints of female patients. A polished ivory-like appearance may also develop on the bones of the affected joints, reflecting a change called eburnation.[52]
-
Severe osteoarthritis and osteopenia of the carpal joint and 1st carpometacarpel joint.
-
MRI of osteoarthritis in the knee, with characteristic narrowing of the joint space.
-
Primary osteoarthritis of the left knee. Note the osteophytes, narrowing of the joint space (arrow), and increased subchondral bone density (arrow).
-
Damaged cartilage from sows. (a) cartilage erosion (b)cartilage ulceration (c)cartilage repair (d)osteophyte (bone spur) formation.
-
Histopathology of osteoarthrosis of a knee joint in an elderly female.
-
Histopathology of osteoarthrosis of a knee joint in an elderly female.
-
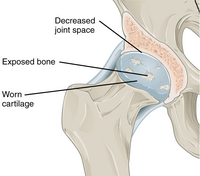
In a healthy joint, the ends of bones are encased in smooth cartilage. Together, they are protected by a joint capsule lined with a synovial membrane that produces synovial fluid. The capsule and fluid protect the cartilage, muscles, and connective tissues.
-
With osteoarthritis, the cartilage becomes worn away. Spurs grow out from the edge of the bone, and synovial fluid increases. Altogether, the joint feels stiff and sore.
-
Osteoarthritis
Classification
A number of classification systems are used for gradation of osteoarthritis:
- WOMAC scale, taking into account pain, stiffness and functional limitation.[53]
- Kellgren-Lawrence grading scale for osteoarthritis of the knee. It uses only projectional radiography features.
- Tönnis classification for osteoarthritis of the hip joint, also using only projectional radiography features.[54]
- Knee injury and Osteoarthritis Outcome Score (KOOS) and Hip disability and Osteoarthritis Outcome Score (HOOS) surveys.[55][56]
Osteoarthritis can be classified into either primary or secondary depending on whether or not there is an identifiable underlying cause.
Both primary generalized nodal osteoarthritis and erosive osteoarthritis (EOA, also called inflammatory osteoarthritis) are sub-sets of primary osteoarthritis. EOA is a much less common, and more aggressive inflammatory form of osteoarthritis which often affects the distal interphalangeal joints of the hand and has characteristic articular erosive changes on x-ray.[57]
Osteoarthritis can be classified by the joint affected:
- Hand:
- Wrist (wrist osteoarthritis)
- Vertebral column (spondylosis)
- Hip osteoarthritis
- Knee osteoarthritis
Management

Lifestyle modification (such as weight loss and exercise) and analgesics are the mainstays of treatment. Acetaminophen (also known as paracetamol) is recommended first line with NSAIDs being used as add on therapy only if pain relief is not sufficient.[58] This is due to the relative greater safety of acetaminophen.[58]
Lifestyle changes
For overweight people, weight loss may be an important factor.[59] Patient education has been shown to be helpful in the self-management of arthritis.[59] It decreases pain, improves function, reduces stiffness and fatigue, and reduces medical usage.[59] Patient education can provide on average 20% more pain relief when compared to NSAIDs alone in patients with hip osteoarthritis.[59]
Physical measures
Moderate exercise is beneficial with respect to pain and function in those with osteoarthritis of the knee and hip.[60][61] These exercises should occur at least three times per week.[62] While some evidence supports certain physical therapies, evidence for a combined program is limited.[63] There is not enough evidence to determine the effectiveness of massage therapy.[64] The evidence for manual therapy is inconclusive.[65] Functional, gait, and balance training have been recommended to address impairments of position sense, balance, and strength in individuals with lower extremity arthritis as these can contribute to a higher rate of falls in older individuals.[66]
Lateral wedge insoles and neutral insoles do not appear to be useful in osteoarthritis of the knee.[67][68][69] Knee braces may help[70] but their usefulness has also been disputed.[69] For pain management heat can be used to relieve stiffness, and cold can relieve muscle spasms and pain.[71] Among people with hip and knee osteoarthritis, exercise in water may reduce pain and disability, and increase quality of life in the short term.[72] Also therapeutic exercise programs such as aerobics and walking reduce pain and improve physical functioning for up to 6 months after the end of the program for people with knee osteoarthritis.[73]
Medication
| Treatment recommendations by risk factors | ||
|---|---|---|
| GI risk | CVD risk | Option |
| Low | Low | NSAID, or paracetamol[74] |
| Moderate | Low | Paracetamol, or low dose NSAID with antacid[74] |
| Low | Moderate | Paracetamol, or low dose aspirin with an antacid[74] |
| Moderate | Moderate | Low dose paracetamol, aspirin, and antacid. Monitoring for abdominal pain or black stool.[74] |
The pain medication acetaminophen is the first line treatment for osteoarthritis.[58][75] However, a 2015 review found acetaminophen to only have a small short-term benefit.[76] For mild to moderate symptoms effectiveness is similar to non-steroidal anti-inflammatory drugs (NSAIDs), though for more severe symptoms NSAIDs may be more effective.[58] NSAIDs such as naproxen, while more effective in severe cases, are associated with greater side effects, such as gastrointestinal bleeding.[58] Diclofenac may be the most effective NSAID.[77]
Another class of NSAIDs, COX-2 selective inhibitors (such as celecoxib) are equally effective when compared to nonselective NSAIDs, and have lower rates of adverse gastrointestinal effects, but higher rates of cardiovascular disease such as myocardial infarction.[78] They are also more expensive than non-specific NSAIDs.[79] Benefits and risks vary in individuals and need consideration when making treatment decisions.[80] NSAIDS applied topically are effective for a small number of people.[81]
Failure to achieve desired pain relief in osteoarthritis after 2 weeks should trigger reassessment of dosage and pain medication.[82] Opioids by mouth, including both weak opioids such as tramadol and stronger opioids, are also often prescribed. Their appropriateness is uncertain, and opioids are often recommended only when first line therapies have failed or are contraindicated.[83][84] This is due to their small benefit and relatively large risk of side effects.[85] Oral steroids are not recommended in the treatment of osteoarthritis.[75]
There are several NSAIDs available for topical use, including diclofenac. A Cochrane review from 2016 concluded that reasonably reliable evidence is available only for use of topical diclofenac and ketoprofen in people aged over 40 years with painful knee arthritis.[86] Transdermal opioid pain medications are not typically recommended in the treatment of osteoarthritis.[87] The use of topical capsaicin to treat osteoarthritis is controversial, as some reviews found benefit[88][89] while others did not.[90]
Joint injection of glucocorticoids (such as hydrocortisone) leads to short term pain relief that may last between a few weeks and a few months.[91] Injections of hyaluronic acid have not produced improvement compared to placebo for knee arthritis,[92][93] but did increase risk of further pain.[92] In ankle osteoarthritis, evidence is unclear.[94] The effectiveness of injections of platelet-rich plasma is unclear; there are suggestions that such injections improve function but not pain, and are associated with increased risk.[vague][95][96]
A 2015 Cochrane review found that intra-articular corticosteroid injections of the knee did not benefit quality of life and had no effect on knee joint space; clinical effects one to six weeks after injection could not be determined clearly due to poor study quality.[97] Another 2015 study reported negative effects of intra-articular corticosteroid injections at higher doses,[98] and a 2017 trial showed reduction in cartilage thickness with intra-articular triamcinolone every 12 weeks for 2 years compared to placebo.[99]
Surgery
If the impact of symptoms of osteoarthritis on quality of life is significant and more conservative management is ineffective, joint replacement surgery or resurfacing may be recommended. Evidence supports joint replacement for both knees and hips as it is both clinically effective,[100][101] and cost-effective.[102][103] Surgery to transfer articular cartilage from a non-weight-bearing area to the damaged area is one possible procedure that has some success, but there are problems getting the transferred cartilage to integrate well with the existing cartilage at the transfer site.[104]
Osteotomy may be useful in people with knee osteoarthritis, but has not been well studied.[105] Arthroscopic surgery is largely not recommended, as it does not improve outcomes in knee osteoarthritis,[106][107] and may result in harm.[108]
Alternative medicine
Glucosamine and chondroitin
The effectiveness of glucosamine is controversial.[109] Reviews have found it to be equal to[110][111] or slightly better than placebo.[112][113] A difference may exist between glucosamine sulfate and glucosamine hydrochloride, with glucosamine sulfate showing a benefit and glucosamine hydrochloride not.[114] The evidence for glucosamine sulfate having an effect on osteoarthritis progression is somewhat unclear and if present likely modest.[115] The Osteoarthritis Research Society International recommends that glucosamine be discontinued if no effect is observed after six months[116] and the National Institute for Health and Care Excellence no longer recommends its use.[8] Despite the difficulty in determining the efficacy of glucosamine, it remains a viable treatment option.[117] The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) recommends glucosamine sulfate and chondroitin sulfate for knee osteoarthritis.[118] Its use as a therapy for osteoarthritis is usually safe.[117][119]
A 2015 Cochrane review of clinical trials of chondroitin found that most were of low quality, but that there was some evidence of short-term improvement in pain and few side effects; it does not appear to improve or maintain the health of affected joints.[120]
Other remedies
Avocado/soybean unsaponifiables (ASU) is an extract made from avocado oil and soybean oil[121] that is sold under many brand names worldwide as a dietary supplement[122] and as a drug in France.[123] A 2014 Cochrane review found that while ASU might help relieve pain in the short term for some people with osteoarthritis, it does not appear to improve or maintain the health of affected joints; the review noted a high quality two year clinical trial comparing to ASU to chondroitin, which has uncertain efficacy in arthritis—the study found no difference between the two.[121] The review also found that while ASU appears to be safe, it has not been adequately studied to be sure.[121]
Devil's claw,[124] Curcumin,[125] phytodolor,[88] SKI306X[89][126] and SAMe[88][127] may be effective in improving pain. There is tentative evidence to support cat's claw,[128] hyaluronan,[129] MSM,[88][126] and rose hip.[88] A few high-quality studies of Boswellia serrata show consistent, but small, improvements in pain and function.[121]
There is little evidence supporting benefits for some supplements, including: the Ayurvedic herbal preparations with brand names Articulin F and Eazmov, collagen, Duhuo Jisheng Wan (a Chinese herbal preparation), fish liver oil, ginger, the herbal preparation gitadyl, omega-3 fatty acids, the brand-name product Reumalax, stinging nettle, vitamins A, C, and E in combination, vitamin E alone, vitamin K, vitamin D and willow bark. There is insufficient evidence to make a recommendation about the safety and efficacy of these treatments.[88][128][130]
Acupuncture and other interventions
While acupuncture leads to improvements in pain relief, this improvement is small and may be of questionable importance.[131] Waiting list-controlled trials for peripheral joint osteoarthritis do show clinically relevant benefits, but these may be due to placebo effects.[132] Acupuncture does not seem to produce long-term benefits.[133] While electrostimulation techniques such as TENS have been used for twenty years to treat osteoarthritis in the knee, there is no conclusive evidence to show that it reduces pain or disability.[134]
A Cochrane review of low level laser therapy found unclear evidence of benefit.[135] Another review found short term pain relief for osteoarthritic knees.[136]
Further research is needed to determine if balnotherapy for osteoarthritis (mineral baths / spa treatments) improves a persons quality of life or ability to function.[137]
Epidemiology
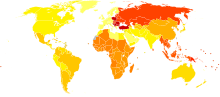
| no data ≤ 200 200–220 220–240 240–260 260–280 280–300 | 300–320 320–340 340–360 360–380 380–400 ≥ 400 |
Globally as of 2010, approximately 250 million people had osteoarthritis of the knee (3.6% of the population).[139][140] Hip osteoarthritis affects about 0.85% of the population.[139]
As of 2004[update], osteoarthritis globally causes moderate to severe disability in 43.4 million people.[141] Together, knee and hip osteoarthritis had a ranking for disability globally of 11th among 291 disease conditions assessed.[139]
United States
As of 2012, osteoarthritis affected 52.5 million people in the United States, approximately 50% of whom were 65 years and older.[12] It is estimated that 80% of the population have radiographic evidence of osteoarthritis by age 65, although only 60% of those will have symptoms.[142] The rate of osteoarthritis in the United States is forecast to be 78 million (26%) adults by 2040.[12]
In the United States, there were approximately 964,000 hospitalizations for osteoarthritis in 2011, a rate of 31 stays per 10,000 population.[143] With an aggregate cost of $14.8 billion ($15,400 per stay), it was the second-most expensive condition seen in U.S. hospital stays in 2011. By payer, it was the second-most costly condition billed to Medicare and private insurance.[144][145]
History
Evidence for osteoarthritis found in the fossil record is studied by paleopathologists, specialists in ancient disease and injury. Osteoarthritis has been reported in fossils of the large carnivorous dinosaur Allosaurus fragilis.[146]
Human knee osteoarthritis may have doubled between early industrial era (env. 19th c.), and postindustrial era (env. 20th c.), per a study of skeletons.[147]
Etymology
Osteoarthritis is derived from the Greek word part osteo-, meaning "of the bone", combined with arthritis: arthr-, meaning "joint", and -itis, the meaning of which has come to be associated with inflammation.[148] The -itis of osteoarthritis could be considered misleading as inflammation is not a conspicuous feature. Some clinicians refer to this condition as osteoarthrosis to signify the lack of inflammatory response.[149]
Research
There are ongoing efforts to determine if there are agents that modify outcomes in osteoarthritis. Sprifermin is one candidate drug. There is also tentative evidence that strontium ranelate may decrease degeneration in osteoarthritis and improve outcomes.[150][151]
As well as attempting to find disease-modifying agents for osteoarthritis, there is emerging evidence that a system-based approach is necessary to find the causes of osteoarthritis.[152] Changes may occur before clinical disease is evident due to abnormalities in biomechanics, biology or structure of joints that predispose them to develop clinical disease. Research is thus focusing on defining these early pre-osteoarthritis changes using biological, mechanical, and imaging markers of osteoarthritis risk, emphasising multi-disciplinary approaches, and looking into personalized interventions that can reverse osteoarthritis risk in healthy joints before the disease becomes evident.
Gene transfer strategies aim to target the disease process rather than the symptoms.[153]
Cell-mediated gene therapy is being studied.[154][155] One version is approved in South Korea for the treatment of moderate knee osteoarthritis.[156] It is not approved in the United States where it was developed as of 2017.[156] The drug is administered intra-articularly.[156]
Biomarkers
Guidelines outlining requirements for inclusion of soluble biomarkers in osteoarthritis clinical trials were published in 2015,[157] but as yet, there are no validated biomarkers for osteoarthritis. A 2015 systematic review of biomarkers for osteoarthritis looking for molecules that could be used for risk assessments found 37 different biochemical markers of bone and cartilage turnover in 25 publications.[158] The strongest evidence was for urinary C-terminal telopeptide of collagen type II (uCTX-II) as a prognostic marker for knee osteoarthritis progression and serum cartilage oligomeric protein (COMP) levels as a prognostic marker for incidence of both knee and hip osteoarthritis. A review of biomarkers in hip osteoarthritis also found associations with uCTXII.[159] Procollagen type II C-terminal propeptide (PIICP) levels reflect type II collagen synthesis in body and within joint fluid PIICP levels can be used as a prognostic marker for early osteoarthritis.[160]
One problem with using a specific collagen type II biomarker from the breakdown of articular cartilage is that the amount of cartilage is reduced (worn away) over time with progression of the disease so a patient can eventually have very advanced osteoarthritis with none of this biomarker detectable in their urine. Another problem with a systemic biomarker is that a patient can have osteoarthritis in multiple joints at different stages of disease at the same time, so the biomarker source cannot be determined. Some other collagen breakdown products in the synovial fluid correlated with each other after acute injuries (a known cause of secondary osteoarthritis) but did not correlate with the severity of the injury.[161]
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y "Osteoarthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. April 2015. Archived from the original on 18 May 2015. Retrieved 13 May 2015.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h Glyn-Jones, S; Palmer, AJ; Agricola, R; Price, AJ; Vincent, TL; Weinans, H; Carr, AJ (3 March 2015). "Osteoarthritis". Lancet. 386: 376–87. doi:10.1016/S0140-6736(14)60802-3. PMID 25748615.
- ^ a b c McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, Hawker GA, Henrotin Y, Hunter DJ, Kawaguchi H, Kwoh K, Lohmander S, Rannou F, Roos EM, Underwood M (2014). "OARSI guidelines for the non-surgical management of knee osteoarthritis". Osteoarthr. Cartil. 22 (3): 363–88. doi:10.1016/j.joca.2014.01.003. PMID 24462672.
- ^ a b GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ Atlas of Osteoarthritis. Springer. 2015. p. 21. ISBN 9781910315163. Archived from the original on 2017-09-08.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h i j k Swedish Agency for Health Technology Assessment and Assessment of Social Services, Statens beredning för medicinsk och social utvärdering (SBU) (1 September 2016). "Occupational Exposures and Osteoarthritis". www.sbu.se. Archived from the original on 2017-06-14. Retrieved 2017-06-08.
{{cite web}}: Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ^ Berenbaum F (2013). "Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!)". Osteoarthritis and Cartilage. 21 (1): 16–21. doi:10.1016/j.joca.2012.11.012. PMID 23194896.
- ^ a b Conaghan P (2014). "Osteoarthritis — Care and management in adults". Archived from the original (PDF) on 2015-12-22.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Di Puccio, F; Mattei, L (18 January 2015). "Biotribology of artificial hip joints". World journal of orthopedics. 6 (1): 77–94. doi:10.5312/wjo.v6.i1.77. PMC 4303792. PMID 25621213.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b March L, Smith EU, Hoy DG, Cross MJ, Sanchez-Riera L, Blyth F, Buchbinder R, Vos T, Woolf AD (2014). "Burden of disability due to musculoskeletal (MSK) disorders". Best Pract Res Clin Rheumatol. 28 (3): 353–66. doi:10.1016/j.berh.2014.08.002. PMID 25481420.
- ^ Elsternwick (2013). "A problem worth solving". Arthritis and Osteoporosis Victoria. Archived from the original on 2015-04-28.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c "Arthritis-Related Statistics: Prevalence of Arthritis in the United States". Centers for Disease Control and Prevention, US Department of Health and Human Services. 9 November 2016. Archived from the original on 29 December 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG (May 2016). "Alternative Methods for Defining Osteoarthritis and the Impact on Estimating Prevalence in a US Population-Based Survey". Arthritis Care Res (Hoboken). 68 (5): 574–80. doi:10.1002/acr.22721.
- ^ Keith, Sinusas (2012). "Osteoarthritis: Diagnosis and Treatment". American Family Physician. 85 (1): 49–56. Retrieved 18 January 2018.
- ^ de Figueiredo EC, Figueiredo GC, Dantas RT (December 2011). "Influência de elementos meteorológicos na dor de pacientes com osteoartrite: Revisão da literatura" [Influence of meteorological elements on osteoarthritis pain: a review of the literature]. Rev Bras Reumatol (in Portuguese). 51 (6): 622–8. doi:10.1590/S0482-50042011000600008. PMID 22124595.
- ^ Vincent, K. R.; Conrad, B. P.; Fregly, B. J.; Vincent, H. K. (2012). "The Pathophysiology of Osteoarthritis: A Mechanical Perspective on the Knee Joint". PM&R: Physical and Rehabilitation Medicine. 4 (5): S3–S9. doi:10.1016/j.pmrj.2012.01.020. PMC 3635670. PMID 22632700.
- ^ "Swollen knee". Mayo Clinic. 2017. Archived from the original on 2017-07-20.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Bunions: Symptoms and causes". Mayo Clinic. 8 November 2016. Archived from the original on 21 April 2017. Retrieved 20 April 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Brandt KD, Dieppe P, Radin E (January 2009). "Etiopathogenesis of osteoarthritis". Med. Clin. North Am. 93 (1): 1–24, xv. doi:10.1016/j.mcna.2008.08.009. PMID 19059018.
- ^ Bosomworth NJ (September 2009). "Exercise and knee osteoarthritis: benefit or hazard?". Can Fam Physician. 55 (9): 871–8. PMC 2743580. PMID 19752252.
- ^ Deweber K, Olszewski M, Ortolano R (2011). "Knuckle cracking and hand osteoarthritis". J Am Board Fam Med. 24 (2): 169–74. doi:10.3122/jabfm.2011.02.100156. PMID 21383216.
- ^ Valdes AM, Spector TD (August 2008). "The contribution of genes to osteoarthritis". Rheum. Dis. Clin. North Am. 34 (3): 581–603. doi:10.1016/j.rdc.2008.04.008. PMID 18687274.
- ^ Spector TD, MacGregor AJ (2004). "Risk factors for osteoarthritis: genetics". Osteoarthr. Cartil. 12 Suppl A: S39–44. doi:10.1016/j.joca.2003.09.005. PMID 14698640.
- ^ Hogervorst T, Bouma HW, de Vos J (August 2009). "Evolution of the hip and pelvis". Acta Orthopaedica Supplementum. 80 (336): 1–39. doi:10.1080/17453690610046620. PMID 19919389.
- ^ van der Kraan PM, van den Berg WB (April 2008). "Osteoarthritis in the context of ageing and evolution. Loss of chondrocyte differentiation block during ageing". Ageing Research Reviews. 7 (2): 106–13. doi:10.1016/j.arr.2007.10.001. PMID 18054526.
- ^ Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C (May 2001). "Knee osteoarthritis and obesity". Int. J. Obes. Relat. Metab. Disord. 25 (5): 622–7. doi:10.1038/sj.ijo.0801585. PMID 11360143.
- ^ Pottie P, Presle N, Terlain B, Netter P, Mainard D, Berenbaum F (November 2006). "Obesity and osteoarthritis: more complex than predicted!". Ann. Rheum. Dis. 65 (11): 1403–5. doi:10.1136/ard.2006.061994. PMC 1798356. PMID 17038451.
- ^ Linn S, Murtaugh B, Casey E (May 2012). "Role of sex hormones in the development of osteoarthritis". PM&R. 4 (5 Suppl): S169–73. doi:10.1016/j.pmrj.2012.01.013. PMID 22632696.
- ^ Tanamas SK, Wijethilake P, Wluka AE, Davies-Tuck ML, Urquhart DM, Wang Y, Cicuttini FM (June 2011). "Sex hormones and structural changes in osteoarthritis: a systematic review". Maturitas. 69 (2): 141–56. doi:10.1016/j.maturitas.2011.03.019. PMID 21481553.
- ^ Ma HL, Blanchet TJ, Peluso D, Hopkins B, Morris EA, Glasson SS (June 2007). "Osteoarthritis severity is sex dependent in a surgical mouse model". Osteoarthr. Cartil. 15 (6): 695–700. doi:10.1016/j.joca.2006.11.005. PMID 17207643.
- ^ King KB, Rosenthal AK (2015). "The adverse effects of diabetes on osteoarthritis: update on clinical evidence and molecular mechanisms". Osteoarthritis Cartilage. 23 (6): 841–50. doi:10.1016/j.joca.2015.03.031. PMID 25837996.
- ^ "OpenStax CNX". cnx.org. Archived from the original on 2016-01-06. Retrieved 2015-10-14.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Sanchez-Adams J, Leddy HA, McNulty AL, O'Conor CJ, Guilak F (2014). "The mechanobiology of articular cartilage: bearing the burden of osteoarthritis". Curr Rheumatol Rep. 16 (10): 451. doi:10.1007/s11926-014-0451-6. PMC 4682660. PMID 25182679.
- ^ a b c Maroudas AI (April 1976). "Balance between swelling pressure and collagen tension in normal and degenerate cartilage". Nature. 260 (5554): 808–9. doi:10.1038/260808a0. PMID 1264261.
- ^ Bollet AJ, Nance JL (July 1966). "Biochemical Findings in Normal and Osteoarthritic Articular Cartilage. II. Chondroitin Sulfate Concentration and Chain Length, Water, and Ash Content". J. Clin. Invest. 45 (7): 1170–7. doi:10.1172/JCI105423. PMC 292789. PMID 16695915.
- ^ a b Brocklehurst R, Bayliss MT, Maroudas A, Coysh HL, Freeman MA, Revell PA, Ali SY (January 1984). "The composition of normal and osteoarthritic articular cartilage from human knee joints. With special reference to unicompartmental replacement and osteotomy of the knee". J Bone Joint Surg Am. 66 (1): 95–106. PMID 6690447.
- ^ Chou MC, Tsai PH, Huang GS, Lee HS, Lee CH, Lin MH, Lin CY, Chung HW (April 2009). "Correlation between the MR T2 value at 4.7 T and relative water content in articular cartilage in experimental osteoarthritis induced by ACL transection". Osteoarthr. Cartil. 17 (4): 441–7. doi:10.1016/j.joca.2008.09.009. PMID 18990590.
- ^ Grushko G, Schneiderman R, Maroudas A (1989). "Some biochemical and biophysical parameters for the study of the pathogenesis of osteoarthritis: a comparison between the processes of ageing and degeneration in human hip cartilage". Connect. Tissue Res. 19 (2–4): 149–76. doi:10.3109/03008208909043895. PMID 2805680.
- ^ Mankin HJ, Thrasher AZ (January 1975). "Water content and binding in normal and osteoarthritic human cartilage". J Bone Joint Surg Am. 57 (1): 76–80. PMID 1123375.
- ^ a b Venn M, Maroudas A (April 1977). "Chemical composition and swelling of normal and osteoarthrotic femoral head cartilage. I. Chemical composition". Ann. Rheum. Dis. 36 (2): 121–9. doi:10.1136/ard.36.2.121. PMC 1006646. PMID 856064.
- ^ Madry H, Luyten FP, Facchini A (2012). "Biological aspects of early osteoarthritis". Knee Surg. Sports Traumatol. Arthrosc. 20 (3): 407–22. doi:10.1007/s00167-011-1705-8. PMID 22009557.
- ^ Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A (2012). "Meniscus pathology, osteoarthritis and the treatment controversy". Nat. Rev. Rheumatol. 8 (7): 412–9. doi:10.1038/nrrheum.2012.69. PMID 22614907.
- ^ Li G, Yin J, Gao J, Cheng TS, Pavlos NJ, Zhang C, Zheng MH (2013). "Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes". Arthritis Research & Therapy. 15 (6): 223. doi:10.1186/ar4405. PMC 4061721. PMID 24321104.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Hill CL, Gale DG, Chaisson CE, Skinner K, Kazis L, Gale ME, Felson DT (2001). "Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis". J. Rheumatol. 28 (6): 1330–7. PMID 11409127.
- ^ Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, Kazis L, Gale DR (3 Apr 2001). "The association of bone marrow lesions with pain in knee osteoarthritis". Ann Intern Med. 134 (7): 541–9. doi:10.7326/0003-4819-134-7-200104030-00007. PMID 11281736.
- ^ Zhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, Bresnihan B, Herrero-Beaumont G, Kirschner S, Leeb BF, Lohmander LS, Mazières B, Pavelka K, Punzi L, So AK, Tuncer T, Watt I, Bijlsma JW (March 2010). "EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis". Ann. Rheum. Dis. 69 (3): 483–9. doi:10.1136/ard.2009.113100. PMID 19762361.
- ^ Bierma-Zeinstra SM, Oster JD, Bernsen RM, Verhaar JA, Ginai AZ, Bohnen AM (August 2002). "Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care". J. Rheumatol. 29 (8): 1713–8. PMID 12180735.
- ^ Osteoarthritis (OA): Joint Disorders at Merck Manual of Diagnosis and Therapy Professional Edition
- ^ Phillips CR, Brasington RD (2010). "Osteoarthritis treatment update: Are NSAIDs still in the picture?". Journal of Musculoskeletal Medicine. 27 (2). Archived from the original on 2010-02-12.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Kalunian KC (2013). "Patient information: Osteoarthritis symptoms and diagnosis (Beyond the Basics)". UpToDate. Archived from the original on 22 September 2010. Retrieved 15 February 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Altman R, Alarcón G, Appelrouth D, Bloch D, Borenstein D, Brandt K, Brown C, Cooke TD, Daniel W, Gray R (November 1990). "The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand". Arthritis Rheum. 33 (11): 1601–10. doi:10.1002/art.1780331101. PMID 2242058.
- ^ Vasan N, Tao L, Vikas B (2010). First Aid for the USMLE Step 1, 2010 (First Aid USMLE). McGraw-Hill Medical. p. 378. ISBN 0-07-163340-5. Archived from the original on 2016-03-16.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Quintana, José M.; Escobar, Antonio; Arostegui, Inmaculada; Bilbao, Amaia; Azkarate, Jesús; Goenaga, J. Ignacio; Arenaza, Juan C. (23 January 2006). "Health-Related Quality of Life and Appropriateness of Knee or Hip Joint Replacement". Archives of Internal Medicine. 166 (2): 220–226. doi:10.1001/archinte.166.2.220.
- ^ "Tönnis Classification of Osteoarthritis by Radiographic Changes". Society of Preventive Hip Surgery. Archived from the original on 2016-12-20. Retrieved 2016-12-13.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "KOOS survey score description and free online calculator – orthotoolkit".
- ^ "HOOS survey score description and free online calculator – orthotoolkit".
- ^ Punzi L, Ramonda R, Sfriso P (October 2004). "Erosive osteoarthritis". Best Pract Res Clin Rheumatol. 18 (5): 739–58. doi:10.1016/j.berh.2004.05.010. PMID 15454130.
- ^ a b c d e Flood J (March 2010). "The role of acetaminophen in the treatment of osteoarthritis". Am J Manag Care. 16 (Suppl Management): S48–54. PMID 20297877. Archived from the original on 2015-03-22.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
- ^ a b c d Cibulka MT, White DM, Woehrle J, Harris-Hayes M, Enseki K, Fagerson TL, Slover J, Godges JJ (April 2009). "Hip pain and mobility deficits—hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association". J Orthop Sports Phys Ther. 39 (4): A1–25. doi:10.2519/jospt.2009.0301. PMID 19352008.
- ^ Hagen KB, Dagfinrud H, Moe RH, Østerås N, Kjeken I, Grotle M, Smedslund G (2012). "Exercise therapy for bone and muscle health: an overview of systematic reviews". BMC Med. 10: 167. doi:10.1186/1741-7015-10-167. PMC 3568719. PMID 23253613.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S (2014). "Exercise for osteoarthritis of the hip". Cochrane Database Syst Rev. 4 (4): CD007912. doi:10.1002/14651858.CD007912.pub2. PMID 24756895.
- ^ Juhl C, Christensen R, Roos EM, Zhang W, Lund H (Mar 2014). "Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials". Arthritis & Rheumatology. 66 (3): 622–36. doi:10.1002/art.38290. PMID 24574223.
- ^ Wang SY, Olson-Kellogg B, Shamliyan TA, Choi JY, Ramakrishnan R, Kane RL (November 2012). "Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review". Annals of Internal Medicine. 157 (9): 632–44. doi:10.7326/0003-4819-157-9-201211060-00007. PMID 23128863.
- ^ De Luigi AJ (May 2012). "Complementary and alternative medicine in osteoarthritis". PM&R. 4 (5 Suppl): S122–33. doi:10.1016/j.pmrj.2012.01.012. PMID 22632691.
- ^ French HP, Brennan A, White B, Cusack T (2011). "Manual therapy for osteoarthritis of the hip or knee — a systematic review". Man Ther. 16 (2): 109–117. doi:10.1016/j.math.2010.10.011. PMID 21146444.
- ^ Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR (November 2004). "Physiological risk factors for falls in older people with lower limb arthritis". J. Rheumatol. 31 (11): 2272–9. PMID 15517643.
- ^ Penny P, Geere J, Smith TO (October 2013). "A systematic review investigating the efficacy of laterally wedged insoles for medial knee osteoarthritis". Rheumatol. Int. 33 (10): 2529–38. doi:10.1007/s00296-013-2760-x. PMID 23612781.
- ^ Parkes MJ, Maricar N, Lunt M, LaValley MP, Jones RK, Segal NA, Takahashi-Narita K, Felson DT (August 2013). "Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis". JAMA. 310 (7): 722–30. doi:10.1001/jama.2013.243229. PMC 4458141. PMID 23989797.
- ^ a b Duivenvoorden, T; Brouwer, RW; van Raaij, TM; Verhagen, AP; Verhaar, JA; Bierma-Zeinstra, SM (16 March 2015). "Braces and orthoses for treating osteoarthritis of the knee". The Cochrane Database of Systematic Reviews. 3: CD004020. doi:10.1002/14651858.CD004020.pub3. PMID 25773267.
- ^ Page CJ, Hinman RS, Bennell KL (2011). "Physiotherapy management of knee osteoarthritis". Int J Rheum Dis. 14 (2): 145–152. doi:10.1111/j.1756-185X.2011.01612.x. PMID 21518313.
- ^ "Osteoarthritis Lifestyle and home remedies". Diseases and Conditions. Mayo Clinic. Archived from the original on 2016-01-25.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Bartels, EM; Juhl, CB; Christensen, R; Hagen, KB; Danneskiold-Samsøe, B; Dagfinrud, H; Lund, H (23 March 2016). "Aquatic exercise for the treatment of knee and hip osteoarthritis". The Cochrane Database of Systematic Reviews. 3: CD005523. doi:10.1002/14651858.CD005523.pub3. PMID 27007113. Archived from the original on 14 April 2016. Retrieved 5 April 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Fransen, Marlene; McConnell, Sara; Harmer, Alison R.; Van der Esch, Martin; Simic, Milena; Bennell, Kim L. (2015-01-09). "Exercise for osteoarthritis of the knee". The Cochrane Database of Systematic Reviews. 1: CD004376. doi:10.1002/14651858.CD004376.pub3. ISSN 1469-493X. PMID 25569281.
- ^ a b c d Consumer Reports Health Best Buy Drugs (July 2013), "The Nonsteroidal Anti-Inflammatory Drugs: Treating Osteoarthritis and Pain. Comparing effectiveness, safety, and price.", NSAIDs, Yonkers, New York: Consumer Reports, archived from the original (PDF) on 22 February 2014, retrieved 12 February 2014
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P (September 2007). "OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence". Osteoarthr. Cartil. 15 (9): 981–1000. doi:10.1016/j.joca.2007.06.014. PMID 17719803.
- ^ Machado, GC; Maher, CG; Ferreira, PH; Pinheiro, MB; Lin, CW; Day, RO; McLachlan, AJ; Ferreira, ML (31 March 2015). "Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials". BMJ (Clinical research ed.). 350: h1225. doi:10.1136/bmj.h1225. PMC 4381278. PMID 25828856.
- ^ da Costa, BR; Reichenbach, S; Keller, N; Nartey, L; Wandel, S; Jüni, P; Trelle, S (21 May 2016). "Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis". Lancet. 387 (10033): 2093–105. doi:10.1016/s0140-6736(16)30002-2. PMID 26997557.
- ^ Chen YF, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, Taylor RS (April 2008). "Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation". Health Technol Assess. 12 (11): 1–278, iii. doi:10.3310/hta12110. PMID 18405470.
- ^ Wielage, RC; Myers, JA; Klein, RW; Happich, M (December 2013). "Cost-effectiveness analyses of osteoarthritis oral therapies: a systematic review". Applied Health Economics and Health Policy. 11 (6): 593–618. doi:10.1007/s40258-013-0061-x. PMID 24214160.
- ^ van Walsem, Anneloes; Pandhi, Shaloo; Nixon, Richard M.; Guyot, Patricia; Karabis, Andreas; Moore, R. Andrew (2015-01-01). "Relative benefit-risk comparing diclofenac to other traditional non-steroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors in patients with osteoarthritis or rheumatoid arthritis: a network meta-analysis". Arthritis Research & Therapy. 17: 66. doi:10.1186/s13075-015-0554-0. ISSN 1478-6354. PMC 4411793. PMID 25879879.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Derry, S; Conaghan, P; Da Silva, JA; Wiffen, PJ; Moore, RA (22 April 2016). "Topical NSAIDs for chronic musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews. 4: CD007400. doi:10.1002/14651858.CD007400.pub3. PMID 27103611.
- ^ Karabis, Andreas; Nikolakopoulos, Stavros; Pandhi, Shaloo; Papadimitropoulou, Katerina; Nixon, Richard; Chaves, Ricardo L.; Moore, R. Andrew (2016-01-01). "High correlation of VAS pain scores after 2 and 6 weeks of treatment with VAS pain scores at 12 weeks in randomised controlled trials in rheumatoid arthritis and osteoarthritis: meta-analysis and implications". Arthritis Research & Therapy. 18: 73. doi:10.1186/s13075-016-0972-7. ISSN 1478-6362. PMC 4818534. PMID 27036633.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ McAlindon, TE; Bannuru, RR; Sullivan, MC; Arden, NK; Berenbaum, F; Bierma-Zeinstra, SM; Hawker, GA; Henrotin, Y; Hunter, DJ; Kawaguchi, H; Kwoh, K; Lohmander, S; Rannou, F; Roos, EM; Underwood, M (March 2014). "OARSI guidelines for the non-surgical management of knee osteoarthritis". Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 22 (3): 363–88. doi:10.1016/j.joca.2014.01.003. PMID 24462672.
- ^ Hochberg, MC; Altman, RD; April, KT; Benkhalti, M; Guyatt, G; McGowan, J; Towheed, T; Welch, V; Wells, G; Tugwell, P; American College of, Rheumatology (April 2012). "American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee". Arthritis Care & Research. 64 (4): 465–74. doi:10.1002/acr.21596. PMID 22563589.
- ^ da Costa, BR; Nüesch, E; Kasteler, R; Husni, E; Welch, V; Rutjes, AW; Jüni, P (17 September 2014). "Oral or transdermal opioids for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews. 9: CD003115. doi:10.1002/14651858.CD003115.pub4. PMID 25229835.
- ^ Derry, Sheena; Conaghan, Philip; Da Silva, José António P; Wiffen, Philip J; Moore, R Andrew (22 April 2016). "Topical NSAIDs for chronic musculoskeletal pain in adults". Cochrane Database of Systematic Reviews. 4: CD007400. doi:10.1002/14651858.cd007400.pub3. PMID 27103611. Archived from the original on 1 September 2016. Retrieved 26 April 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ da Costa BR, Nüesch E, Kasteler R, Husni E, Welch V, Rutjes AW, Jüni P (2014). "Oral or transdermal opioids for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews. 9: CD003115. doi:10.1002/14651858.CD003115.pub4. PMID 25229835.
- ^ a b c d e f De Silva V, El-Metwally A, Ernst E, Lewith G, Macfarlane GJ (May 2011). "Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review". Rheumatology (Oxford). 50 (5): 911–20. doi:10.1093/rheumatology/keq379. PMID 21169345.
- ^ a b Cameron M, Gagnier JJ, Little CV, Parsons TJ, Blümle A, Chrubasik S (November 2009). "Evidence of effectiveness of herbal medicinal products in the treatment of arthritis. Part I: Osteoarthritis". Phytother Res. 23 (11): 1497–515. doi:10.1002/ptr.3007. PMID 19856319.
- ^ Altman R, Barkin RL (March 2009). "Topical therapy for osteoarthritis: clinical and pharmacologic perspectives". Postgrad Med. 121 (2): 139–47. doi:10.3810/pgm.2009.03.1986. PMID 19332972.
- ^ Arroll B, Goodyear-Smith F (April 2004). "Corticosteroid injections for osteoarthritis of the knee: meta-analysis". BMJ. 328 (7444): 869. doi:10.1136/bmj.38039.573970.7C. PMC 387479. PMID 15039276.
- ^ a b Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S (August 2012). "Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis". Annals of Internal Medicine. 157 (3): 180–91. doi:10.7326/0003-4819-157-3-201208070-00473. PMID 22868835.
- ^ Jevsevar, D; Donnelly, P; Brown, GA; Cummins, DS (16 December 2015). "Viscosupplementation for Osteoarthritis of the Knee: A Systematic Review of the Evidence". The Journal of Bone and Joint Surgery. American Volume. 97 (24): 2047–60. doi:10.2106/jbjs.n.00743. PMID 26677239.
- ^ Witteveen, AG; Hofstad, CJ; Kerkhoffs, GM (17 October 2015). "Hyaluronic acid and other conservative treatment options for osteoarthritis of the ankle". The Cochrane Database of Systematic Reviews. 10 (10): CD010643. doi:10.1002/14651858.CD010643.pub2. PMID 26475434.
It is unclear if there is a benefit or harm for HA as treatment for ankle OA
- ^ Khoshbin A, Leroux T, Wasserstein D, Marks P, Theodoropoulos J, Ogilvie-Harris D, Gandhi R, Takhar K, Lum G, Chahal J (December 2013). "The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesis". Arthroscopy. 29 (12): 2037–48. doi:10.1016/j.arthro.2013.09.006. PMID 24286802.
- ^ Rodriguez-Merchan, EC (September 2013). "Intraarticular Injections of Platelet-rich Plasma (PRP) in the Management of Knee Osteoarthritis". Archives of bone and joint surgery. 1 (1): 5–8. PMC 4151401. PMID 25207275.
- ^ Jüni, Peter; Hari, Roman; Rutjes, Anne W. S.; Fischer, Roland; Silletta, Maria G.; Reichenbach, Stephan; da Costa, Bruno R. (2015). "Intra-articular corticosteroid for knee osteoarthritis". The Cochrane Database of Systematic Reviews (10): CD005328. doi:10.1002/14651858.CD005328.pub3. ISSN 1469-493X. PMID 26490760. Archived from the original on 2016-01-06.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Wernecke, Chloe; Braun, Hillary J.; Dragoo, Jason L. (2015). "The Effect of Intra-articular Corticosteroids on Articular Cartilage". Orthopaedic Journal of Sports Medicine. 3 (5). doi:10.1177/2325967115581163. ISSN 2325-9671. PMC 4622344. PMID 26674652.
- ^ McAlindon, Timothy E.; LaValley, Michael P.; Harvey, William F.; Price, Lori Lyn; Driban, Jeffrey B.; Zhang, Ming; Ward, Robert J. (2017). "Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial". JAMA. 317 (19): 1967–1975. doi:10.1001/jama.2017.5283. ISSN 1538-3598. PMID 28510679.
- ^ Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG (December 2008). "Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review". Can J Surg. 51 (6): 428–36. PMC 2592576. PMID 19057730.
- ^ Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ (April 2012). "Knee replacement". Lancet. 379 (9823): 1331–40. doi:10.1016/S0140-6736(11)60752-6. PMID 22398175.
- ^ Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR (2013). "Predicting the cost-effectiveness of total hip and knee replacement: A health economic analysis". The bone & joint journal. 95-B (1): 115–21. doi:10.1302/0301-620X.95B1.29835. PMID 23307684.
- ^ Daigle ME, Weinstein AM, Katz JN, Losina E (2012). "The cost-effectiveness of total joint arthroplasty: A systematic review of published literature". Best practice & research. Clinical rheumatology. 26 (5): 649–58. doi:10.1016/j.berh.2012.07.013. PMC 3879923. PMID 23218429.
- ^ Hunziker EB, Lippuner K, Keel MJ, Shintani N (2015). "An educational review of cartilage repair: precepts & practice – myths & misconceptions – progress & prospects". Osteoarthritis Cartilage. 23 (3): 334–50. doi:10.1016/j.joca.2014.12.011. PMID 25534362.
- ^ Brouwer, RW; Huizinga, MR; Duivenvoorden, T; van Raaij, TM; Verhagen, AP; Bierma-Zeinstra, SM; Verhaar, JA (13 December 2014). "Osteotomy for treating knee osteoarthritis". The Cochrane Database of Systematic Reviews. 12 (12): CD004019. doi:10.1002/14651858.CD004019.pub4. PMID 25503775.
- ^ Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM (2014). "A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative". Seminars in arthritis and rheumatism. 43 (6): 701–12. doi:10.1016/j.semarthrit.2013.11.012. PMID 24387819.
- ^ Katz, JN; Brownlee, SA; Jones, MH (February 2014). "The role of arthroscopy in the management of knee osteoarthritis". Best practice & research. Clinical rheumatology. 28 (1): 143–56. doi:10.1016/j.berh.2014.01.008. PMC 4010873. PMID 24792949.
- ^ Thorlund, JB.; Juhl, CB.; Roos, EM.; Lohmander, LS. (2015). "Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms". BMJ. 350: h2747. doi:10.1136/bmj.h2747. PMC 4469973. PMID 26080045.
- ^ Burdett N, McNeil JD (Sep 2012). "Difficulties with assessing the benefit of glucosamine sulphate as a treatment for osteoarthritis". International Journal of Evidence-based Healthcare. 10 (3): 222–6. doi:10.1111/j.1744-1609.2012.00279.x. PMID 22925619.
- ^ Wandel S, Jüni P, Tendal B, Nüesch E, Villiger PM, Welton NJ, Reichenbach S, Trelle S (Sep 16, 2010). "Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis". BMJ (Clinical research ed.). 341: c4675. doi:10.1136/bmj.c4675. PMC 2941572. PMID 20847017.
- ^ Wu D, Huang Y, Gu Y, Fan W (Jun 2013). "Efficacies of different preparations of glucosamine for the treatment of osteoarthritis: a meta-analysis of randomised, double-blind, placebo-controlled trials". International Journal of Clinical Practice. 67 (6): 585–94. doi:10.1111/ijcp.12115. PMID 23679910.
- ^ Chou R, McDonagh MS, Nakamoto E, Griffin J (Oct 2011). "Analgesics for Osteoarthritis: An Update of the 2006 Comparative Effectiveness Review". PubMed Health, US National Library of Medicine. PMID 22091473. Archived from the original on 2013-03-10.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Miller KL, Clegg DO (February 2011). "Glucosamine and chondroitin sulfate". Rheumatic Diseases Clinics of North America. 37 (1): 103–18. doi:10.1016/j.rdc.2010.11.007. PMID 21220090.
The best current evidence suggests that the effect of these supplements, alone or in combination, on OA pain, function, and radiographic change is marginal at best.
- ^ Rovati LC, Girolami F, Persiani S (Jun 2012). "Crystalline glucosamine sulfate in the management of knee osteoarthritis: efficacy, safety, and pharmacokinetic properties". Therapeutic Advances in Musculoskeletal Disease. 4 (3): 167–80. doi:10.1177/1759720X12437753. PMC 3400104. PMID 22850875.
- ^ Gregory, PJ; Fellner, C (June 2014). "Dietary supplements as disease-modifying treatments in osteoarthritis: a critical appraisal". Pharmacy and Therapeutics. 39 (6): 436–52. PMC 4103717. PMID 25050057.
- ^ Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P (February 2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (PDF). Osteoarthr. Cartil. 16 (2): 137–62. doi:10.1016/j.joca.2007.12.013. PMID 18279766. Archived from the original (PDF) on July 21, 2011.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Henrotin Y, Mobasheri A, Marty M (Jan 30, 2012). "Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis?". Arthritis Research & Therapy. 14 (1): 201. doi:10.1186/ar3657. PMC 3392795. PMID 22293240.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Bruyère, Olivier; Cooper, Cyrus; Pelletier, Jean-Pierre; Branco, Jaime; Luisa Brandi, Maria; Guillemin, Francis; Hochberg, Marc C.; Kanis, John A.; Kvien, Tore K.; Martel-Pelletier, Johanne; Rizzoli, René; Silverman, Stuart; Reginster, Jean-Yves (December 2014). "An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: A report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO)". Seminars in Arthritis and Rheumatism. 44 (3): 253–263. doi:10.1016/j.semarthrit.2014.05.014.
- ^ Vangsness CT, Jr; Spiker, W; Erickson, J (January 2009). "A review of evidence-based medicine for glucosamine and chondroitin sulfate use in knee osteoarthritis". Arthroscopy. 25 (1): 86–94. doi:10.1016/j.arthro.2008.07.020. PMID 19111223.
- ^ Singh JA, Noorbaloochi S, MacDonald R, Maxwell LJ (2015). "Chondroitin for osteoarthritis". Cochrane Database Syst Rev. 1: CD005614. doi:10.1002/14651858.CD005614.pub2. PMC 4881293. PMID 25629804.
- ^ a b c d Cameron, M; Chrubasik, S (22 May 2014). "Oral herbal therapies for treating osteoarthritis". The Cochrane Database of Systematic Reviews. 5: CD002947. doi:10.1002/14651858.CD002947.pub2. PMC 4494689. PMID 24848732.
- ^ Christiansen, BA; Bhatti, S; Goudarzi, R; Emami, S (January 2015). "Management of Osteoarthritis with Avocado/Soybean Unsaponifiables". Cartilage. 6 (1): 30–44. doi:10.1177/1947603514554992. PMC 4303902. PMID 25621100.
- ^ "Piascledine" (PDF). Haute Autorité de santé. July 25, 2013. Archived from the original (PDF) on December 30, 2016.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) See [Piascledine HAS index page for Piascledine] - ^ Sanders, M; Grundmann, O (September 2011). "The use of glucosamine, devil's claw (Harpagophytum procumbens), and acupuncture as complementary and alternative treatments for osteoarthritis". Alternative medicine review : a journal of clinical therapeutic. 16 (3): 228–38. PMID 21951024.
- ^ Grover, AK; Samson, SE (5 January 2016). "Benefits of antioxidant supplements for knee osteoarthritis: rationale and reality". Nutrition journal. 15: 1. doi:10.1186/s12937-015-0115-z. PMC 4700773. PMID 26728196.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Ameye, LG; Chee, WS (2006). "Osteoarthritis and nutrition. From nutraceuticals to functional foods: a systematic review of the scientific evidence". Arthritis research & therapy. 8 (4): R127. doi:10.1186/ar2016. PMC 1779427. PMID 16859534.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lopez HL (May 2012). "Nutritional interventions to prevent and treat osteoarthritis. Part II: focus on micronutrients and supportive nutraceuticals". Physical Medicine and Rehabilitation. 4 (5 Suppl): S155–68. doi:10.1016/j.pmrj.2012.02.023. PMID 22632695.
- ^ a b Rosenbaum CC, O'Mathúna DP, Chavez M, Shields K (2010). "Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis". Altern Ther Health Med. 16 (2): 32–40. PMID 20232616.
- ^ Oe, M; Tashiro, T; Yoshida, H; Nishiyama, H; Masuda, Y; Maruyama, K; Koikeda, T; Maruya, R; Fukui, N (27 January 2016). "Oral hyaluronan relieves knee pain: a review". Nutrition journal. 15: 11. doi:10.1186/s12937-016-0128-2. PMC 4729158. PMID 26818459.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Hussain, Salman; Singh, Ambrish; Akhtar, Mohd; Najmi, Abul Kalam (18 April 2017). "Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials". Rheumatology International. doi:10.1007/s00296-017-3719-0.
- ^ Lin, X; Huang, K; Zhu, G; Huang, Z; Qin, A; Fan, S (21 September 2016). "The Effects of Acupuncture on Chronic Knee Pain Due to Osteoarthritis: A Meta-Analysis". The Journal of Bone and Joint Surgery. American Volume. 98 (18): 1578–85. doi:10.2106/jbjs.15.00620. PMID 27655986.
- ^ Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S, van der Windt DA, Berman BM, Bouter LM (2010). Manheimer E (ed.). "Acupuncture for peripheral joint osteoarthritis". Cochrane Database of Systematic Reviews (1): CD001977. doi:10.1002/14651858.CD001977.pub2. PMC 3169099. PMID 20091527.
- ^ Wang SM, Kain ZN, White PF (February 2008). "Acupuncture analgesia: II. Clinical considerations" (PDF). Anesthesia and Analgesia. 106 (2): 611–21, table of contents. doi:10.1213/ane.0b013e318160644d. PMID 18227323. Archived from the original (PDF) on 2016-12-27.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Rutjes AW, Nüesch E, Sterchi R, Kalichman L, Hendriks E, Osiri M, Brosseau L, Reichenbach S, Jüni P (2009). Rutjes AW (ed.). "Transcutaneous electrostimulation for osteoarthritis of the knee". Cochrane Database of Systematic Reviews (4): CD002823. doi:10.1002/14651858.CD002823.pub2. PMID 19821296. Archived from the original on 2016-12-27.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Brosseau, L; Welch, V; Wells, G; DeBie, R; Gam, A; Harman, K; Morin, M; Shea, B; Tugwell, P (2004). "Low level laser therapy (Classes I, II and III) for treating osteoarthritis". Cochrane Database of Systematic Reviews (3): CD002046. doi:10.1002/14651858.CD002046.pub2. PMID 15266461.
- ^ Bjordal, J; Johnson, M; Lopes-Martins, R; Bogen, B; Chow, R; Ljunggren, A (2007). "Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials". BMC Musculoskeletal Disorders. 8 (1): 51. doi:10.1186/1471-2474-8-51.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Verhagen, A. P.; Bierma-Zeinstra, S. M. A.; Boers, M.; Cardoso, J. R.; Lambeck, J.; de Bie, R. A.; de Vet, H. C. W. (2007-10-17). "Balneotherapy for osteoarthritis". The Cochrane Database of Systematic Reviews (4): CD006864. doi:10.1002/14651858.CD006864. ISSN 1469-493X. PMID 17943920.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 2009-11-11. Retrieved Nov 11, 2009.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c Cross, M; Smith, E; Hoy, D; Nolte, S; Ackerman, I; Fransen, M; Bridgett, L; Williams, S; Guillemin, F; Hill, C. L.; Laslett, L. L.; Jones, G; Cicuttini, F; Osborne, R; Vos, T; Buchbinder, R; Woolf, A; March, L (2014). "The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study". Annals of the Rheumatic Diseases. 73 (7): 1323–30. doi:10.1136/annrheumdis-2013-204763. PMID 24553908.
- ^ Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ^ "Table 9: Estimated prevalence of moderate and severe disability (millions) for leading disabling conditions by age, for high-income and low- and middle-income countries, 2004". The Global Burden of Disease: 2004 Update. Geneva: World Health Organization. 2008. p. 35. ISBN 978-92-4-156371-0.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Green GA (2001). "Understanding NSAIDs: from aspirin to COX-2". Clin Cornerstone. 3 (5): 50–60. doi:10.1016/S1098-3597(01)90069-9. PMID 11464731.
- ^ Pfuntner A., Wier L.M., Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011. HCUP Statistical Brief #162. September 2013. Agency for Healthcare Research and Quality, Rockville, Maryland."Archived copy". Archived from the original on 2016-03-04. Retrieved 2016-02-09.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ Torio CM, Andrews RM (August 2013). "National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011". HCUP Statistical Brief #160. Rockville, Maryland: Agency for Healthcare Research and Quality. Archived from the original on 2017-03-14.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Pfuntner, A; Wier, L. M.; Steiner, C (December 2013). "Costs for Hospital Stays in the United States, 2011: Statistical Brief #168". PMID 24455786.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Molnar, R. E. (2001). "Therapod Paleopathology: A Literature Survey". In Tanke, Darren H.; Carpenter, Kenneth; Skrepnick, Michael William (eds.). Mesozoic Vertebrate Life. Indiana University Press. pp. 337–63. ISBN 978-0-253-33907-2.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Wallace, Ian J.; Worthington, Steven; Felson, David T.; Jurmain, Robert D.; Wren, Kimberly T.; Maijanen, Heli; Woods, Robert J.; Lieberman, Daniel E. (2017-08-29). "Knee osteoarthritis has doubled in prevalence since the mid-20th century". Proceedings of the National Academy of Sciences of the United States of America. 114 (35): 9332–9336. doi:10.1073/pnas.1703856114. ISSN 0027-8424. PMC 5584421. PMID 28808025.
- ^ Devaraj TL (2011). "Chapter 41: Nature cure yoga for osteoarthritis". Nature Cure for Common Diseases. New Delhi: Arya Publication. p. 368. ISBN 978-8189093747.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Tanchev, Panayot (2017-04-17). "Osteoarthritis or Osteoarthrosis: Commentary on Misuse of Terms". Reconstructive Review. 7 (1). ISSN 2331-2270.
- ^ Civjan N (2012). Chemical Biology: Approaches to Drug Discovery and Development to Targeting Disease. John Wiley & Sons. p. 313. ISBN 9781118437674. Archived from the original on 2013-12-31.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Bruyère O, Burlet N, Delmas PD, Rizzoli R, Cooper C, Reginster JY (2008). "Evaluation of symptomatic slow-acting drugs in osteoarthritis using the GRADE system". BMC Musculoskelet Disord. 9: 165. doi:10.1186/1471-2474-9-165. PMC 2627841. PMID 19087296.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Chu, CR; Andriacchi, TP (2015). "Dance between biology, mechanics, and structure: a systems-based approach to developing osteoarthritis prevention strategies". J Orthop Res. 33 (7): 939–947. doi:10.1002/jor.22817. PMID 25639920.
- ^ T. Pap; J. Schedel; G. Pap; U. Moller-Ladner; R.E. Gay; S. Gay C. Guincamp (2000). "Gene therapy in osteoarthritis". Joint Bone Spine. 67 (6): 570–571. doi:10.1016/s1297-319x(00)00215-3. PMID 11195326.
- ^ Lee, K. H.; Song, S. U.; Hwang, T. S.; Yi, Y.; Oh, I. S.; Lee, J. Y.; Choi, K. B.; Choi, M. S.; Kim, S. J. (2001-09-20). "Regeneration of hyaline cartilage by cell-mediated gene therapy using transforming growth factor beta 1-producing fibroblasts". Human Gene Therapy. 12 (14): 1805–1813. doi:10.1089/104303401750476294. ISSN 1043-0342. PMID 11560773.
- ^ Noh, Moon Jong; Lee, Kwan Hee (2015-11-18). "Orthopedic cellular therapy: An overview with focus on clinical trials". World Journal of Orthopedics. 6 (10): 754–761. doi:10.5312/wjo.v6.i10.754. ISSN 2218-5836. PMC 4644862. PMID 26601056.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c "Korea OKs first cell gene therapy 'Invossa'". The Korea Herald. 2017-07-12. Retrieved 2017-11-23.
- ^ Kraus, VB; Blanco, FJ; Englund, M; Henrotin, Y; Lohmander, LS; Losina, E; Onnerfjord, P; Persiani, S (2015). "OARSI Clinical Trials Recommendations: Soluble biomarker assessments in clinical trials in osteoarthritis". Osteoarthritis Cartilage. 23 (5): 686–697. doi:10.1016/j.joca.2015.03.002. PMC 4430113. PMID 25952342.
- ^ Saberi Hosnijeh, F; Runhaar, J; van Meurs, JB; Bierma-Zeinstra, SM (2015). "Biomarkers for osteoarthritis: Can they be used for risk assessment? A systematic review". Maturitas. 82 (1): 36–49. doi:10.1016/j.maturitas.2015.04.004. PMID 25963100.
- ^ Nepple, JJ; Thomason, KM; An, TW; Harris-Hayes, M; Clohisy, JC (2015). "What is the utility of biomarkers for assessing the pathophysiology of hip osteoarthritis? A systematic review". Clin Orthop Relat Res. 473 (5): 1683–1701. doi:10.1007/s11999-015-4148-6. PMC 4385333. PMID 25623593.
- ^ Nguyen, Lich Thi; Sharma, Ashish Ranjan; Chakraborty, Chiranjib; Saibaba, Balaji; Ahn, Moo-Eob; Lee, Sang-Soo (2017-03-12). "Review of Prospects of Biological Fluid Biomarkers in Osteoarthritis". International Journal of Molecular Sciences. 18 (3). doi:10.3390/ijms18030601. ISSN 1422-0067. PMC 5372617. PMID 28287489.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kumahashi, N; Swärd, P; Larsson, S; Lohmander, LS; Frobell, R; Struglics, A (2015). "Type II collagen C2C epitope in human synovial fluid and serum after knee injury - associations with molecular and structural markers of injury". Osteoarthritis Cartilage. 23 (9): 1506–12. doi:10.1016/j.joca.2015.04.022. PMID 25937025.