Drinking

Drinking is the act of ingesting water or other drinks through the mouth. Water is required for many of life’s physiological processes. Both excessive and inadequate water intake are associated with health problems.
Physiology
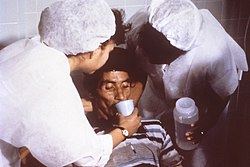
Human drinking
When a liquid is poured into an open human mouth, the swallowing process is completed by peristalsis which delivers the liquid to the stomach; much of the activity is abetted by gravity. The liquid may be poured from the hands or drinkware may be used as vessels. Drinking can also be performed by acts of inhalation, typically when imbibing hot liquids or drinking from a spoon. Infants employ a method of suction wherein the lips are pressed tight around a source, as in breastfeeding: a combination of breath and tongue movement creates a vacuum which draws in liquid.[1]
Land animals
To stay hydrated, most land animals drink their water, but the methods and motions differ greatly among species.[2] Cats, canines, and ruminants all lower the neck and lap in water with their powerful tongues. Most birds scoop or draw water into the buccal areas of their bills, raising and tilting their heads back to drink (an exception is the common pigeon which can suck in water directly by inhalation).[2]
Many desert animals do not drink even if water becomes available, but rely on eating succulent plants. Most amphibians do not drink at all, but slowly absorb water through direct skin contact.[2]
-
A Canada goose pulling water into its bill.
-
Sheep drinking at a watering hole.
-
Cats drink at a slower pace than ruminants, who face greater predation hazards in the wild.[2]
-
Uniquely, elephants draw water into their trunks and squirt it into their mouths.[2]
-
Drinking has been observed in many insect species.[2]
Thirst
The sensation caused by dehydration of the body is called thirst. The sensation of thirst is a dry feeling in the back of the throat and an intense desire to drink fluids. Thirst is regulated by the hypothalamus in response to subtle changes in the body's electrolyte levels, and also as a result of changes in the volume of blood circulating.
Human water requirements
A daily intake of water is required for the normal physiological functioning of the human body. The USDA recommends a daily minimum intake of 3.7 liters (appx. 1 gallon) of water per day for an adult male, and 2.7 liters (appx. 0.75 gallon) for an adult female.[3] For hydration in the human metabolism, water sources can include not only drinking water itself but all beverages, as well as high-moisture foods such as fruits and meats.[3]
Other sources claim that a high intake of fresh drinking water, separate and distinct from other sources of moisture, is necessary for good health — eight servings per day of 8 fluid ounces (1.8 liters, or 0.5 gallon) is the amount recommended by many nutritionists,[4] although scientific evaluations of this practice remain inconclusive.[5][6]
Polydipsia is the medical term for the desire to drink large quantities of water. It is often accompanied by polyuria and may be a symptom of Diabetes mellitus or Diabetes insipidus.[7]
Role in health
Much of the world's disease is caused by the lack of clean drinking water. Lack of water in diet will eventually cause death by hypernatremia and dehydration, particularly when sweating consumes much of the body water. Unclean and unsanitary water can contain many bacteria and parasites that would otherwise be absent in clean water. Studies show that in some developing countries more than half of the population does not have access to safe drinking water.
It is also possible to overhydrate, which sometimes happens with athletes who consume too much water, thereby diluting the concentration of salts in the body. Overconsumption of water can be a sign of disease and/or mental health problems(e.g. damage to the hypothalamus), as stated above.
Fluid restriction
Fluid restriction or water restriction occurs when a person intentionally abstains from drinking water (or other beverage for hydration), either partially or completely.
Partial fluid restriction can be used in medicine, but have the disadvantages of being difficult to maintain, and it is often ineffective.[8] Drugs causing increased diuresis (diuretics) is generally an alternative, and have less risk of causing decreased glomerular filtration rate through the kidneys and resultant decreased kidney function. Fluid restriction is occasionally a practice in management of heart failure. However, according to a review in 2009, there is apparently no evidence of benefit of fluid restriction in patients with clinically stable heart failure otherwise receiving optimal pharmacological treatment.[9] Rather, diuretics are preferred in heart failure, mainly ACE inhibitors, with substantial evidence of improving survival and quality of life in heart failure patients.[10][11] Theoretically, fluid restriction could also correct the electrolyte imbalance in hyponatremia, but again, diuretics, mainly vasopressin receptor antagonists, show better efficiency.[8] Nevertheless, in hyponatremia secondary to SIADH, long-term fluid restriction (of 1,200–1,800 mL/day) in addition to diuretics is standard treatment.[12]
Also, fluid restriction is the test of choice to distinguish primary polydipsia from diabetes insipidus. In primary polydipsia, the urine osmolality should increase and stabilize at above 280 Osm/kg with fluid restriction, while a stabilization at a lower level indicatess diabetes insipidus.[13] Stabilization in this test means, more specifically, when the hourly increase in osmolality is less than 30 Osm/kg per hour for at least 3 hours.[13]
Fluid restriction can also be part of religious practice, such as being part of the fasting from dawn till dusk in the Ramadan period for Muslims. During the daylight hours of Ramadan fasting, practising Muslims are dehydrating, but it is not clear whether this is chronic during the month of Ramadan.[14] No detrimental effects on health have as yet been directly attributed to negative water balance at the levels that may be produced during Ramadan.[14]
Also, patients with terminal illness may refuse both nutrition and hydration.[15]
Alcoholic beverages
“Drinking” is often used metonymically as a synonym for the consumption of alcoholic beverages. Most cultures throughout history have incorporated some number of the wide variety of "strong drinks" into their meals, celebrations, ceremonies, toasts and other occasions.[16] The earliest known evidence of fermented drinks in human culture dates to 8,000 BC.[17]
Despite its popularity, the drinking of alcohol poses significant health risks. Alcohol abuse and the addiction of alcoholism are common maladies worldwide. A high rate of consumption can also lead to cirrhosis, gastritis, gout, pancreatitis, hypertension and numerous other illnesses.[18]
-
An array of modern alcoholic beverages.
-
Beer drinking at Oktoberfest
-
Drinks raised in a traditional toast.
Drinking in art
-
Midnight Modern Conversation (William Hogarth, 1733): English gentlemen sharing alcoholic punch.
-
A 19th-century illustration of the young Rip Van Winkle having another drink (not water).
-
Boy with a Lute (Frans Hals, c.1625): a young musician "calling for a refill".[19]
-
Pouring from an amphora (illustration from The Rubaiyat of Omar Khayyam
See also
References
- ^ Flint, Austin (1875). The Physiology of Man. New York: D. Appleton and Co. pp. 137–138. OCLC 5357686. Retrieved 2 April 2012.
- ^ a b c d e f Broom, Donald M. (1981). Biology of Behaviour: Mechanisms, Functions and Applications. Cambridge: Cambridge University Press. p. 105. ISBN 0-521-29906-3. Retrieved 3 April 2012.
- ^ a b National Academy of Sciences. "Dietary Guidance". USDA Food and Nutrition Information Center. United States Department of Agriculture. Retrieved 2 April 2012.
Redirects to the NAS report, Dietary Reference Intakes: Electrolytes and Water (PDF)
{{cite web}}: External link in|quote= - ^ Greenhalgh, Alison (2001). "Healthy living – Water". BBC Health. BBC. Retrieved 2 April 2012.
- ^ Valtin, Heinz; Gorman, Sheila A. (2012). "Drink at least eight glasses of water a day: Really? Is there scientific evidence for "8 × 8"?". AJPregu.physiology.org. American Physiological Society. Retrieved 2 April 2012.
- ^ Negoianu, Dan; Goldfarb, Stanley (2008). "Just Add Water" (PDF). Journal of the American Society of Nephrology. 19 (6). ASN: 1041–1043. doi:10.1681/ASN.2008030274. PMID 18385417. Retrieved 2 April 2012.
- ^ Provan, Drew (2010). Oxford Handbook of Clinical and Laboratory Investigation. Oxford: Oxford University Press. p. 129. ISBN 0-19-923371-3. Retrieved 2 April 2012.
- ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1016/j.amjcard.2005.10.050, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1016/j.amjcard.2005.10.050instead. - ^ Tai MK (2009). "Evidence-based practice of fluid restriction in patients with heart failure". Hu Li Za Zhi (in Chinese). 56 (5): 23–9. PMID 19760574.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ The CONSENSUS Trial Study Group. (1987). "Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS)". N Engl J Med. 316 (23): 1429–35. doi:10.1056/NEJM198706043162301. PMID 2883575.
- ^ The SOLVD Investigators. (1991). "Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure". N Engl J Med. 325 (5): 293–302. doi:10.1056/NEJM199108013250501. PMID 2057034.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1007/978-3-540-79565-0_40, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1007/978-3-540-79565-0_40instead. - ^ a b Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1038/sj.ejcn.1601899, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1038/sj.ejcn.1601899instead. - ^ Patient Refusal of Nutrition and Hydration: Walking the Ever-Finer Line American Journal Hospice & Palliative Care, pp. 8–13, March/April 1995
- ^ Gately, Iain (2008). Drink: A Cultural History of Alcohol. New York: Penguin. pp. 1–14. ISBN 1-59240-464-2. Retrieved 2 April 2012.
- ^ Gately, p. 2.
- ^ Fiebach, Nicholas H., ed. (2007). Principles of Ambulatory Medicine. Lippincott Williams & Wilkins. p. 387. ISBN 0-7817-6227-8. Retrieved 2 April 2012.
- ^ Schjeldahl, Peter (8 August 2011). "Haarlem Shuffle: The Fast World of Frans Hals". The New Yorker. Condé Nast: 74–75. Retrieved 2 April 2012.(subscription required)



![Cats drink at a slower pace than ruminants, who face greater predation hazards in the wild.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/c/ce/Drinking_tiger.jpg/120px-Drinking_tiger.jpg)
![Uniquely, elephants draw water into their trunks and squirt it into their mouths.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/f/f9/Loxodonta_africana_-Roger_Williams_Park_Zoo%2C_USA-8a.jpg/80px-Loxodonta_africana_-Roger_Williams_Park_Zoo%2C_USA-8a.jpg)
![Drinking has been observed in many insect species.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3f/Drinking_Bee2.jpg/120px-Drinking_Bee2.jpg)






![Boy with a Lute (Frans Hals, c.1625): a young musician "calling for a refill".[19]](http://upload.wikimedia.org/wikipedia/commons/thumb/b/be/Frans_Hals_001.png/98px-Frans_Hals_001.png)
