Rhizomelic chondrodysplasia punctata
| Rhizomelic chondrodysplasia punctata | |
|---|---|
 | |
| Low levels of plasmalogens is a characteristic of rhizomelic chondrodysplasia punctata. | |
| Specialty | Medical genetics |
| Symptoms | Alopecia, flat face[1] |
| Causes | PEX7 gene, GNPAT gene and AGPS gene mutations[2] |
| Diagnostic method | Clinical and radiologic finding[3] |
| Treatment | Physical therapy[4] |
Rhizomelic chondrodysplasia punctata is a rare developmental brain disorder characterized by abnormally short arms and legs (rhizomelia), seizures, recurrent respiratory tract infections and congenital cataracts.
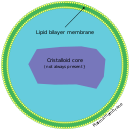
The cause is a genetic mutation that results in low levels of plasmalogens, which are a type of lipid found in cell membranes throughout the body, but whose function is not known.[2]
Signs and symptoms[edit]
Rhizomelic chondrodysplasia punctata has the following symptoms:[4][1]
- Bilateral shortening of the femur, resulting in short legs
- Post-natal growth problems (deficiency)
- Cataracts
- Intellectual disability
- Possible seizures
- Possible infections of respiratory tract
Genetics[edit]
This condition is a consequence of mutations in the PEX7 gene, the GNPAT gene (which is located on chromosome 1) or the AGPS gene. The condition is acquired in an autosomal recessive manner.[2]
Pathophysiology[edit]

The mechanism of rhizomelic chondrodysplasia punctata in the case of type 1 of this condition involves a defect in PEX7, whose product is involved in peroxisome assembly. There are 3 pathways that depend on peroxisomal biogenesis factor 7 activities, including:[4][5][verification needed]
- AGPS (catalyzes plasmalogen biosynthesis)
- PhYH (catalyzes catabolism of phytanic acid)
- ACAA1 (catalyzes beta-oxidation of VLCFA - straight)
Diagnosis[edit]
The diagnosis of rhizomelic chondrodysplasia punctata can be based on genetic testing[6] as well as radiography results, plus a physical examination of the individual.[3]
Types[edit]
- Type 1 (RCDP1) is associated with PEX7 mutations; these are peroxisome biogenesis disorders where proper assembly of peroxisomes is impaired.[4]
- Type 2 (RCDP2) is associated with DHAPAT mutations.[7]
- Type 3 (RCDP3) is associated with AGPS mutations.[8]
Treatment[edit]
Management of rhizomelic chondrodysplasia punctata can include physical therapy; additionally orthopedic procedures improved function sometimes in affected people.[4]
Prognosis[edit]
The prognosis is poor in this condition,[3] and most children die before the age of 10.[4] However, some survive to adulthood, especially if they have a non-classical (mild) form of RCDP.[4]
Children with classical, or severe, RCDP1 have severe developmental disabilities. Most of them achieve early developmental skills, such as smiling, but they will not develop skills expected from a baby older than six months (such as feeding themselves or walking).[4] By contrast, children with non-classical mild RCDP1 often learn to walk and talk.[4]
See also[edit]
References[edit]
- ^ a b "Rhizomelic chondrodysplasia punctata type 1". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. US National Library of Medicine. Retrieved 23 January 2017.
- ^ a b c Reference, Genetics Home. "rhizomelic chondrodysplasia punctata". Genetics Home Reference. Retrieved 2017-01-16.
- ^ a b c "Rhizomelic chondrodysplasia punctata". Orphanet. Retrieved 23 January 2017.
- ^ a b c d e f g h i Braverman, Nancy E.; Moser, Ann B.; Steinberg, Steven J. (2020). "Rhizomelic Chondrodysplasia Punctata Type 1". GeneReviews. PMID 20301447. NBK1270.
- ^ Brodsky, Michael C. (2016-06-28). Pediatric Neuro-Ophthalmology. Springer. p. 620. ISBN 9781493933846.
- ^ "Rhizomelic chondrodysplasia punctata type 1". Genetics Testing Laboratory (GTR): Conditions. US National Library of Medicine. Retrieved 23 January 2017.
- ^ Online Mendelian Inheritance in Man (OMIM): Rhizomelic Chondrodysplasia Punctata, Type 2; RCDP2 - 222765
- ^ Online Mendelian Inheritance in Man (OMIM): Rhizomelic Chondrodysplasia Punctata, Type 3; RCDP3 - 600121
Further reading[edit]
- Benacerraf, Beryl (2007). Ultrasound of fetal syndromes (2nd ed.). Philadelphia: Churchill Livingstone / Elsevier. ISBN 978-0443066412. Retrieved 23 January 2017.
- Ashwal, Stephen; Ferriero, Donna M.; Schor, Nina F. (2012). Swaiman, Kenneth F. (ed.). Swaiman's pediatric neurology principles and practice (5th ed.). [Edinburgh]: Elsevier Saunders. ISBN 978-0323089111. Retrieved 23 January 2017.
- Braverman NE, Steinberg SJ, Fallatah W, et al. (2020). Adam MP, Ardinger HH, Pagon RA, et al. (eds.). "Rhizomelic Chondrodysplasia Punctata Type 1". GeneReviews® [Internet]. University of Washington. PMID 20301447. NBK1270.
- Braverman NE, Bober MB, Brunetti-Pierri N, et al. (2020). Adam MP, Ardinger HH, Pagon RA, et al. (eds.). "Chondrodysplasia Punctata 1, X-Linked". GeneReviews® [Internet]. University of Washington. PMID 20301713.
- Kumble S, Savarirayan R (2020). Adam MP, Ardinger HH, Pagon RA, et al. (eds.). "Chondrodysplasia Punctata 2, X-Linked". GeneReviews® [Internet]. University of Washington. PMID 21634086. NBK55062.
