MDMA
 | |
| Clinical data | |
|---|---|
| Other names | (±)-1,3-benzodioxolyl-N-methyl-2-propanamine; (±)-3,4-methylenedioxy-N-methyl-α-methyl-2-phenethylamine; DL-3,4-methylenedioxy-N-methamphetamine; methylenedioxymethamphetamine |
| Pregnancy category |
|
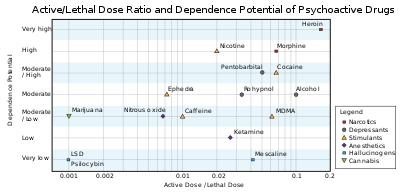
| Dependence liability | Moderate |
| Routes of administration | Oral, sublingual, insufflation, inhalation (vaporization), injection,[2] rectal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Hepatic, CYP450 extensively involved, especially CYP2D6 |
| Elimination half-life | 6–10 hours (though duration of effects is typically actually 3–5 hours)[citation needed] |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
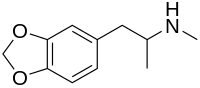
| Formula | C11H15NO2 |
| Molar mass | 193.24 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
MDMA (3,4-methylenedioxy-N-methylamphetamine) is an empathogenic drug of the phenethylamine and amphetamine classes of drugs. MDMA has become widely known as "ecstasy" (shortened to "E", "X", or "XTC"), usually referring to its street form, although this term may also include the presence of possible adulterants. The UK term "Mandy" and the US term "Molly" colloquially refer to MDMA that is relatively free of adulterants.[3]
MDMA can induce euphoria, a sense of intimacy with others, diminished anxiety, and mild psychedelia. Many studies, particularly in the fields of psychology and cognitive therapy, have suggested MDMA has therapeutic benefits and facilitates therapy sessions in certain individuals, a practice for which it had been formally used in the past. Clinical trials are now testing the therapeutic potential of MDMA for post-traumatic stress disorder, anxiety associated with terminal cancer[4][5] and addiction.[6]
MDMA is criminalized in most countries. Some limited exceptions exist for scientific and medical research. For 2008, the UN estimated between 10 and 25 million people globally used MDMA at least once in the past year. This was broadly similar to the number of cocaine, amphetamine, and opioid users, but far fewer than the global number of cannabis users.[7] It is taken in a variety of contexts far removed from its roots in psychotherapeutic settings, and is commonly associated with dance parties (or "raves") and electronic dance music.[8]
Regulatory authorities in several locations around the world have approved scientific studies administering MDMA to humans to examine its therapeutic potential and its effects.[9]
Medical use
MDMA has been indicated as possibly useful in psychotherapy, facilitating self-examination with reduced fear.[10][11][12] Indeed, some therapists, including Leo Zeff, Claudio Naranjo, George Greer, Joseph Downing, and Philip Wolfson, used MDMA in their practices until it was made illegal. George Greer synthesized MDMA in the lab of Alexander Shulgin and administered it to about 80 of his clients over the course of the remaining years preceding MDMA's Schedule I placement in 1985. In a published summary of the effects,[13] the authors reported patients felt improved in various mild psychiatric disorders and experienced other personal benefits, especially improved intimate communication with their significant others. In a subsequent publication on the treatment method, the authors reported one patient with severe pain from terminal cancer experienced lasting pain relief and improved quality of life.[14] In the United States, no research on MDMA was allowed at all, from 1985 until 1992, when the FDA approved Dr. Charles Grob to conduct human studies.[15]
In the year 2000, Doctor Jose Carlos Bouso performed the first clinical trial of MDMA for use in treating Post Traumatic Stress Disorder.[16] Since 2009, two randomized, controlled trials of MDMA-assisted psychotherapy for post-traumatic stress disorder were published. The positive effects were so large as to achieve statistical significance in spite of the small size of the trials (In one study, the rate of clinical response was 10/12 (83%) in the active treatment group versus 2/8 (25%) in the placebo group. In the other study, a p-score of 1.4% was found for the PDS scale and 1.6% for the CAP scale one year after treatment. A p-score of 5% or less is often considered statistically significant, and the effect found needs to be larger with smaller studies to have statistical significance, ceteris paribus, in order to correct for sample size.) In the second study, positive effect in CAP scale immediately after treatment did not achieve statistical significance (p=6.6%), but may do so with a larger sample size. The patients treated with two or three sessions of MDMA-psychotherapy showed greater improvement than the ones treated by placebo-psychotherapy[17] or placebo-inactive dose of MDMA.[18] This improvement was generally maintained on a follow-up several years later.[19]
Recreational use

Small doses of MDMA are used as an entheogen to enhance prayer or meditation by some religious practitioners.[20]
MDMA is often considered the drug of choice within the rave culture and is also used at clubs, festivals and house parties. In the rave environment, the sensorial effects from the music and setup such as lasers are often highly synergistic with the drug. The psychedelic amphetamine quality of MDMA lends it to variable reasons as to why it appeals to users in the "rave" setting. Some users enjoy the feeling of mass communion from the inhibition-depressing effects of the drug, while others use it as party fuel because of the drug's stimulatory effects.[21]
MDMA is occasionally known for being taken in conjunction with psychedelic drugs, such as LSD or psilocybin mushrooms, or even common drugs such as cannabis. As this practice has become more prevalent, most of the more common combinations have been given nicknames, such as “candy flipping” for MDMA combined with LSD, “hippy flipping” for MDMA with psilocybin mushrooms, or “kitty flipping” for MDMA with ketamine.[22] The term “flipping” may come from the subjective effects of using MDMA with a psychedelic in which the user may shift rapidly between a more lucid state and a more psychedelic state several times during the course of their experiences. Many users use mentholated products while taking MDMA for its cooling sensation while experiencing the drug’s effects. Examples include menthol cigarettes, Vicks VapoRub, NyQuil,[23] and lozenges.
Subjective effects
The primary effects attributable to MDMA consumption are predictable and fairly consistent among users. In general, users begin reporting subjective effects within 30 to 60 minutes of consumption, hitting a peak at about 75 to 120 minutes which plateaus coherently for about 3.5 hours.[24] Users note peak serotonin occurs from 2.5-3 hours after ingestion. This is followed by a comedown of a few hours, which has been described as a deficit of serotonin, fatigue accompanied by noticeable toxicity in the jaw which manifests as clenching or trembling, and difficulty sleeping or insomnia.
The following subjective effects of MDMA were statistically significant in a placebo-controlled trial, using Altered States of Consciousness rating scale: derealization, depersonalization, altered perception of space and time, positive basic mood, mania-like experience, anxious derealization, thought disorder, fears of loss of thought or body control, visual hallucinations or pseudo-hallucinations, synesthesia, changed meaning of percepts, facilitated recollection or imagination. On an Adjective Mood rating scale, the following measurements were significantly increased: self-confidence, heightened mood, apprehension-anxiety, thoughtfulness-contemplativeness, extroversion, dazed state, sensitivity, and emotional excitation.[24]
Adverse effects
In January 2001, an overview of the subjective side effects of MDMA was based on clinical research conducted over several years involving 74 healthy volunteers. The researchers found a number of common side effects, and many of the effects seemed to occur in different amounts based on the sex of the user. The top side effects reported were difficulty concentrating, jaw clenching/grinding of the teeth during sleep, lack of appetite, and dry mouth/thirst (all occurring in more than 50% of the 74 volunteers). They also measured some of the test subjects for blood pressure, heart rate, and body temperature against a placebo control, but no statistically significant changes were seen.[24][25]
It has also been found that MDMA has anti-inflammatory effects in the periphery, which includes inhibitory effects on T cell proliferation, cytokine production (including TNF-α, IL-1β, IL-12 and IL-15) and levels of circulating lymphocytes and natural killer cells in the blood.[26]
A 2008 study by Johns Hopkins Medical School found a slight but significant correlation of cognitive deficiency in MDMA users, but admitted these data may be confounded by other illicit drug use. The significant finding of the article was the serotonergic neurotoxicity in stacked doses and a lasting serotonin reuptake inhibition (SERT). At high doses and in high temperatures, in rats, serotonergic neurotoxicity is limited, but dopaminergic neurotoxicity occurs. However, rats may not be a generalizable model for human neurotoxicity studies.[27]
A 2010 study found EEG measured brain activity believed to confirm neurotoxicity to serotonergic neurotransmission systems, and noted that the recorded brain activity data were "in line with the observation of attentional and memory impairments in Ecstasy users with moderate to high misuse".[28]
However, a 2011 study found no signs of cognitive impairment due to MDMA use, nor a decrease in any mental ability. The report also raised concerns that previous methods used to conduct research on the drug chose subjects not consistent with the general population, such as previous substance abusers, and therefore not necessarily average cognitive function, and thereby overstated the cognitive differences between users and nonusers.[29]
After-effects
Effects reported by some users once the acute effects of MDMA have worn off include:
- Psychological
- Physiological
A slang term given to the depressive period following MDMA consumption is Tuesday Blues (or "Suicide Tuesday"), referring to the low mood that can be experienced by midweek from depleted serotonin levels following MDMA use on the previous Friday or Saturday when raves or dance concerts were frequently scheduled. Some users reported consuming 5-HTP, L-tryptophan and vitamins the day after use can reduce the depressive effect by replenishing serotonin levels (magnesium supplements are also used prior to or during use, in an attempt to prevent jaw/muscle clenching).[36]
Overdose
Upon overdose, the potentially serious serotonin syndrome, stimulant psychosis, and/or hypertensive crisis, among other dangerous adverse reactions, may come to prominence, the symptoms of which can include:
- Psychological
- Disorientation and/or confusion
- Agitation,[38][39] restlessness[39] and paranoia[38]
- Hallucinations[31][38][39] and/or delusions[40]
- Thought disorder or disorganized thinking
- Cognitive and memory impairment potentially to the point of retrograde or anterograde amnesia[41]
- Physiological
- Muscle rigidity[39]
- Convulsions[38]
- Hyperreflexia or overresponsive or overreactive reflexes[42]
- Hyperactivity[38]
- Hypertension[38][39] or hypotension[39]
- Tachycardia[39]
- Tachypnoea or rapid breathing and/or dyspnea or shortness of breath
- Palpitations[39]
- Angina pectoris or severe chest pain, as well as pulmonary hypertension (PH)[43]
- Vasculitis or destruction of blood vessels[44]
- Cardiotoxicity or damage to the heart[45]
- Cardiac dysfunction, arrest, myocardial infarction, and/or heart failure[46][47][48]
- Hemorrhage and/or stroke[49][50]
- Severe hyperthermia, potentially resulting in organ failure[51][52]
- Loss of consciousness[53]
- Renal failure[39]
- Coma[38] or death[53]
Chronic use

Some studies indicate repeated recreational users of MDMA have increased rates of depression and anxiety, even after quitting the drug.[55][56][57] Other meta analyses have reported possibility of impairment of executive functioning.[58] Despite these findings, many factors, including total lifetime MDMA consumption, the duration of abstinence between uses, dosage, the environment of use, multiple drug use/abuse, quality of mental health, various lifestyle choices, and predispositions to develop clinical depression and other disorders, have made the results of many studies difficult to verify. A study that attempted to eliminate these confounding factors found few differences in the cognitive functioning of MDMA-using ravers versus non-MDMA-using ravers, "In a study designed to minimize limitations found in many prior investigations, we failed to demonstrate marked residual cognitive effects in ecstasy users. This finding contrasts with many previous findings -- including our own -- and emphasizes the need for continued caution in interpreting field studies of cognitive function in illicit ecstasy users."[59] MDMA use has been occasionally associated with liver damage,[60] excessive wear of teeth,[61] and (very rarely) hallucinogen persisting perception disorder.[62]
Short-term health concerns
Short-term physical health risks of MDMA consumption include dehydration [1], insomnia, hyperthermia,[63][64] and hyponatremia.[65] Continuous activity without sufficient rest or rehydration may cause body temperature to rise to dangerous levels, and loss of fluid via excessive perspiration puts the body at further risk as the stimulatory and euphoric qualities of the drug may render the user oblivious to their energy expenditure for quite some time. Diuretics such as alcohol may exacerbate these risks further.[citation needed]
Long-term effects on serotonin and dopamine
MDMA causes a reduction in the reuptake concentration of serotonin transporters in the brain. The rate at which the brain recovers from serotonergic changes is unclear. One study demonstrated lasting serotonergic changes in some animals exposed to MDMA.[66] Other studies have suggested that the brain may recover from serotonergic damage.[67][68]
Some studies suggest MDMA has a direct neurotoxicity in humans.[69][70] While other studies conclude MDMA mediates the toxicity of serotonin. Anecdotal user reports allude to a significant reduction in perceptible toxicity with coadministration of an equivalent amount of 5htp while coadministration with catecholamines increases the sensations of muscular vibration and jaw clenching. For more information on small amine uptake into post synaptic vestules see Cheese_effect#Physical_effects_and_pharmacology. Still other studies, however, suggest potential brain damage may be partially reversible following prolonged abstinence from MDMA.[68][71] Depression and deficits in memory have been shown to occur more frequently in long-term MDMA users.[72][73] However, some recent studies have suggested MDMA use may not be associated with chronic depression.[74][75]
One study on MDMA toxicity, by George A. Ricaurte of Johns Hopkins School of Medicine, which claimed a single recreational dose of MDMA could cause Parkinson's disease in later life due to severe dopaminergic stress, was actually retracted by Ricaurte himself after he discovered his lab had administered not MDMA but methamphetamine, which is known to cause dopaminergic changes similar to the serotonergic changes caused by MDMA.[76] Ricaurte blamed this mistake on a labeling error by the chemical supply company that sold the material to his lab, but the supply company responded there was no evidence of a labeling error on their end. Most studies have found the levels of the dopamine transporter (or other markers of dopamine function) in MDMA users deserve further study or are normal.[77][78][79][80][81][82][83]
Several studies have indicated a possible mechanism for neurotoxicity of a metabolite of MDMA, through the reaction of alpha-methyldopamine, a principal metabolite, and glutathione, the major antioxidant in the human body. One possible product of this reaction, 2,5-bis-(glutathion-S-yl)-alpha-methyldopamine, has been demonstrated to produce the same toxic effects observed in MDMA, while MDMA, and alpha-methyldopamine themselves have been shown to be non-neurotoxic. It is, however, impossible to avoid the metabolism of MDMA in the body, and the production of this toxic metabolite.[84][85][86] Some studies have demonstrated possible ways to minimize the production of this particular metabolite, though evidence at this point is sparse at best.
Purity and dosage of "ecstasy"

Another concern associated with MDMA use is toxicity from chemicals other than MDMA in ecstasy tablets. Due to its near-universal illegality, the purity of a substance sold as ecstasy is unknown to the typical user. The MDMA content of tablets varies widely between regions and different brands of pills and fluctuates somewhat each year. Pills may contain other active substances meant to stimulate in a way similar to MDMA, such as amphetamine, mephedrone, methamphetamine, ephedrine, caffeine, all of which may be comparatively cheap to produce and can help to boost overall profits. In some cases, tablets sold as ecstasy do not even contain any MDMA. Pills may include a variety of non-psychoactive substances as well, such as paracetamol, ibuprofen, talcum powder, etc.[87]
A number of deaths have been attributed to para-methoxyamphetamine (PMA), a hallucinogenic amphetamine, being sold as ecstasy.[88][89] PMA is unique in its ability to quickly elevate body temperature and heart rate at relatively low doses, especially in comparison to MDMA. Hence, users believing they are consuming two 120-mg pills of MDMA could actually be consuming a dose of PMA that is potentially lethal, depending on the purity of the pill. Not only does PMA cause the release of serotonin, but it also acts as a monoamine oxidase inhibitor. When combined with an MDMA or an MDMA-like substance, serotonin syndrome can result.[90] Combining MAO inhibitors with certain legal prescription and over-the-counter medications can also lead to (potentially fatal) serotonin syndrome.
Harm assessment
The UK study placed great weight on the risk for acute physical harm, the propensity for physical and psychological dependency on the drug, and the negative familial and societal impacts of the drug. They did not evaluate or rate the negative impact of 'ecstasy' on the cognitive health of ecstasy users, e.g., impaired memory and concentration. Based on these factors, the study placed MDMA at number 18 in the list of 20 harmful drugs.[91]
David Nutt, a former chairman of the UK Advisory Council on the Misuse of Drugs, stated in the Journal of Psychopharmacology in January 2009, that 'ecstasy' use compared favorably with horse riding in terms of risk, with the drug leading to around 30 deaths a year in the UK compared to about 10 from horse riding, and "acute harm to person" occurring in about one in 10,000 episodes of 'ecstasy' use compared to about one in 350 episodes of horse riding.[92] Dr. Nutt noted the lack of a balanced risk assessment in public discussions of MDMA:[92]
The general public, especially the younger generation, are disillusioned with the lack of balanced political debate about drugs. This lack of rational debate can undermine the trust in government in relation to drug misuse and thereby undermining the government's message in public information campaigns. The media in general seem to have an interest in scare stories about illicit drugs, though there are some exceptions (Horizon, 2008).[93] A telling review of 10-year media reporting of drug deaths in Scotland illustrates the distorted media perspective very well (Forsyth, 2001).[94] During this decade, the likelihood of a newspaper reporting a death from paracetamol was in [sic] per 250 deaths, for diazepam it was 1 in 50, whereas for amphetamine it was 1 in 3 and for ecstasy every associated death was reported.
A spokesperson for the ACMD said, "The recent article by Professor David Nutt published in the Journal of Psychopharmacology was done in respect of his academic work and not as chair of the ACMD."[95]
The most carefully designed study so far,[59] compared the effect on cognitive skills in 52 'ecstasy' users against 59 very closely matched nonusers. The study eliminated potential confounding factors such as the use of other drugs and history of drug use. The study found no short- or long-term differences in cognitive skills in the test group (users) versus the control group (nonusers).
Drug interactions
A number of reported potentially dangerous possible interactions occur between MDMA and other drugs, including serotonergic drugs.[96] Several cases have been reported of death in individuals who ingested MDMA while taking ritonavir (Norvir), which inhibits multiple CYP450 enzymes. Toxicity or death has also been reported in people who took MDMA in combination with certain monoamine oxidase inhibitors, such as phenelzine (Nardil), tranylcypromine (Parnate), or moclobemide (Aurorix, Manerix).[97] Conversely, MAOB inhibitors such as selegiline (Deprenyl; Eldepryl, Zelapar, Emsam) do not seem to carry these risks when taken at selective doses, and have been used to completely block neurotoxicity in rats.[98]
Sassafras oil
Commercial sassafras oil generally is a byproduct of camphor production in Asia or comes from related trees in Brazil. Safrole is a precursor for the clandestine manufacture of MDMA, and as such, its transport is monitored internationally. Roots of Sassafras can also be steeped to make tea and were used in the flavoring of traditional root beer until being banned for mass production by the FDA. Laboratory animals that were given oral doses of sassafras tea or sassafras oil that contained large doses of safrole developed permanent liver damage or various types of cancer. In humans, liver damage can take years to develop, and it may not have obvious signs.[citation needed] While sassafras oil is an important ingredient in clandestine manufacture of MDMA, MDMA itself does not contain any sassafras oil.
Hormonal and in pregnancy
Babies of mothers who used MDMA during pregnancy may have delayed motor functions.[99] Mothers who used MDMA are more likely to give birth to boys, a phenomenon also reported in exposure to polybrominated biphenyls (PBB).[100] In saliva there is a 75% increase in the male sex hormone testosterone in both males and females after taking MDMA.[100]
Chemistry

Safrole, a colorless or slightly yellow oily liquid, extracted from the root-bark or the fruit of the sassafras tree is the primary precursor for all manufacture of MDMA. There are numerous synthetic methods available in the literature to convert safrole into MDMA via different intermediates.[101][102][103][104] One common route is via the MDP2P (3,4-methylenedioxyphenyl-2-propanone, also known as piperonyl acetone) intermediate, which can be produced in at least two different ways. One method is to isomerize safrole to isosafrole in the presence of a strong base, and then oxidize isosafrole to MDP2P. Another, reportedly better,[citation needed] method is to make use of the Wacker process to oxidize safrole directly to the MDP2P (3,4-methylenedioxy phenyl-2-propanone) intermediate. This can be done with a palladium catalyst. Once the MDP2P intermediate has been prepared, a reductive amination leads to MDMA, a racemate {1:1 mixture of (R)-1-(benzo[d][1,3]dioxol-5-yl)-N-methylpropan-2-amine and (S)-1-(benzo[d][1,3]dioxol-5-yl)-N-methylpropan-2-amine}. Another method for the synthesis of racemic MDMA is addition of hydrogen bromide to safrole and reaction of the adduct with methylamine. Safrole is not required for MDMA production, and other precursor chemicals are often used instead, for example piperonal.
Relatively small quantities of essential oil are required to make large amounts of MDMA. The essential oil of Ocotea cymbarum typically contains between 80 and 94% safrole. This would allow 500 ml of the oil, which retails at between $20 and $100, to be used to produce between 150 and 340 grams of MDMA.[105]
Pharmacology
MDMA acts as a releasing agent of serotonin, norepinephrine, and dopamine.[106] It enters neurons via carriage by the monoamine transporters.[106] Once inside, MDMA inhibits the vesicular monoamine transporter, which results in increased concentrations of serotonin, norepinephrine, and dopamine in the cytoplasm,[107] and induces their release by reversing their respective transporters through a process known as phosphorylation.[108]
MDMA has been identified as a potent agonist of TAAR1, a newly discovered GPCR important for regulation of monoaminergic systems in the brain.[109] Activation of TAAR1 increases cAMP production via adenylyl cyclase activation and inhibits transporter function.[109][110][111][112][113] These effects increase monoamine efflux and prolong the amount of time monoamines remain in the synapse. It also acts as a weak 5-HT1 and 5-HT2 receptor agonist, and its more efficacious metabolite MDA likely augments this action.[114][115][116][117]
MDMA's unusual entactogenic effects have been hypothesized to be, at least partly, the result of indirect oxytocin secretion via activation of the serotonin system.[118] Oxytocin is a hormone released following events such as hugging, orgasm, and childbirth, and is thought to facilitate bonding and the establishment of trust.[119] Based on studies in rats, MDMA is believed to cause the release of oxytocin, at least in part, by both directly and indirectly agonizing the serotonin 5-HT1A receptor. A placebo-controlled study in 15 human volunteers found 100 mg MDMA increased blood levels of oxytocin, and the amount of oxytocin increase was correlated with the subjective prosocial effects of MDMA.[120]
Three neurobiological mechanisms for the therapeutic effects of MDMA have been suggested: "1) MDMA increases oxytocin levels, which may strengthen the therapeutic alliance; 2) MDMA increases ventromedial prefrontal activity and decreases amygdala activity, which may improve emotional regulation and decrease avoidance, and 3) MDMA increases norepinephrine (NE) release and circulating cortisol levels, which may facilitate emotional engagement and enhance extinction of learned fear associations."[121]
Pharmacokinetics

MDMA reaches maximal concentrations in the blood stream between 1.5 and 3 hr after ingestion.[122] It is then slowly metabolized and excreted, with levels of MDMA and its metabolites decreasing to half their peak concentration over approximately 8 hours.[123] Thus, there are still high MDMA levels in the body when the experiential effects have mostly ended, indicating acute tolerance has developed to the actions of MDMA. Taking additional supplements of MDMA at this point, therefore, produces higher concentrations of MDMA in the blood and brain than might be expected based on the perceived effects.
Metabolites of MDMA that have been identified in humans include 3,4-methylenedioxyamphetamine (MDA), 4-hydroxy-3-methoxy-methamphetamine (HMMA), 4-hydroxy-3-methoxyamphetamine (HMA), 3,4-dihydroxyamphetamine (DHA) (also called alpha-methyldopamine (α-Me-DA)), 3,4-methylenedioxyphenylacetone (MDP2P), and 3,4-Methylenedioxy-N-hydroxyamphetamine (MDOH). The contributions of these metabolites to the psychoactive and toxic effects of MDMA are an area of active research. Sixty-five percent of MDMA is excreted unchanged in the urine (in addition, 7% is metabolized into MDA) during the 24 hours after ingestion.[124]
MDMA is known to be metabolized by two main metabolic pathways: (1) O-demethylenation followed by catechol-O-methyltransferase (COMT)-catalyzed methylation and/or glucuronide/sulfate conjugation; and (2) N-dealkylation, deamination, and oxidation to the corresponding benzoic acid derivatives conjugated with glycine. The metabolism may be primarily by cytochrome P450 (CYP450) enzymes (CYP2D6 (in humans, but CYP2D1 in mice), and CYP3A4) and COMT. Complex, nonlinear pharmacokinetics arise via autoinhibition of CYP2D6 and CYP2D8, resulting in zeroth order kinetics at higher doses. It is thought that this can result in sustained and higher concentrations of MDMA if the user takes consecutive doses of the drug.
Because the enzyme CYP2D6 is deficient or totally absent in some people,[125] it was once hypothesized that these people might have elevated risk when taking MDMA. However, there is still no evidence for this theory and available evidence argues against it.[126] It is now thought that the contribution of CYP2D6 to MDMA metabolism in humans is less than 30% of the metabolism. Indeed, an individual lacking CYP2D6 was given MDMA in a controlled clinical setting and a larger study gave MDMA to healthy volunteers after inhibiting CYP2D6 with paroxetine. Lack of the enzyme caused a modest increase in drug exposure and decreases in some metabolites, but physical effects did not appear appreciably elevated. While there is little or no evidence that low CYP2D6 activity increases risks from MDMA, it is likely that MDMA-induced CYP2D inhibition will increase risk of those prescription drugs that are metabolized by this enzyme. MDMA-induced CYP2D inhibition appears to last for up to a week after MDMA exposure.
MDMA and metabolites are primarily excreted as conjugates, such as sulfates and glucuronides.[127]

MDMA is a chiral compound and has been almost exclusively administered as a racemate. However, the two enantiomers have been shown to exhibit different kinetics. (S)-MDMA is more effective in eliciting 5-HT, NE, and DA release, while (D)-MDMA is overall less effective, and more selective for 5-HT and NE release (having only a very faint efficacy on DA release).[128] The disposition of MDMA may also be stereoselective, with the S-enantiomer having a shorter elimination half-life and greater excretion than the R-enantiomer. Evidence suggests[129] that the area under the blood plasma concentration versus time curve (AUC) was two to four times higher for the (R)-enantiomer than the (S)-enantiomer after a 40 mg oral dose in human volunteers. Likewise, the plasma half-life of (R)-MDMA was significantly longer than that of the (S)-enantiomer (5.8 ± 2.2 hours vs 3.6 ± 0.9 hours). However, because MDMA excretion and metabolism have nonlinear kinetics,[130] the half-lives would be higher at more typical doses (100 mg is sometimes considered a typical dose[122]). Given as the racemate MDMA has a half-life of around 8 hours.
Detection of use
MDMA and MDA may be quantitated in blood, plasma or urine to monitor for use, confirm a diagnosis of poisoning or assist in the forensic investigation of a traffic or other criminal violation or a sudden death. Some drug abuse screening programs rely on hair, saliva, or sweat as specimens. Most commercial amphetamine immunoassay screening tests cross-react significantly with MDMA or its major metabolites, but chromatographic techniques can easily distinguish and separately measure each of these substances. The concentrations of MDA in the blood or urine of a person who has taken only MDMA are, in general, less than 10% those of the parent drug.[131][132][133]
History
The examples and perspective in this section deal primarily with the United Kingdom and United States and do not represent a worldwide view of the subject. (July 2010) |
MDMA was first synthesized in 1912 by Merck chemist Anton Köllisch. At the time, Merck was interested in developing substances that stopped abnormal bleeding. Merck wanted to evade an existing patent, held by Bayer, for one such compound: hydrastinine. At the behest of his superiors Walther Beckh and Otto Wolfes, Köllisch developed a preparation of a hydrastinine analogue, methylhydrastinine. MDMA was an intermediate compound in the synthesis of methylhydrastinine, and Merck was not interested in its properties at the time.[134] On 24 December 1912, Merck filed two patent applications that described the synthesis of MDMA[135] and its subsequent conversion to methylhydrastinine.[136]
Merck records indicate that its researchers returned to the compound sporadically. In 1927, Max Oberlin studied the pharmacology of MDMA and observed that its effects on blood sugar and smooth muscles were similar to ephedrine's. Researchers at Merck conducted experiments with MDMA in 1952 and 1959.[134] In 1953 and 1954, the United States Army commissioned a study of toxicity and behavioral effects in animals of injected mescaline and several analogues, including MDMA. The Army experimented with MDMA as an interrogation tool in Project MKUltra.[137] These originally classified investigations were declassified and published in 1973.[138] MDMA was being used recreationally in the United States by 1970.[139] In the mid-1970s, Alexander Shulgin, then at University of California, Berkeley, heard from his students about unusual effects of MDMA; among others, the drug had helped one of them to overcome his stutter. Intrigued, Shulgin synthesized MDMA and tried it himself in 1976.[140] Two years later, he and David E. Nichols published the first report on the drug's psychotropic effect in humans. They described "altered state of consciousness with emotional and sensual overtones" that can be compared "to marijuana, and to psilocybin devoid of the hallucinatory component".[141]
Shulgin took to occasionally using MDMA for relaxation, referring to it as "my low-calorie martini", and giving the drug to his friends, researchers, and other people whom he thought could benefit from it. One such person was psychotherapist Leo Zeff, who had been known to use psychedelics in his practice. Zeff was so impressed with the effects of MDMA that he came out of his semi-retirement to proselytize for it. Over the following years, Zeff traveled around the U.S. and occasionally to Europe, training other psychotherapists in the use of MDMA.[140][142][143] Among underground psychotherapists, MDMA developed a reputation for enhancing communication during clinical sessions, reducing patients' psychological defenses, and increasing capacity for therapeutic introspection.[144]
In the early 1980s clubbers started using MDMA in Ibiza’s discos.[145] Subsequently, the drug emerged in the other parts of Europe and the United States. In the U.S., MDMA rose to prominence as "Adam" in trendy nightclubs and gay dance clubs in the Dallas area.[146] From there, use spread to raves in major cities around the country,[citation needed] and then to mainstream society. "Ecstasy" was recognized as slang for MDMA as early as June 1982.[147] The drug was first proposed for scheduling by the Drug Enforcement Administration (DEA) in July 1984[148] and was classified as a Schedule I controlled substance in the U.S. on 31 May 1985; on an emergency basis. No double blind studies had yet been conducted as to the efficacy of MDMA for psychotherapy.[149]
In the late 1980s, MDMA began to be widely used in the UK and other parts of Europe, becoming an integral element of rave culture and other psychedelic-influenced music scenes. Spreading along with rave culture, illicit MDMA use became increasingly widespread among young adults in universities and later in high schools. MDMA became one of the four most widely used illicit drugs in the U.S., along with cocaine, heroin, and cannabis.[150] According to some estimates as of 2004, only marijuana attracts more first time users in the U.S.[150]
After MDMA was criminalized, most medical use stopped, although some therapists continued to prescribe the drug illegally. Later Charles Grob initiated an ascending-dose safety study in healthy volunteers. Subsequent legally approved MDMA studies in humans have taken place in the U.S. in Detroit (Wayne State University), Chicago (University of Chicago), San Francisco (UCSF and California Pacific Medical Center), Baltimore (NIDA–NIH Intramural Program), and South Carolina, as well as in Switzerland (University Hospital of Psychiatry, Zürich), the Netherlands (Maastricht University), and Spain (Universitat Autònoma de Barcelona).[151]
In 2010, the BBC reported that use of MDMA had decreased in the UK in previous years. This is thought to be due to increased seizures and decreased production of the precursor chemicals used to manufacture MDMA. Unwitting substitution with other drugs, such as mephedrone and methamphetamine,[152] as well as legal alternatives to MDMA, such as BZP, MDPV, and methylone, are also thought to have contributed to its decrease in popularity.[153]
Legal status
MDMA is legally controlled in most of the world under the UN Convention on Psychotropic Substances and other international agreements, although exceptions exist for research and limited medical use. In general, the unlicensed use, sale or manufacture of MDMA are all criminal offences.
Australia
MDMA was declared illegal in Australia in 1986 because of its harmful effects and potential for abuse. It is classed as a Schedule 9 Prohibited Substance in the country, meaning it is available for scientific research purposes only. Any other type of sale, use or manufacture is strictly prohibited by law. Permits for research uses on humans must be approved by a recognized ethics committee on human research.
United Kingdom
MDMA was made illegal in 1977 by a modification order to the existing Misuse of Drugs Act 1971. Although MDMA was not named explicitly in this legislation, the order extended the definition of Class A drugs to include various ring-substituted phenethylamines,[154] thereby making it illegal to sell, buy, or possess the drug without a licence. Penalties include a maximum of seven years and/or unlimited fine for possession; life and/or unlimited fine for production or trafficking. See list of drugs illegal in the UK for more information. In February 2009 an official independent scientific advisory board to the UK government recommended that MDMA be re-classified to Class B, but this recommendation was immediately rejected by the government. This 2009 report on MDMA stated:[155]
The original classification of MDMA in 1977 under the Misuse of Drugs Act 1971 as a Class A drug was carried out before it had become widely used and with limited knowledge of its pharmacology and toxicology. Since then use has increased enormously, despite it being a Class A drug. As a consequence, there is now much more evidence on which to base future policy decisions.... Recommendation 1: A harm minimisation approach to the widespread use of MDMA should be continued.... Recommendation 6: MDMA should be re-classified as a Class B drug.
In 2000, the UK Police Foundation issued the Runciman Report, which reviewed the medical and social harms of MDMA and recommended: "Ecstasy and related compounds should be transferred from Class A to Class B."[156] In 2002, the Home Affairs Committee of the UK House of Commons, issued a report, The Government's Drugs Policy: Is it working?, which also recommended that MDMA should be reclassified to a Class B drug.[157] The UK government rejected both recommendations, saying that re-classification of MDMA would not be considered without a recommendation from the Advisory Council on the Misuse of Drugs, the official UK scientific advisory board on drug abuse issues.[158]
In February 2009, the UK Advisory Council on the Misuse of Drugs issued A review of MDMA ('ecstasy'), its harms and classification under the Misuse of Drugs Act 1971, which recommended that MDMA be re-classified in the UK from a class A drug to a class B drug.[155]
From the Discussion section of the ACMD report on MDMA:
Physical harms: (10.2) Use of MDMA is undoubtedly harmful. High doses may lead to death: by direct toxicity, in situations of hyperthermia/dehydration, excessive water intake, or for other reasons. However, fatalities are relatively low given its widespread use, and are substantially lower than those due to some other Class A drugs, particularly heroin and cocaine. Although it is no substitute for abstinence, the risks can be minimised by following advice such as drinking appropriate amounts of water (see Annex E). (10.3) Some people experience acute medical consequences as a result of MDMA use, which can lead to hospital admission, sometimes with the requirement for intensive care. MDMA poisonings are not currently increasing in number and are less frequent than episodes due to cocaine. (10.4) MDMA appears not to have a high propensity for dependence or withdrawal reactions, although a number of users seek help through treatment services. (10.5) MDMA appears to have little acute or enduring effect on the mental health of the average user, and, unlike amphetamines and cocaine, it is seldom implicated in significant episodes of paranoia. (10.6) There is at the present time little evidence of longer-term harms to the brain in terms of either its structure or its function. However, there is evidence for some small decline in a variety of domains, including verbal memory, even at low cumulative dose. The magnitude of such deficits appears to be small and their clinical relevance is unclear. The evidence shows that MDMA has been misused in the UK for 20 years, but it should be noted that long-term effects of use cannot be ruled out. (10.7) Overall, the ACMD judges that the physical harms of MDMA more closely equate with those of amphetamine than of heroin or cocaine.
Societal harms: (10.8) MDMA use seems to have few societal effects in terms of intoxication-related harms or social disorder. However, the ACMD notes the very small proportion of cases where ‘ecstasy’ use has been implicated in sexual assault. (10.9) Disinhibition and impulsive, violent or risky behaviours are not commonly seen under the influence of MDMA, unlike with cocaine, amphetamines, heroin and alcohol. (10.10) The major issue for law enforcement is ‘ecstasy's’ position, alongside other Class A drugs, as a commodity favoured by organised criminal groups. It is therefore generally associated with a range of secondary harms connected with the trafficking of illegal drugs.
The UK Home Office rejected the recommendation of its independent scientific advisory board to downgrade MDMA to Class B, "saying it is not prepared to send a message to young people that it takes ecstasy less seriously".[159][160]
The government's veto was criticized in scientific publications. Colin Blakemore, Professor of Neuroscience, Oxford, stated in the British Medical Journal, "The government's decisions compromise its commitment to evidence based policy".[161] Also in response, an editorial in the New Scientist noted "A much larger percentage of people suffer a fatal acute reaction to peanuts than to MDMA.... Sadly, perspective is something that is generally lacking in the long and tortuous debate over illegal drugs."[162]
United States
In the U.S., MDMA was legal and unregulated until 31 May 1985, at which time it was emergency scheduled to DEA Schedule I, for drugs deemed to have no medical uses and a high potential for abuse. During DEA hearings to schedule MDMA, most experts recommended DEA Schedule III prescription status for the drug, due to beneficial usage of MDMA in psychotherapy. The Administrative Law Judge (ALJ) overseeing the hearings, Francis Young, also recommended that MDMA be placed in Schedule III. The DEA however classified MDMA as Schedule I.[163][164] However, in Grinspoon v. Drug Enforcement Administration, 828 F.2d 881 (1st Cir. 1987), the First Circuit Court of Appeals remanded the scheduling determination for reconsideration by the DEA.[165] MDMA was temporarily removed from Schedule I.[166] Ultimately, in 1988, the DEA re-evaluated its position on remand and subsequently placed MDMA into Schedule I of the Controlled Substances Act.[167]
In a 2011 federal court hearing the American Civil Liberties Union successfully argued that the sentencing guideline for MDMA/ecstasy is based on outdated science, leading to excessive prison sentences.[168]
Netherlands
The Expert Committee on the List (Expertcommissie Lijstensystematiek Opiumwet) of the Netherlands issued a report in June 2011 which discussed the evidence for harm and the legal status of MDMA.[169] From the English-language summary:[170]
As regards MDMA, better known as XTC, the committee concludes that investigations show that damage to the health of the individual in the long term is less serious than was initially assumed. But the extent of the illegal production and involvement of organised crime leads to damage to society, including damage to the image of the Netherlands abroad. This argues in favour of maintaining MDMA on List I.
The Committee noted that research had found the health risks of MDMA were less serious than previously assumed (citing the 2009 UK ACMD report), and so they considered moving MDMA out of the Dutch List I ('hard drugs') to List II ('soft drugs' such as cannabis), but this was not acceptable because the criminal black market would continue to produce all the MDMA. Note, the Committee did not discuss permitting legally regulated production of MDMA for non-medical use because this is not allowed under the UN 1971 Convention on Psychotropic Substances (See Drug decriminalization vs. legalization).
Canada
Listed as a Schedule 1[171] as it is an analogue of amphetamine.[172] The CDSA was updated as a result of the Safe Streets Act changing amphetamines from Schedule 3 to Schedule 1 on March 2012.[173]
World Health Organization
In 1985 the World Health Organization's Expert Committee on Drug Dependence recommended that MDMA be placed in Schedule I of the 1971 Convention on Psychotropic Substances, despite noting:[174]
No data are available concerning its clinical abuse liability, nature and magnitude of associated public health or social problems.
The decision to recommend scheduling of MDMA was not unanimous:[174]
One member, Professor Paul Grof (Chairman), felt that the decision on the recommendation should be deferred awaiting, in particular, the data on the substance's potential therapeutic usefulness and that at this time international control is not warranted.
The 1971 Convention has a provision in Article 7(a) that allows use of Schedule I drugs for "scientific and very limited medical purposes." The committee's report stated:[174][175]
The Expert Committee held extensive discussions concerning therapeutic usefulness of 3,4 Methylenedioxymethamphetamine. While the Expert Committee found the reports intriguing, it felt that the studies lacked the appropriate methodological design necessary to ascertain the reliability of the observations. There was, however, sufficient interest expressed to recommend that investigations be encouraged to follow up these preliminary findings. To that end, the Expert Committee urged countries to use the provisions of article 7 of the Convention on Psychotropic Substances to facilitate research on this interesting substance.
Cost and distribution
The European Monitoring Centre for Drugs and Drug Addiction notes that, although there are some reports of tablets being sold for as little as €1, most countries in Europe now report typical retail prices in the range of €3 to €9 per tablet.[176] The United Nations Office on Drugs and Crime claimed in its 2008 World Drug Report that typical U.S. retail prices are US$20 to $25 per tablet, or from $3 to $10 per tablet if bought in batches.[177] A new research area named Drug Intelligence aims to automatically monitor distribution networks based on image processing and machine learning techniques, in which an Ecstasy pill picture is analyzed to detect correlations among different production batches.[178] These novel techniques allow police scientists to facilitate the monitoring of illicit distribution networks.
Australia
MDMA is particularly expensive in Australia, costing A$20–A$50 per tablet. In terms of purity data for Australian MDMA, the average is around 34%, ranging from less than 1% to about 85%. The majority of tablets contain 70–85 mg of MDMA. Most MDMA enters Australia from the Netherlands, the UK, Asia, and the U.S.[179]
References
- ^ Stimulants, Narcotics, Hallucinogens – Drugs, Pregnancy, and Lactation., Gerald G. Briggs, OB/GYN News, 1 June 2003.
- ^ "Methylenedioxymethamphetamine (MDMA, ecstasy)". Drugs and Human Performance Fact Sheets. National Highway Traffic Safety Administration.
- ^ PMID 22998806
- ^ Turner, Amy (4 May 2008). "Ecstasy is the key to treating PTSD". The Times. London. Retrieved 12 May 2010.
- ^ Ecstasy to be tested on terminal cancer patients, Associated Press, 28 December 2004
- ^ Jerome, Lisa (2013). "Can MDMA Play a Role in the Treatment of Substance Abuse?". Current Drug Abuse Reviews. 6 (1): 54–62. doi:10.2174/18744737112059990005. Retrieved 9 December 2013.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "World Drug Report 2010" (PDF). United Nations Office on Drugs and Crime. p. 15. Retrieved 27 February 2012.
- ^ World Health Organization (2004). Neuroscience of Psychoactive Substance Use and Dependence. World Health Organization. pp. 97–. ISBN 978-92-4-156235-5.
- ^ Psychedelic Research Worldwide. MAPS. Retrieved on 11 June 2011.
- ^ Greer G. and Tolbert R. (1989). "The Therapeutic Use of MDMA", pp. 21–36 in Ecstasy: The Clinical, Pharmacological, and Neurotoxicological Effects of the Drug MDMA, Peroutka, SJ (ed.) Springer, ISBN 0792303059.
- ^ Doblin R (2002). "A Clinical Plan for MDMA (Ecstasy) in the Treatment of Post-Traumatic Stress Disorder (PTSD): Partnering with the FDA" (PDF). J Psychoactive Drugs. 34 (2): 185–194. doi:10.1080/02791072.2002.10399952. PMID 12691208.
- ^ Sessa B, Nutt DJ (2007). "MDMA, Politics and Medical Research: Have We Thrown the Baby Out With the Bathwater?" (PDF). J. Psychopharmacol. (Oxford). 21 (8): 787–791. doi:10.1177/0269881107084738. PMID 17984158.
- ^ Greer, G.; Tolbert, R. (1986). "Subjective Reports of the Effects of MDMA in a Clinical Setting". Journal of Psychoactive Drugs. 18 (4): 319–327. doi:10.1080/02791072.1986.10472364. PMID 2880946.
{{cite journal}}: CS1 maint: multiple names: authors list (link) [dead link] - ^ Greer, G.; Tolbert, R. (1998). "A Method of Conducting Therapeutic Sessions with MDMA" (PDF). Journal of Psychoactive Drugs. 30 (4): 371–379. doi:10.1080/02791072.1998.10399713. PMID 9924843.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Julie Holland (2001). Ecstasy: The Complete Guide: A Comprehensive Look at the Risks and Benefits. p. 20.
- ^ Julie Holland (2001). Ecstasy: The Complete Guide: A Comprehensive Look at the Risks and Benefits. p. 391.
- ^ Mithoefer MC; Wagner MT; Mithoefer AT; Jerome I; Doblin R. (2009). "The safety and efficacy of {+/-}3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study" (PDF). Journal of Psychopharmachology. 25 (4): 439–52. doi:10.1177/0269881110378371. PMC 3122379. PMID 20643699.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23118021, please use {{cite journal}} with
|pmid=23118021instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23172889, please use {{cite journal}} with
|pmid=23172889instead. - ^ MDMA and Religion. CSP. Retrieved on 11 June 2011.
- ^ Reynolds, Simon (1999). Generation Ecstasy: Into the World of Techno and Rave Culture. Routledge. p. 81. ISBN 0415923735.
- ^ University of Maryland, College Park Center for Substance Abuse Research. "Ecstasy:CESAR".
- ^ "Director's Report to the National Advisory Council on Drug Abuse". National Institute on Drug Abuse. May 2000.[dead link]
- ^ a b c Liechti, ME; Gamma, A; Vollenweider, FX (2001). "Gender Differences in the Subjective Effects of MDMA". Psychopharmacology. 154 (2): 161–168. doi:10.1007/s002130000648. PMID 11314678.
- ^ Erowid (September 2001). Short-Term Side Effects of MDMA.
- ^ Boyle, NT (September 2010). "Methylenedioxymethamphetamine ('Ecstasy')-induced immunosuppression: a cause for concern?" (PDF). British Journal of Pharmacology. 161 (1): 17–32. doi:10.1111/j.1476-5381.2010.00722.x. PMC 2962814. PMID 20718737.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ McCann, U. D.; Szabo, Z.; Vranesic, M.; Palermo, M.; Mathews, W. B.; Ravert, H. T.; Dannals, Robert F.; Ricaurte, George A. (2008). "Positron emission tomographic studies of brain dopamine and serotonin transporters in abstinent 3,4-methylenedioxymethamphetamine ("ecstasy") users: relationship to cognitive performance". Psychopharmacology. 200 (3): 439–450. doi:10.1007/s00213-008-1218-4. PMC 2789420. PMID 18661256.
- ^ Adamaszek M, Khaw AV, Buck U, Andresen B, Thomasius R (2010) ''Evidence of Neurotoxicity of Ecstasy: Sustained Effects on Electroencephalographic Activity in Polydrug Users.'' ''PLoS ONE'' 5(11) e14097.
- ^ Halpern JH, Sherwood AR, Hudson JI, Gruber S, Kozin D, Pope HG (2011). "Residual neurocognitive features of long-term ecstasy users with minimal exposure to other drugs". Addiction. 106 (4): 777–86. doi:10.1111/j.1360-0443.2010.03252.x. PMC 3053129. PMID 21205042.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e "Ecstasy basics". betweenthelines.net.au. Retrieved 25 May 2010.
- ^ a b c d "Ecstasy: effects on the body". ydr.com.au. Retrieved 25 May 2010.
- ^ a b c "Ecstasy". betterhealth.vic.gov.au. Retrieved 25 May 2010.
- ^ a b c d e "MDMA Basics". erowid.org. Retrieved 25 May 2010.
- ^ Arrue A, Gomez FM, Giralt MT (April 2004). "Effects of 3,4-methylenedioxymethamphetamine ('Ecstasy') on the jaw-opening reflex". mdma.net. Retrieved 25 May 2010.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "What Is Bruxism?". bruxism.org.uk. Retrieved 25 May 2010.
- ^ Molly Flannagan, Ecstasy: Neurotoxicity and How It Can Be Reduced, 2001
- ^ "Drug Toxicity". Web.cgu.edu. Retrieved 17 February 2011.
- ^ a b c d e f g John; Gunn, Scott; Singer, Mervyn; Webb, Andrew Kellum. Oxford American Handbook of Critical Care. Oxford University Press (2007). ASIN: B002BJ4V1C. Page 464.
- ^ a b c d e f g h i Doweiko, Harold (2006). Concepts Of Chemical Dependency. Thomson; Benjamin Cummings. p. 211. ISBN 978-0495083696. Retrieved 12 December 2012.
- ^ Peroutka SJ, Newman H, Harris H (1988). "Subjective effects of 3,4-methylenedioxymethamphetamine in recreational users". Neuropsychopharmacology. 1 (4): 273–277. PMID 2908020.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chummun H, Tilley V, Ibe J (2010). "3,4-methylenedioxyamfetamine (ecstasy) use reduces cognition". Br J Nurs. 19 (2): 94–100. PMID 20235382.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ de la Torre R, Farré M, Roset PN, Pizarro N, Abanades S, Segura M; et al. (2004). "Human pharmacology of MDMA: pharmacokinetics, metabolism, and disposition". Ther Drug Monit. 26 (2): 137–144. doi:10.1097/00007691-200404000-00009. PMID 15228154.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Bassi S, Rittoo D (2005). "Ecstacy and chest pain due to coronary artery spasm". Int J Cardiol. 99 (3): 485–487. doi:10.1016/j.ijcard.2003.11.057. PMID 15771938.
- ^ Woodrow G, Turney JH (1999). "Ecstasy-induced renal vasculitis". Nephrol Dial Transplant. 14 (3): 798. doi:10.1093/ndt/14.3.798a.
- ^ Badon LA, Hicks A, Lord K, Ogden BA, Meleg-Smith S, Varner KJ (2002). "Changes in cardiovascular responsiveness and cardiotoxicity elicited during binge administration of Ecstasy". J Pharmacol Exp Ther. 302 (3): 898–907. doi:10.1124/jpet.302.3.898. PMID 12183645.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tiangco DA, Halcomb S, Lattanzio FA, Jr., Hargrave BY (2010). "3,4-Methylenedioxymethamphetamine alters left ventricular function and activates nuclear factor-kappa B (NF-kB) in a time and dose dependent manner". Int J Mol Sci. 11 (12): 4843–4863. doi:10.3390/ijms11124743. PMC 3100831. PMID 21614177.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Mende L, Böhm R, Regenthal R, Klein N, Grond S, Radke J (2005). "Cardiac arrest caused by an ecstasy intoxication". Anasthesiol Intensivmed Notfallmed Schmerzther. 40 (12): 762–765. doi:10.1055/s-2005-870500. PMID 16362878.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Qasim A, Townend J, Davies MK (2001). "Ecstasy induced acute myocardial infarction". Heart. 85 (6): E10. doi:10.1136/heart.85.6.e10. PMC 1729787. PMID 11359764.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Auer J, Berent R, Weber T, Lassnig E, Eber B (2002). "Subarachnoid haemorrhage with "Ecstasy" abuse in a young adult". Neurol Sci. 23 (4): 199–201. doi:10.1007/s100720200062. PMID 12536290.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Manchanda S, Connolly MJ (1993). "Cerebral infarction in association with Ecstasy abuse". Postgrad Med J. 69 (817): 874–875. doi:10.1136/pgmj.69.817.874. PMC 2399908. PMID 7904748.
- ^ Crean RD, Davis SA, Von Huben SN, Lay CC, Katner SN, Taffe MA (2006). "Effects of (+/-)3,4-methylenedioxymethamphetamine, (+/-)3,4-methylenedioxyamphetamine and methamphetamine on temperature and activity in rhesus macaques". Neuroscience. 142 (2): 515–525. doi:10.1016/j.neuroscience.2006.06.033. PMC 1853374. PMID 16876329.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sharma HS, Ali SF (2008). "Acute administration of 3,4-methylenedioxymethamphetamine induces profound hyperthermia, blood–brain barrier disruption, brain edema formation, and cell injury". Ann N Y Acad Sci. 1139: 242–258. doi:10.1196/annals.1432.052. PMID 18991870.
- ^ a b Caroline, Nancy (2010). Nancy Caroline's Emergency Care In The Streets. Jones & Bartlett Learning. ISBN 978-0763781729. Retrieved 12 December 2012.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17382831, please use {{cite journal}} with
|pmid=17382831instead. - ^ Verheyden SL, Henry JA, Curran HV (2003). "Acute, sub-acute and long-term subjective consequences of 'ecstasy' (MDMA) consumption in 430 regular users". Hum Psychopharmacol. 18 (7): 507–17. doi:10.1002/hup.529. PMID 14533132.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Verheyden SL, Maidment R, Curran HV (2003). "Quitting ecstasy: an investigation of why people stop taking the drug and their subsequent mental health". J. Psychopharmacol. (Oxford). 17 (4): 371–8. doi:10.1177/0269881103174014. PMID 14870948.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Laws KR, Kokkalis J (2007). "Ecstasy (MDMA) and memory function: a meta-analytic update". Human Psychopharmacology: Clinical and Experimental. 22 (6): 381–88. doi:10.1002/hup.857.
- ^ Rodgers J, Buchanan T, Scholey AB, Heffernan TM, Ling J, Parrott AC (2003). "Patterns of drug use and the influence of gender on self-reports of memory ability in ecstasy users: a web-based study". J. Psychopharmacol. (Oxford). 17 (4): 389–96. doi:10.1177/0269881103174016. PMID 14870950.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Halpern, J. H., Sherwood, A. R., Hudson, J. I., Gruber, S., Kozin, D., Pope Jr, H. G. (2011). "Residual neurocognitive features of long-term ecstasy users with minimal exposure to other drugs". Addiction. 106 (4): 777–786. doi:10.1111/j.1360-0443.2010.03252.x. PMC 3053129. PMID 21205042.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jones AL, Simpson KJ (1999). "Review article: mechanisms and management of hepatotoxicity in ecstasy (MDMA) and amphetamine intoxications" (PDF). Aliment. Pharmacol. Ther. 13 (2): 129–33. doi:10.1046/j.1365-2036.1999.00454.x. PMID 10102941.
- ^ Milosevic A, Agrawal N, Redfearn P, Mair L (1999). "The occurrence of toothwear in users of Ecstasy (3,4-methylenedioxymethamphetamine)" (PDF). Community Dent Oral Epidemiol. 27 (4): 283–7. doi:10.1111/j.1600-0528.1998.tb02022.x. PMID 10403088.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Creighton FJ, Black DL, Hyde CE (1991). "'Ecstasy' psychosis and flashbacks" (PDF). Br J Psychiatry. 159 (5): 713–5. doi:10.1192/bjp.159.5.713. PMID 1684523.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nimmo SM, Kennedy BW, Tullett WM, Blyth AS, Dougall JR (1993). "Drug-induced hyperthermia". Anaesthesia. 48 (10): 892–5. doi:10.1111/j.1365-2044.1993.tb07423.x. PMID 7902026.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Malberg JE, Seiden LS (1998). "Small changes in ambient temperature cause large changes in 3,4-methylenedioxymethamphetamine (MDMA)-induced serotonin neurotoxicity and core body temperature in the rat". J. Neurosci. 18 (13): 5086–94. PMID 9634574.
- ^ Wolff K, Tsapakis EM, Winstock AR; et al. (2006). "Vasopressin and oxytocin secretion in response to the consumption of ecstasy in a clubbing population". J. Psychopharmacol. (Oxford). 20 (3): 400–10. doi:10.1177/0269881106061514. PMID 16574714.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Fischer C, Hatzidimitriou G, Wlos J, Katz J, Ricaurte G (1995). "Reorganization of ascending 5-HT axon projections in animals previously exposed to the recreational drug (+/-)3,4-methylenedioxymethamphetamine (MDMA, "ecstasy")". J. Neurosci. 15 (8): 5476–85. PMID 7643196.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Scheffel U, Szabo Z, Mathews WB; et al. (1998). "In vivo detection of short- and long-term MDMA neurotoxicity—a positron emission tomography study in the living baboon brain". Synapse. 29 (2): 183–92. doi:10.1002/(SICI)1098-2396(199806)29:2<183::AID-SYN9>3.0.CO;2-3. PMID 9593108.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ a b Reneman L, Lavalaye J, Schmand B; et al. (2001). "Cortical serotonin transporter density and verbal memory in individuals who stopped using 3,4-methylenedioxymethamphetamine (MDMA or "ecstasy"): preliminary findings". Arch. Gen. Psychiatry. 58 (10): 901–6. doi:10.1001/archpsyc.58.10.901. PMID 11576026.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Ecstasy and Neurotoxicity at Dancesafe.org
- ^ Does MDMA Cause Brain Damage?, Matthew Baggott, and John Mendelson
- ^ Research on Ecstasy Is Clouded by Errors, Donald G. McNeil Jr., New York Times (2 December 2003).
- ^ Depression at DanceSafe.org
- ^ Wareing, M. and Fisk, J.E. and Murphy, P.N. (2000). "Working memory deficits in current and previous users of MDMA ('ecstasy')" (PDF). Br J Psychol. 91 (Pt 2): 181–8. doi:10.1348/000712600161772. PMID 10832513.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Study claims recreational ecstasy use and depression unrelated, Wikinews, (26 April 2006).
- ^ Guillot C, Greenway D (2006). "Recreational ecstasy use and depression" (PDF). J. Psychopharmacol. (Oxford). 20 (3): 411–6. doi:10.1177/0269881106063265. PMID 16574715.
- ^ Ecstasy Study Botched, Retracted, Kristen Philipkoski, Wired.com, 09.05.03
- ^ McCann UD, Ricaurte GA (2001). "Caveat emptor: editors beware" (PDF). Neuropsychopharmacology. 24 (3): 333–6. doi:10.1016/S0893-133X(00)00171-8. PMID 11256359.
- ^ Green AR, Mechan AO, Elliott JM, O'Shea E, Colado MI (2003). "The pharmacology and clinical pharmacology of 3,4-methylenedioxymethamphetamine (MDMA, "ecstasy")". Pharmacol. Rev. 55 (3): 463–508. doi:10.1124/pr.55.3.3. PMID 12869661.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zakzanis KK, Campbell Z, Jovanovski D (2007). "The neuropsychology of ecstasy (MDMA) use: a quantitative review". Hum Psychopharmacol. 22 (7): 427–35. doi:10.1002/hup.873. PMID 17896346.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gijsman HJ, Verkes RJ, van Gerven JM, Cohen AF (1999). "MDMA study" (PDF). Neuropsychopharmacology. 21 (4): 597. doi:10.1016/S0893-133X(99)00021-4. PMID 10481843.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kish, SJ (2002). "How strong is the evidence that brain serotonin neurons are damaged in human users of ecstasy?". Pharmacol. Biochem. Behav. 71 (4): 845–55. doi:10.1016/S0091-3057(01)00708-0. PMID 11888575.
- ^ Kish SJ (2003). "What is the evidence that Ecstasy (MDMA) can cause Parkinson's disease?" (PDF). Mov. Disord. 18 (11): 1219–23. doi:10.1002/mds.10643. PMID 14639660.
- ^ Aghajanian & Liebermann (2001) 'Caveat Emptor: Reseearchers Beware' Neuropsychopharmacology 24,3:335–6
- ^ McCann, Una D.; Ricaurte, George A. (1991). "Major metabolites of(±)3,4-methylenedioxyamphetamine (MDA) do not mediate its toxic effects on brain serotonin neurons". Brain Research. 545 (1–2): 279–282. doi:10.1016/0006-8993(91)91297-E. PMID 1860050.
- ^ Miller, RT; Lau, SS; Monks, TJ (1997). "2,5-Bis-(glutathion-S-yl)-alpha-methyldopamine, a putative metabolite of (+/-)-3,4-methylenedioxyamphetamine, decreases brain serotonin concentrations". Eur J Pharmacol. 323 (2–3): 173–80. doi:10.1016/S0014-2999(97)00044-7. PMID 9128836.
- ^ Conway, EL; Louis, WJ; Jarrot, B. (1978). "Acute and chronic administration of alpha-methyldopa: regional levels of endogenous and alpha-methylated catecholamines in rat brain". Eur J Pharmacol. 52 (3–4): 271–80. doi:10.1016/0014-2999(78)90279-0. PMID 729639.
- ^ Test Result Statistics: Summary Data. EcstasyData.org. Retrieved on 29 August 2012.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 14616331, please use {{cite journal}} with
|pmid=14616331instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18393753, please use {{cite journal}} with
|pmid=18393753instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6103055, please use {{cite journal}} with
|pmid=6103055instead. - ^ Scientists want new drug rankings, BBC News (23 March 2007).
- ^ a b Nutt DJ (2009). "Equasy-- an overlooked addiction with implications for the current debate on drug harms". J Psychopharmacol. 23 (1): 3–5. doi:10.1177/0269881108099672. PMID 19158127.
- ^ Horizon (2008) Britain's most dangerous drugs. Tuesday 5 February 2008, 9pm, BBC Two.
- ^ Forsyth, A (1 November 2001). "Distorted? a quantitative exploration of drug fatality reports in the popular press". International Journal of Drug Policy. 12 (5–6): 435–453. doi:10.1016/S0955-3959(01)00092-5.
- ^ Ecstasy 'not worse than riding', BBC News, 7 February 2009
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17620161, please use {{cite journal}} with
|pmid=17620161instead. - ^ Vuori E, Henry JA, Ojanperä I; et al. (2003). "Death following ingestion of MDMA (ecstasy) and moclobemide". Addiction. 98 (3): 365–8. doi:10.1046/j.1360-0443.2003.00292.x. PMID 12603236.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ The Prozac Misunderstanding, at TheDEA.org
- ^ Lynn T. Singer; Derek G. Moore; Sarah Fulton; Julia Goodwin; John J.D. Turner; Meeyoung O. Min; Andrew C. Parrott (May 2012). "Neurobehavioral Outcomes of Infants Exposed to MDMA (Ecstasy) and Other Recreational Drugs During Pregnancy". Neurotoxicology and Teratology.
- ^ a b "Ecstasy in Pregnancy Is Bad for Baby, Study Finds author1=Stephanie Pappas". 8 March 2012.
{{cite web}}: Missing pipe in:|title=(help) - ^ Milhazes N, Martins P, Uriarte E; et al. (2007). "Electrochemical and spectroscopic characterisation of amphetamine-like drugs: application to the screening of 3,4-methylenedioxymethamphetamine (MDMA) and its synthetic precursors". Anal. Chim. Acta. 596 (2): 231–41. doi:10.1016/j.aca.2007.06.027. PMID 17631101.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Milhazes N, Cunha-Oliveira T, Martins P; et al. (2006). "Synthesis and cytotoxic profile of 3,4-methylenedioxymethamphetamine ("ecstasy") and its metabolites on undifferentiated PC12 cells: A putative structure-toxicity relationship". Chem. Res. Toxicol. 19 (10): 1294–304. doi:10.1021/tx060123i. PMID 17040098.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Reductive aminations of carbonyl compounds with borohydride and borane reducing agents. Baxter, Ellen W.; Reitz, Allen B. Organic Reactions (Hoboken, New Jersey, United States) (2002), 59.
- ^ Gimeno P, Besacier F, Bottex M, Dujourdy L, Chaudron-Thozet H (2005). "A study of impurities in intermediates and 3,4-methylenedioxymethamphetamine (MDMA) samples produced via reductive amination routes". Forensic Sci. Int. 155 (2–3): 141–57. doi:10.1016/j.forsciint.2004.11.013. PMID 16226151.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nov 2005 DEA Microgram newsletter, p. 166. Usdoj.gov (11 November 2005). Retrieved on 12 August 2013.
- ^ a b Fitzgerald JL, Reid JJ (1990). "Effects of methylenedioxymethamphetamine on the release of monoamines from rat brain slices". European Journal of Pharmacology. 191 (2): 217–20. doi:10.1016/0014-2999(90)94150-V. PMID 1982265.
- ^ Bogen IL, Haug KH, Myhre O, Fonnum F (2003). "Short- and long-term effects of MDMA ("ecstasy") on synaptosomal and vesicular uptake of neurotransmitters in vitro and ex vivo". Neurochemistry International. 43 (4–5): 393–400. doi:10.1016/S0197-0186(03)00027-5. PMID 12742084.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fleckenstein AE, Volz TJ, Riddle EL, Gibb JW, Hanson GR (2007). "New insights into the mechanism of action of amphetamines". Annual Review of Pharmacology and Toxicology. 47: 681–98. doi:10.1146/annurev.pharmtox.47.120505.105140. PMID 17209801.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11723224, please use {{cite journal}} with
|pmid=11723224instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19364908, please use {{cite journal}} with
|pmid=19364908instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11459929, please use {{cite journal}} with
|pmid=11459929instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18310473, please use {{cite journal}} with
|pmid=18310473instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17234900, please use {{cite journal}} with
|pmid=17234900instead. - ^ Battaglia G, Brooks BP, Kulsakdinun C, De Souza EB (1988). "Pharmacologic profile of MDMA (3,4-methylenedioxymethamphetamine) at various brain recognition sites". European Journal of Pharmacology. 149 (1–2): 159–63. doi:10.1016/0014-2999(88)90056-8. PMID 2899513.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lyon RA, Glennon RA, Titeler M (1986). "3,4-Methylenedioxymethamphetamine (MDMA): stereoselective interactions at brain 5-HT1 and 5-HT2 receptors". Psychopharmacology. 88 (4): 525–6. doi:10.1007/BF00178519. PMID 2871581.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nash JF, Roth BL, Brodkin JD, Nichols DE, Gudelsky GA (1994). "Effect of the R(-) and S(+) isomers of MDA and MDMA on phosphatidyl inositol turnover in cultured cells expressing 5-HT2A or 5-HT2C receptors". Neuroscience Letters. 177 (1–2): 111–5. doi:10.1016/0304-3940(94)90057-4. PMID 7824160.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Setola V, Hufeisen SJ, Grande-Allen KJ; et al. (2003). "3,4-methylenedioxymethamphetamine (MDMA, "Ecstasy") induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro". Molecular Pharmacology. 63 (6): 1223–9. doi:10.1124/mol.63.6.1223. PMID 12761331.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Ecstasy Really Does Unleash the Love Hormone". New Scientist. 4 April 2007.
- ^ Theodoridou A, Rowe AC, Penton-Voak IS, Rogers PJ (2009). "Oxytocin and social perception: oxytocin increases perceived facial trustworthiness and attractiveness". Horm Behav. 56 (1): 128–32. doi:10.1016/j.yhbeh.2009.03.019. PMID 19344725.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dumont GJ, Sweep FC, van der Steen R, Hermsen R, Donders AR, Touw DJ, van Gerven JM, Buitelaar JK, Verkes RJ. (2009). "Increased oxytocin concentrations and prosocial feelings in humans after ecstasy (3,4-methylenedioxymethamphetamine) administration" (PDF). Soc Neurosci. 4 (4): 359–366. doi:10.1080/17470910802649470. PMID 19562632.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Johansen, PO.; Krebs, TS. (2009). "How could MDMA (ecstasy) help anxiety disorders? A neurobiological rationale" (PDF). Journal of Psychopharmachology. 23 (4): 389–91. doi:10.1177/0269881109102787. PMID 19273493.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b R. De La Torre, M. Farré, J. Ortuño, M. Mas, R. Brenneisen, P. N. Roset, ; et al. (February 2000). "Non-linear pharmacokinetics of MDMA ('ecstasy') in humans". Annals of the New York Academy of Sciences. 49 (2): 104–109. doi:10.1046/j.1365-2125.2000.00121.x.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ R. DE LA TORRE, M. FARRÉ, P. N. ROSET, C. HERNÁNDEZ LÓPEZ, M. MAS, J. ORTUÑO; et al. (September 2000). "Pharmacology of MDMA in humans". Annals of the New York Academy of Sciences. 914 (1): 225–237. doi:10.1111/j.1749-6632.2000.tb05199.x.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Verebey K, Alrazi J, Jaffe JH (1988). "The complications of 'ecstasy' (MDMA)". JAMA. 259 (11): 1649–1650. doi:10.1001/jama.259.11.1649. PMID 2893845.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ eMedicine – Toxicity, MDMA: Article by David Yew. Emedicine.com. Retrieved on 11 June 2011.
- ^ de la Torre R, Farré M, Roset PN; et al. (2004). "Human pharmacology of MDMA: pharmacokinetics, metabolism, and disposition" (PDF). Ther Drug Monit. 26 (2): 137–44. doi:10.1097/00007691-200404000-00009. PMID 15228154.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Shima N, Kamata H, Katagi M, Tsuchihashi H, Sakuma T, Nemoto N (2007). "Direct Determination of Glucuronide and Sulfate of 4-Hydroxy-3-methoxymethamphetamine, the Main Metabolite of MDMA, in Human Urine". J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 857 (1): 123–129. doi:10.1016/j.jchromb.2007.07.003. PMID 17643356.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Michael H. Baumann and Richard B. Rothman (6 November 2009). "NEURAL AND CARDIAC TOXICITIES ASSOCIATED WITH 3,4-METHYLENEDIOXYMETHAMPHETAMINE (MDMA)". International Review of Neurobiology. International Review of Neurobiology. 88 (1): 257–296. doi:10.1016/S0074-7742(09)88010-0. ISBN 9780123745040. PMC 3153986. PMID 19897081.
- ^ J. K. Fallon, A. T. Kicman, J. A. Henry, P. J. Milligan, D. A. Cowan, A. J. Hutt (1 July 1999). "Stereospecific Analysis and Enantiomeric Disposition of 3,4-Methylenedioxymethamphetamine (Ecstasy) in Humans". Clinical Chemistry. 45 (7): 1058–1069. PMID 10388483.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Melanie Mueller, Frank T. Peters, Hans H. Maurer, Una D. McCann and George A. Ricaurte (October 2008). "Nonlinear Pharmacokinetics of (±)3,4-Methylenedioxymethamphetamine (MDMA, "Ecstasy") and Its Major Metabolites in Squirrel Monkeys at Plasma Concentrations of MDMA That Develop After Typical Psychoactive Doses". JPET. 327 (1): 38–44. doi:10.1124/jpet.108.141366.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kolbrich EA, Goodwin RS, Gorelick DA, Hayes RJ, Stein EA, Huestis MA. Plasma pharmacokinetics of 3,4-methylenedioxymethamphetamine after controlled oral administration to young adults. Ther. Drug Monit. 30: 320–332, 2008.
- ^ Barnes, AJ; De Martinis, BS; Gorelick, DA; Goodwin, RS; Kolbrich, EA; Huestis, MA (2009). "Disposition of MDMA and metabolites in human sweat following controlled MDMA administration" (PDF). Clinical chemistry. 55 (3): 454–62. doi:10.1373/clinchem.2008.117093. PMC 2669283. PMID 19168553.
- ^ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 9th edition, Biomedical Publications, Seal Beach, California, 2011, pp. 1078–1080.
- ^ a b Bernschneider-Reif S, Oxler F, Freudenmann RW (2006). "The origin of MDMA ('Ecstasy') – separating the facts from the myth". Pharmazie. 61 (11): 966–972. PMID 17152992.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Firma E. Merck in Darmstadt (16 May 1914). "German Patent 274350: Verfahren zur Darstellung von Alkyloxyaryl-, Dialkyloxyaryl- und Alkylendioxyarylaminopropanen bzw. deren am Stickstoff monoalkylierten Derivaten". Kaiserliches Patentamt. Retrieved 12 April 2009.
- ^ Firma E. Merck in Darmstadt (15 October 1914). "German Patent 279194: Verfahren zur Darstellung von Hydrastinin Derivaten". Kaiserliches Patentamt.
- ^ Lowlinson JH, Ruiz P, Millman RB, Langrod JG. Substance Abuse: A Comprehensive Textbook. Williams & Wilkins. 1997. pp. 269–275.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Hardman HF, Haavik CO, Seevers MH (1973). "Relationship of the Structure of Mescaline and Seven Analogs to Toxicity and Behavior in Five Species of Laboratory Animals". Toxicology Applied Pharmacology. 25 (2): 299–309. doi:10.1016/S0041-008X(73)80016-X. PMID 4197635.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The first confirmed sample was seized and identified by Chicago Police in 1970, seeSreenivasan VR (1972). "Problems in Identification of Methylenedioxy and Methoxy Amphetamines". Journal of Criminal Law, Criminology & Police Science. 63 (2). The Journal of Criminal Law, Criminology, and Police Science, Vol. 63, No. 2: 304–312. doi:10.2307/1142315. JSTOR 1142315.
- ^ a b Ann Shulgin; Alexander Shulgin (1991). PiHKAL: A Chemical Love Story. Part I. Chapter 12. Transform Press. ISBN 0-9630096-0-5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Shulgin AT; Nichols DE (1978). "Characterization of Three New Psychotomimetics". In Willette, Robert E.; Stillman, Richard Joseph (ed.). The Psychopharmacology of Hallucinogens. New York: Pergamon Press. pp. 74–83. ISBN 0-08-021938-1.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Bennett, Drake (30 January 2005). "Dr. Ecstasy". New York Times Magazine.
- ^ Myron J. Stolaroff (2005). The Secret Chief Revealed. MAPS. pp. 16–18. ISBN 0-9660019-6-6.
- ^ Doblin, Rick. "A Clinical Plan for MDMA (Ecstasy) in the Treatment of Post-Traumatic Stress Disorder (PTSD): Partnering with the FDA". Multidisciplinary Association for Psychedelic Studies. Retrieved 9 December 2013.
- ^ McKinley, Jr., James C. (12 September 2013). "Overdoses of 'Molly' Led to Electric Zoo Deaths". The New York Times. Retrieved 9 December 2013.
- ^ ''The Austin Chronicle'' – "Countdown to Ecstasy." by Marc Savlov. Weeklywire.com. Retrieved on 11 June 2011.
- ^ Idol, Billy. Billy Idol. Track 9, "It's So Cruel"
- ^ "Pharmaceutical Company Unravels Drug's Chequered Past". 2005.
- ^ Erowid MDMA Vault: Info No. 3 on Scheduling. Erowid.org. Retrieved on 11 June 2011.
- ^ a b ''Primetime'' with Peter Jennings. Video.google.com. Retrieved on 11 June 2011.
- ^ Bibliography of Psychedelic Research Studies. collected by the Multidisciplinary Association for Psychedelic Studies
- ^ "Mephedrone (4-Methylmethcathinone) appearing in "Ecstasy" in the Netherlands". 19 September 2010. Retrieved 31 December 2012.
- ^ "Why ecstasy is 'vanishing' from UK nightclubs". BBC News. 19 January 2010. Retrieved 14 February 2010.
- ^ Misuse of Drugs Act 1971. Statutelaw.gov.uk (5 January 1998). Retrieved on 11 June 2011.
- ^ a b A review of MDMA ('ecstasy'), its harms and classification under the Misuse of Drugs Act 1971, Advisory Council on the Misuse of Drugs (ACMD), 11 February 2009
- ^ Drugs and the law: Report of the inquiry into the Misuse of Drugs Act 1971 London: Police Foundation, 2000, Runciman Report
- ^ "The Government's Drugs Policy: Is it working?" House of Commons, Home Affairs Committee, May 2002
- ^ [Fifth Report], UK House of Commons, Science and Technology Committee, (July 2006) Drug classification: Making a hash of it?
- ^ Kmietowicz Z (2009). "UK government rejects advice from drugs adviser to downgrade ecstasy". BMJ. 338: b592. doi:10.1136/bmj.b592. PMID 19218326.
- ^ Campbell A (Home Office minister). Letter to professor David Nutt (chair of the ACMD). (2009) [dead link]
- ^ Blakemore C (2009). "Classification of cannabis and ecstasy in the UK". BMJ. 338 (1): b731. doi:10.1136/bmj.b731. PMID 19233870.
- ^ Editorial: Drugs drive politicians out of their minds New Scientist (11 February 2009).
- ^ MAPS. "Documents from the DEA Scheduling Hearing of MDMA,".
- ^ MDMA (Ecstasy) Law & Policy Center for Cognitive Liberty & Ethics
- ^ Grinspoon v. Drug Enforcement Administration, 828 F.2d 881 (1st Cir. 1987)
- ^ Schedules of Controlled Substances; Deletion of 3,4-Methylenedioxymethamphetamine (MDMA) From Schedule I of the Controlled Substances Act, 53 Fed. Reg. 2,225 (DEA 1988).
- ^ Schedules of Controlled Substances; Scheduling of 3,4-Methylenedioxymethamphetamine (MDMA) Into Schedule I of the Controlled Substances Act; Remand, 53 Fed. Reg. 5,156 (DEA 22 February 1988).
- ^ Court Rejects Harsh Federal Drug Sentencing Guideline as Scientifically Unjustified | American Civil Liberties Union. Aclu.org (15 July 2011). Retrieved on 29 August 2012.
- ^ Rapport Drugs in Lijsten | Rapport. Rijksoverheid.nl (27 June 2011). Retrieved on 29 August 2012.
- ^ Committee: the current system of the Opium Act does not have to be changed | Press release. Government.nl (24 June 2011). Retrieved on 29 August 2012.
- ^ "Schedule I". Controlled Drugs and Substances Act. Isomer Design. Retrieved 9 December 2013.
- ^ "Definitions and interpretations". Controlled Drugs and Substances Act. Isomer Design. Retrieved 9 December 2013.
- ^ "Backgrounder: The Safe Streets and Communities Act Four Components Coming Into Force". Canadian Department of Justice. Retrieved 9 December 2013.
- ^ a b c 22nd report of the Expert Committee on Drug Dependence World Health Organization, 1985. (PDF) . Retrieved on 29 August 2012.
- ^ E for Ecstasy by Nicholas Saunders, Appendix 1: Reference Section. Ecstasy.org. Retrieved on 11 June 2011.
- ^ European Monitoring Centre for Drugs and Drug Addiction (2008). Annual report: the state of the drugs problem in Europe (PDF). Luxembourg: Office for Official Publications of the European Communities. p. 49. ISBN 978-92-9168-324-6.
- ^ United Nations Office on Drugs and Crime (2008). World drug report (PDF). United Nations Publications. p. 271. ISBN 978-92-1-148229-4.
- ^ Camargo, Jorge (30 November 2012). "Monitoring of illicit pill distribution networks using an image collection exploration framework". Forensic Science International. 223 (1): 298–305. doi:10.1016/j.forsciint.2012.10.004. Retrieved 9 December 2013.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Drugtext – 10 years of ecstasy and other party drug use in Australia: What have we done and what is there left to do?. Drugtext.org. Retrieved on 11 June 2011.
Further reading
- Julie Holland – "Ecstasy: The Complete Guide: A Comprehensive Look at the Risks and Benefits of MDMA" Park Street Press (2001).
- Jerome Beck, Marsha Rosenbaum – "Pursuit of Ecstasy: The MDMA Experience" SUNY Press (1994).
- Leslie Iversen – "Speed, Ecstasy, Ritalin: The Science of Amphetamines" Oxford University Press (2008).
- David Pearce – "Utopian Pharmacology: Mental Health in the Third Millenium: MDMA and Beyond" (2008).
- Earth Erowid – "Do Antioxidants Protect Against MDMA Hangover, Tolerance, and Neurotoxicity?" Erowid Extracts (2001).
- Marsha Rosenbaum, Rick Doblin – "Why MDMA Should Not Have Been Made Illegal" SAGE Publications (1991).
- Nature News – "Ecstasy Could Augment the Benefits of Psychotherapy" (2008).
- Nature News – "Party drug could ease trauma long term" (2010).
- Reuters Health – "Ecstasy May Help PTSD Victims Get Better" (2009).
- The Economist – "Agony and Ecstasy: Ecstasy May Be Good For Those Who Can’t Get Over Something Truly Horrible" (2008).
- New Scientist – "Ecstasy's Long-Term Effects Revealed" (2009).
- Matt Palmquist Miller-McCune – "The Ecstasy and the Agony" (August 2009).
- ACMD – "MDMA (Ecstasy): A Review of its Harms and Classification Under the Misuse of Drugs Act 1971" UK Home Office (2009).
- NIDA InfoFacts – "MDMA (Ecstasy)" (September 2013).
External links
- Alexander Shulgin & Ann Shulgin – PiHKAL: "No. 109 MDMA: MDM; ADAM; Ecstasy; 3,4-Methylenedioxy-N-methylamphetamine" (1991).
- ABC News – "Primetime Special: Peter Jennings – Ecstasy Rising" (2004).
- The Vaults of Erowid: "MDMA ("Ecstasy")".
- Erowid Experience Vaults: "MDMA ("Ecstasy", "E", "X") Reports".
- DanceSafe: ": What is Ecstasy?".
- MAPS: "R&D Medicines > MDMA".
- National Institute on Drug Abuse: "MDMA Facts for Teens".
- National Institute on Drug Abuse: "MDMA Facts and Statistics".
- EcstasyData.org: Providing Access to Lab Testing Results for Street Ecstasy Tablets.
- PillReports.com: Ecstasy Test Results Database by Enlighten.
- Fifteen Minutes: E is for Ecstasy
- Jessica Winter, "Can a Single Pill Change Your Life?" O Magazine, 15 February 2011


