Ebola: Difference between revisions
Prokaryotes (talk | contribs) m →ZMapp antibody treatment: of the |
Crazycasta (talk | contribs) →Behavioral changes: were->where (spelling fix) |
||
| Line 95: | Line 95: | ||
[[File:Biosafety level 4 hazmat suit.jpg|thumb|A researcher working with the Ebola virus while wearing a [[positive pressure personnel suit|BSL-4 positive pressure suit]] to avoid infection]] |
[[File:Biosafety level 4 hazmat suit.jpg|thumb|A researcher working with the Ebola virus while wearing a [[positive pressure personnel suit|BSL-4 positive pressure suit]] to avoid infection]] |
||
===Behavioral changes=== |
===Behavioral changes=== |
||
Ebola viruses are [[Contagious disease|contagious]], with prevention predominantly involving behavior changes, proper full body [[personal protective equipment]], and [[disinfection]]. Techniques to avoid infection involve not contacting infected blood or secretions, including from those who are dead.<ref name=CDC2014P/> This involves suspecting and diagnosing the disease early and using [[standard precautions]] for all patients in the healthcare setting.<ref name=CDC1998>{{Cite book|last=Centers for Disease Control and Prevention and World Health Organization | title = Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting | url = http://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf | format = PDF | accessdate = 2013-02-08 | year = 1998 | publisher = Centers for Disease Control and Prevention | location = Atlanta, Georgia, US }}</ref> Recommended measures when caring for those who are infected include: wearing protective clothing including: masks, gloves, gowns and goggles, equipment sterilization and isolating them.<ref name=CDC2014P/> [[Hand washing]] is important but can be difficult in areas |
Ebola viruses are [[Contagious disease|contagious]], with prevention predominantly involving behavior changes, proper full body [[personal protective equipment]], and [[disinfection]]. Techniques to avoid infection involve not contacting infected blood or secretions, including from those who are dead.<ref name=CDC2014P/> This involves suspecting and diagnosing the disease early and using [[standard precautions]] for all patients in the healthcare setting.<ref name=CDC1998>{{Cite book|last=Centers for Disease Control and Prevention and World Health Organization | title = Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting | url = http://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf | format = PDF | accessdate = 2013-02-08 | year = 1998 | publisher = Centers for Disease Control and Prevention | location = Atlanta, Georgia, US }}</ref> Recommended measures when caring for those who are infected include: wearing protective clothing including: masks, gloves, gowns and goggles, equipment sterilization and isolating them.<ref name=CDC2014P/> [[Hand washing]] is important but can be difficult in areas where there is not even enough water for drinking.<ref name=Gath2014/> |
||
Due to lack of proper equipment and hygienic practices, large-scale epidemics have occured mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Traditional [[burial]] rituals, especially those requiring [[embalming]] of bodies, should be discouraged or modified.<ref name=CDC1998/> Airline crews who fly to areas of these areas of the world are taught to identify Ebola and are to isolate anyone who has symptoms.<ref>[http://www.webmd.com/a-to-z-guides/ebola-fever-virus-infection Ebola Virus: Symptoms, Treatment, and Prevention<!-- Bot generated title -->]</ref> |
Due to lack of proper equipment and hygienic practices, large-scale epidemics have occured mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Traditional [[burial]] rituals, especially those requiring [[embalming]] of bodies, should be discouraged or modified.<ref name=CDC1998/> Airline crews who fly to areas of these areas of the world are taught to identify Ebola and are to isolate anyone who has symptoms.<ref>[http://www.webmd.com/a-to-z-guides/ebola-fever-virus-infection Ebola Virus: Symptoms, Treatment, and Prevention<!-- Bot generated title -->]</ref> |
||
Revision as of 00:39, 5 August 2014
| Ebola | |
|---|---|
| Specialty | Infectious diseases |
Ebola virus disease (EVD) or Ebola hemorrhagic fever (EHF) is the human disease caused by the Ebola virus. Symptoms typically start two days to three weeks after infection with the EVD virus: fever, sore throat, myalgia (muscle pains), and headaches. Typically, nausea, vomiting, and diarrhea occur, followed by decreased functioning of the liver and kidneys. At that point in the course of the Ebola virus disease, some infected people begin to suffer bleeding.[1]
Infection with the Ebola virus can occur upon contact with either the blood or the bodily fluids of an infected animal: (monkey, fruit bat, pig) or human being.[1] The Ebola virus disease is not naturally transmitted through the air; the EV is not inhaled.[2] Fruit bats are believed to carry and spread the EVD virus without being infected or affected. The human diagnosis of EVD infection is by the exclusion and elimination of other diseases with similar symptoms, such as malaria, cholera, and other viral hemorrhagic fevers. Blood samples are tested for viral antibodies, viral RNA, and the EVD virus, itself, to confirm the EVD-infection diagnosis.[1] Once human infection occurs, the disease can spread among people; and a male survivor of EVD might transmit the Ebola virus disease via his semen, for approximately two months after recovery.
Prevention of the EVD includes decreasing the spread of the disease from infected monkeys and pigs to humans. This can be done by checking for and detecting EVD infection in such livestock, then killing the infected animals, and properly destroying the bodies. Properly cooking meat and wearing protective clothing when handling meat are helpful measures, as are wearing protective clothing and washing hands when around a patient with EVD. Samples of bodily fluids and tissues from EVD patients are handled with special caution.[1]
There is no specific treatment for the disease; efforts to help persons who are infected include giving either oral rehydration therapy (slightly sweet and salty water to drink) or intravenous fluids.[1] The disease has high mortality rate: often killing between 50% and 90% of those infected with the virus.[1][3] EVD was first identified in Sudan and the Democratic Republic of the Congo. The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] Between 1976, when it was first identified, through 2013, fewer than 1,000 people per year have been infected.[1][4] The largest outbreak to date is the ongoing 2014 West Africa Ebola outbreak, which is affecting Guinea, Sierra Leone, and Liberia.[5] As of July 2014 more than 1320 cases have been identified.[5] Efforts are ongoing to develop a vaccine; however, none yet exists.[1]
Signs and symptoms

Signs and symptoms of Ebola usually begin suddenly with an flu-like stage characterized by fatigue, fever, headaches, and joint, muscle, and abdominal pain.[7][8] Vomiting, diarrhea and loss of appetite are also common.[8] Less common symptoms include the following: sore throat, chest pain, hiccups, shortness of breath and trouble swallowing.[8] The average time between contracting the infection and the start of symptoms is 8 to 10 days, but can occur between 2 and 21 days.[8] Skin manifestations may include a maculopapular rash (in about 50% of cases).[9] Early symptoms of EVD may be similar to those of malaria, dengue fever, or other tropical fevers, before the disease progresses to the bleeding phase.[7]
Bleeding
In the bleeding phase internal and subcutaneous bleeding may present itself through reddening of the eyes and bloody vomit.[7] Bleeding into the skin may create petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites).
All people infected show some symptoms of circulatory system involvement, including impaired blood clotting.[9] Bleeding from puncture sites and mucous membranes (e.g. gastrointestinal tract, nose, vagina and gums) is reported in 40–50% of cases.[10] Types of bleeding known to occur with Ebola virus disease include vomiting blood, coughing it up or blood in the stool. Heavy bleeding is rare and is usually confined to the gastrointestinal tract.[9][11] In general, the development of bleeding symptoms often indicates a worse prognosis and this blood loss can result in death.[12]
Causes

EVD is caused by four of five viruses classified in the genus Ebolavirus, family Filoviridae, order Mononegavirales. These four viruses are Bundibugyo virus (BDBV), Ebola virus (EBOV), Sudan virus (SUDV), Taï Forest virus (TAFV). The fifth virus, Reston virus (RESTV), is not thought to be disease-causing in humans. During an outbreak those at highest risk are health care workers and close contacts of those with the infection.[13]
Transmission
It is not entirely clear how Ebola is spread.[14] EVD is believed to occur after an ebola virus is transmitted to an initial human by contact with an infected animal's bodily fluids. Human-to-human transmission can occur via direct contact with blood or bodily fluids from an infected person (including embalming of an infected dead person) or by contact with contaminated medical equipment, particularly needles and syringes.[15] Semen is infectious in survivors for up to 50 days. Transmission through oral exposure and through conjunctiva exposure is likely[16] and has been confirmed in non-human primates.[17] The potential for widespread EVD infections is considered low as the disease is only spread by direct contact with the secretions from someone who is showing signs of infection.[15] The quick onset of symptoms makes it easier to identify sick individuals and limits a person's ability to spread the disease by traveling. Because dead bodies are still infectious, some doctors disposed of them in a safe manner, despite local traditional burial rituals.[18]
Medical workers who do not wear appropriate protective clothing may also contract the disease.[19] In the past, hospital-acquired transmission has occurred in African hospitals due to the reuse of needles and lack of universal precautions.[20]
EVD is not naturally transmitted through the air.[2] They are, however, infectious as breathable 0.8–1.2 micrometre laboratory generated droplets;[21] because of this potential route of infection, these viruses have been classified as Category A biological weapons.[22] Recently the virus has been shown to travel without contact from pigs to non-human primates.[23]
Bats drop partially eaten fruits and pulp, then land mammals such as gorillas and duikers feed on these fallen fruits. This chain of events forms a possible indirect means of transmission from the natural host to animal populations, which have led to research towards viral shedding in the saliva of bats. Fruit production, animal behavior, and other factors vary at different times and places that may trigger outbreaks among animal populations.[24]
Reservoir

Bats are considered the most likely natural reservoir of the Ebola virus (EBOV); plants, arthropods, and birds have also been considered.[26] Bats were known to reside in the cotton factory in which the first cases for the 1976 and 1979 outbreaks were employed, and they have also been implicated in Marburg virus infections in 1975 and 1980.[27] Of 24 plant species and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.[28] The absence of clinical signs in these bats is characteristic of a reservoir species. In a 2002–2003 survey of 1,030 animals including 679 bats from Gabon and the Republic of the Congo, 13 fruit bats were found to contain EBOV RNA fragments.[29] As of 2005, three types of fruit bats (Hypsignathus monstrosus, Epomops franqueti, and Myonycteris torquata) have been identified as being in contact with EBOV. They are now suspected to represent the EBOV reservoir hosts.[30][31] Antibodies against Ebola Zaire and Reston viruses have been found in fruit bats in Bangladesh, thus identifying potential virus hosts and signs of the filoviruses in Asia.[32]
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians, and arthropods sampled from outbreak regions, no ebolavirus was detected apart from some genetic traces found in six rodents (Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic.[27][33] Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high lethality from infection in these species makes them unlikely as a natural reservoir.[27]
Transmission between natural reservoir and humans is rare, and outbreaks are usually traceable to a single case where an individual has handled the carcass of gorilla, chimpanzee, or duiker.[34] Fruit bats are also eaten by people in parts of West Africa where they are smoked, grilled or made into a spicy soup.[31][35]
Virology
Genome

Like all mononegaviruses, ebolavirions contain linear nonsegmented, single-strand, non-infectious RNA genomes of negative polarity that possesses inverse-complementary 3' and 5' termini, do not possess a 5' cap, are not polyadenylated, and are not covalently linked to a protein.[36] Ebolavirus genomes are approximately 19 kilobase pairs long and contain seven genes in the order 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[37] The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV, and TAFV) differ in sequence and the number and location of gene overlaps.
Structure
Like all filoviruses, ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched.[37] In general, ebolavirions are 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974 to 1,086 nm (in contrast to marburgvirions, whose median particle length was measured at 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture.[38]
Replication
The ebolavirus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol. The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is, therefore, a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-strand antigenomes that are, in turn, transcribed into negative-strand virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.[39]
Pathophysiology
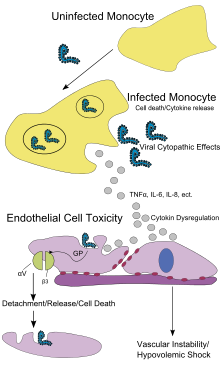
Endothelial cells, mononuclear phagocytes, and hepatocytes are the main targets of infection. After infection, a secreted glycoprotein (sGP) known as the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a trimeric complex, which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a dimeric protein that interferes with the signaling of neutrophils, a type of white blood cell, which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen.[40]
The presence of viral particles and cell damage resulting from budding causes the release of cytokines (to be specific, TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.[41]
Diagnosis
The medical history, especially travel and work history along with exposure to wildlife are important to suspect the diagnosis of EVD. The diagnosis is confirmed by isolating the virus, detecting its RNA or proteins, or detecting antibodies against the virus in a person's blood. Isolating the virus by cell culture, detecting the viral RNA by polymerase chain reaction (PCR) and detecting proteins by enzyme-linked immunosorbent assay (ELISA) is effective early and in those who have died from the disease. Detecting antibodies against the virus is effective late in the disease and in those who recover.[42]
During an outbreak, virus isolation is often not feasible. The most common diagnostic methods are therefore real time PCR and ELISA detection of proteins, which can be performed in field or mobile hospitals.[43] Filovirions can be seen and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot tell the difference between the various filoviruses despite there being some length differences.[38]
Classification

The genera Ebolavirus and Marburgvirus were originally classified as the species of the now-obsolete Filovirus genus. In March 1998, the Vertebrate Virus Subcommittee proposed in the International Committee on Taxonomy of Viruses (ICTV) to change the Filovirus genus to the Filoviridae family with two specific genera: Ebola-like viruses and Marburg-like viruses. This proposal was implemented in Washington, DC on April 2001 and in Paris on July 2002. In 2000, another proposal was made in Washington, D.C., to change the "-like viruses" to "-virus" resulting in today's Ebolavirus and Marburgvirus.[44]
Rates of genetic change are 100 times slower than influenza A in humans, but on the same magnitude as those of hepatitis B. Extrapolating backwards using these rates indicates that Ebolavirus and Marburgvirus diverged several thousand years ago.[45] However, paleoviruses (genomic fossils) of filoviruses (Filoviridae) found in mammals indicate that the family itself is at least tens of millions of years old.[46] Fossilized viruses that are closely related to ebolaviruses have been found in the genome of the Chinese hamster.[47]
Differential diagnosis
The symptoms of EVD are similar to those of Marburg virus disease.[48] It can also easily be confused with many other diseases common in Equatorial Africa such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis. Other infectious diseases that should be included in the differential diagnosis include the following: leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, hemorrhagic smallpox, measles, and fulminant viral hepatitis.[citation needed] Non-infectious diseases that can be confused with EVD are acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and even warfarin poisoning.[49][50][51][52]
Prevention

Behavioral changes
Ebola viruses are contagious, with prevention predominantly involving behavior changes, proper full body personal protective equipment, and disinfection. Techniques to avoid infection involve not contacting infected blood or secretions, including from those who are dead.[14] This involves suspecting and diagnosing the disease early and using standard precautions for all patients in the healthcare setting.[53] Recommended measures when caring for those who are infected include: wearing protective clothing including: masks, gloves, gowns and goggles, equipment sterilization and isolating them.[14] Hand washing is important but can be difficult in areas where there is not even enough water for drinking.[12]
Due to lack of proper equipment and hygienic practices, large-scale epidemics have occured mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Traditional burial rituals, especially those requiring embalming of bodies, should be discouraged or modified.[53] Airline crews who fly to areas of these areas of the world are taught to identify Ebola and are to isolate anyone who has symptoms.[54]
Quarantine
Quarantine, also known as enforced isolation, is usually effective in decreasing spread.[55][56] Governments often quarantine areas where the disease is occurring or those who may be infected.[57] In the United States the law allows quarantine of those infected with Ebola.[58] The lack of roads and transportation may help slow the disease in Africa. During the 2014 outbreak Liberia closed schools.[59]
Vaccine
No vaccine is currently available for humans.[1][60][61] The most promising candidates are DNA vaccines[62] or vaccines derived from adenoviruses,[63] vesicular stomatitis Indiana virus (VSIV)[64][65][66] or filovirus-like particles (VLPs)[67] because these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.[68][69][70][71]
Vaccines have protected nonhuman primates. Immunization takes six months, which impedes the counter-epidemic use of the vaccines. Searching for a quicker onset of effectiveness, in 2003 a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein was tested on crab-eating macaques. Twenty-eight days later they were challenged with the virus and remained resistant.[63] A vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or the Marburg glycoprotein in 2005 protected nonhuman primates,[72] opening clinical trials in humans.[68] The study by October completed the first human trial, over three months giving three vaccinations safely inducing an immune response. Individuals for a year were followed, and, in 2006, a study testing a faster-acting, single-shot vaccine began; this new study was completed in 2008.[69] Trying the vaccine on a strain of Ebola that more resembles the one that infects humans is the next step.[citation needed]
On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak.[73] An experimental vaccine made by researchers at Canada's national laboratory in Winnipeg was used in 2009 to pre-emptively treat a German scientist who might have been infected during a lab accident.[74] However, actual EBOV infection could never be demonstrated without a doubt.[75] Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis.[76][77][clarification needed]
Laboratory
Ebola viruses are World Health Organization Risk Group 4 pathogens, requiring biosafety level 4-equivalent containment. Laboratory researchers must be properly trained in BSL-4 practices and wear proper personal protective equipment.
Treatment

No ebolavirus-specific treatment exists.[61] Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control hemorrhaging, maintaining oxygen levels, pain management, and administration of antibiotics or antimycotics to treat secondary infections.[78][79][80] Early treatment may increase the chance of survival.[81]
However, during the 2014 West Africa Ebola outbreak, two American aid workers were given an experimental treatment, ZMapp, that had been used with good results in two sets of monkeys, via compassionate use protocols that significantly improved their critical condition.[82]
Prognosis
The disease has a high mortality rate: often between 50 percent and 90 percent.[1][3] If an infected person survives, recovery may be quick and complete. Prolonged cases are often complicated by the occurrence of long term problems, such as inflammation of the testicles, joint pains, muscle pains, skin peeling, or hair loss. Eye symptoms, such as light sensitivity, excess tearing, iritis, iridocyclitis, choroiditis and blindness have also been described. EBOV and SUDV may be able to persist in the semen of some survivors for up to seven weeks, which could give rise to infections and disease via sexual intercourse.[1]
Epidemiology

The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] Between 1976, when it was first identified, through 2013, fewer than 1,000 people per year have been infected.[1][4] The largest outbreak to date is the ongoing 2014 West Africa Ebola outbreak, which is affecting Guinea, Sierra Leone, and Liberia.[5] As of July 2014 more than 1320 cases have been identified.[5]
2007 to 2011
As of 30 August 2007, 103 people (100 adults and three children) were infected by a suspected hemorrhagic fever outbreak in the village of Kampungu, Democratic Republic of the Congo. The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The World Health Organization sent a team to take blood samples for analysis and confirmed that many of the cases were the result of Ebolavirus.[83][84] The Congo's last major Ebola epidemic killed 245 people in 1995 in Kikwit, about 200 miles (320 km) from the source of the August 2007 outbreak.[85]
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of Ebolavirus, which was tentatively named Bundibugyo.[86] The epidemic came to an official end on 20 February 2008. While it lasted, 149 cases of this new strain were reported, and 37 of those led to deaths.
An International Symposium to explore the environment and filovirus, cell system and filovirus interaction, and filovirus treatment and prevention was held at Centre Culturel Français, Libreville, Gabon, during March 2008.[87] The virus appeared in southern Kasai Occidental on 27 November 2008,[88] and blood and stool samples were sent to laboratories in Gabon and South Africa for identification.
On 25 December 2008, it was reported that the Ebola virus had killed 9 and infected 21 people in the Western Kasai province of the Democratic Republic of Congo.[89] On 29 December, Doctors Without Borders reported 11 deaths in the same area, stating that a further 24 cases were being treated. In January 2009, Angola closed down part of its border with the Democratic Republic of Congo to prevent the spread of the outbreak.[90]
On 12 March 2009, an unidentified 45-year-old scientist from Germany accidentally pricked her finger with a needle used to inject Ebola into lab mice. She was given an experimental vaccine never before used on humans. Since the peak period for an outbreak during the 21-day Ebola incubation period had passed as of 2 April 2009, she had been declared healthy and safe. It remains unclear whether or not she was ever actually infected with the virus.[91]
In May 2011, a 12-year-old girl in Uganda died from Ebola (Sudan subspecies). No further cases were recorded.[92]
2012 outbreaks
In July 2012, the Ugandan Health Ministry confirmed 13 deaths due to an outbreak of the Ebola-Sudan variant[93] in the Kibaale District.[94] On 28 July, it was reported that 14 out of 20 (70% mortality rate) had died in Kibaale.[95] On 30 July, Stephen Byaruhanga, a health official in Kibaale District, said the Ebola outbreak had spread from one remote village to several villages.[96]
The World Health Organization's (WHO) global and alert response network reported on August 3 that the suspected case count had risen to 53, including 16 deaths. Of these cases, five were confirmed by UVRI as Ebola cases. There were no confirmed cases outside of Kibaale District except for a patient who was medically evacuated to Kampala District and then died. WHO and CDC support was on the ground in Uganda supporting the government response. There were no confirmed cases outside of Uganda.[97] Included among populations confirmed to be affected were prisoners in Kabbale prison. [98] Dr. Joaquim Saweka, the WHO representative to Uganda, reported that the outbreak was under control and that everyone known to have had contact with a known Ebola patient was in isolation.[99]
On 8 August, the Ugandan Ministry of Health recorded 23 probable and confirmed cases, including 16 deaths. Ten cases were confirmed by the Uganda Virus Research Institute as Ebola. 185 people who came into contact with probable and confirmed Ebola cases were followed during the incubation period of 21 days.[100]
On 17 August, the Ministry of Health of the Democratic Republic of the Congo reported an outbreak of the Ebola-Bundibugyo variant[101] in the eastern region.[102] By 21 August, the WHO reported a total of 15 cases and 10 fatalities.[103] No evidence suggested that this outbreak was connected to the Ugandan outbreak.[104] By 13 September 2012, the WHO revealed that the virus had claimed 32 lives and that the probable cause of the outbreak was tainted bush meat hunted by local villagers around the towns of Isiro and Viadana.[105]
2014 outbreak

In February 2014, a strain of the Ebola Virus appeared in Guinea. This is the first Ebola virus outbreak registered in the region. As of April 10, 157 suspected and confirmed cases and 101 deaths had been reported in Guinea, 22 suspected cases in Liberia including 14 deaths, 8 suspected cases in Sierra Leone including 6 deaths, and 1 suspected case in Mali.[106][107] Investigations on these are under way.[108][109][110] By late June 2014 the death toll had reached 390 with over 600 cases reported.[111] By 23 July 2014, the World Health Organization had reported 1201 confirmed cases including 672 deaths since the epidemic began in March.[112] On 31 July 2014, WHO reports the death toll has reached 826 from 1440 cases. [113]
Emory University Hospital was the first US hospital to care for patients exposed to Ebola.[114] Two American medical providers, Kent Brantly and Nancy Writebol, were exposed while treating infected patients in Liberia. Arrangements were made for them to be transported to Emory via speciality aircraft. Emory Hospital has a specially built isolation unit set up in collaboration with the CDC to treat patients exposed to certain serious infectious diseases.[115][116][117] On 2 August 2014 Brantly was flown in to Dobbins Air Force Base in Marietta, Georgia and transferred to Emory Hospital.[118]
History

Ebola virus was first isolated in 1976 during outbreaks of Ebola hemorrhagic fever in Zaire[119] and Sudan.[120] The strain of Ebola that broke out in Zaire has one of the highest case fatality rates of any human virus, roughly 90%.[121]
The name of the disease originates from one of those first recorded outbreaks in 1976 in Yambuku, Democratic Republic of the Congo (then Zaire), which lies on the Ebola River.[119]
While investigating an outbreak of Simian hemorrhagic fever virus (SHFV) in November 1989, an electron microscopist from USAMRIID discovered filoviruses similar in appearance to Ebola in tissue samples taken from crab-eating macaque imported from the Philippines to Hazleton Laboratories Reston, Virginia.[122] Blood samples were taken from 178 animal handlers during the incident.[123] Of those, six animal handlers eventually seroconverted. When the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.[124]
In 1990, Hazelton Research Products' Reston Quarantine Unit in Reston, Virginia suffered a mysterious outbreak of fatal illness among a shipment of crab-eating macaque monkeys imported from the Philippines. The company's veterinary pathologist sent tissue samples from dead animals to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Maryland, where a laboratory test known as an ELISA assay showed antibodies to Ebola virus.
Shortly afterward, a US Army team headquartered at USAMRIID went into action to euthanize the monkeys which had not yet died, bringing those monkeys and those which had already died of the disease to Ft. Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (REBOV) after the location of the incident.[125]
Some scientists also believe that the Plague of Athens, which wiped out about a third of its inhabitants during the Peloponnesian War, may have been caused by Ebola. However, these studies are conflicting, and point to other possible diseases such as typhoid.[126]
Society and culture
Given the lethal nature of Ebola, and since no approved vaccine or treatment is available, it is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use in biological warfare.[127][128]
Other animals
In general, outbreaks of EVD among human populations result from handling infected wild animal carcasses. In general, declines in animal populations precede outbreaks among human populations. Since 2003, such declines have been monitored through surveillance of animal populations with the aim of predicting and preventing EVD outbreaks in humans.[129] Recovered carcasses from gorillas contain multiple Ebola virus strains, which suggest multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoir and animal populations.[130]
Ebola has a high mortality among primates.[131] Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.[132] Outbreaks of EVD may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in 420 square kilometer Lossi Sanctuary between 2002 and 2003.[130] Transmission among chimpanzees through meat consumption constitutes a significant risk factor, while contact between individuals, such as touching dead bodies and grooming is not.[133]
Domestic animals
Ebola virus can be transmitted to dogs and pigs.[134] While dogs may be asymptomatic, pigs tend to develop symptomatic disease.
Research
Medications
Favipiravir looks like it may be useful in a mouse model of the disease.[12] Estrogen receptor drugs used to treat infertility and breast cancer (clomiphene and toremifene) inhibit the progress of Ebola virus in infected mice.[135] Ninety percent of the mice treated with clomiphene and fifty percent of those treated with toremifene survived the tests.[135] Given their oral availability and history of human use, these drugs would be candidates for treating Ebola virus infection in remote geographical locations, either on their own or together with other antiviral drugs.
Human antibodies

During an outbreak 1999 in the Democratic Republic of the Congo, seven of eight people who received blood transfusions from individuals who had previously survived the infection survived themselves.[136] However, this potential treatment is considered controversial.[137] Intravenous antibodies appear to be protective in non-human primates who have been exposed to large doses of ebola.[138]
ZMapp antibody treatment
On August 4, 2014 reports mentioned a promising treatment based on plants, which helped to stabilize and improve the conditions of two American patients, the first two humans to receive this treatment. The treatment drug was referred to as ZMapp, an antibody response related therapy. Based on the initially positive results, ZMapp may offer a cure. ZMapp was produced by MAPP Biopharmaceutical Inc. using a three-mouse monoclonal antibody, manufactured in genetically modified tobacco plants (of the genus Nicotiana).[139][140] In the three-mouse drug production process, mice were exposed to three different fragments of the virus strain and antibodies were harvested to create the medicine.[141][142]
Other treatments
Other promising treatments rely on antisense technology.
RNA interference
Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the Zaire Ebola virus (ZEBOV) RNA polymerase L protein could prevent disease in nonhuman primates.[143][144]
References
- ^ a b c d e f g h i j k l m n "Ebola virus disease Fact sheet N°103". World Health Organization. March 2014. Retrieved 12 April 2014.
- ^ a b "2014 Ebola Virus Disease (EVD) outbreak in West Africa". WHO. Apr 21 2014. Retrieved 3 August 2014.
{{cite web}}: Check date values in:|date=(help) - ^ a b C.M. Fauquet (2005). Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses. Oxford: Elsevier/Academic Press. p. 648. ISBN 9780080575483.
- ^ a b "Ebola Viral Disease Outbreak — West Africa, 2014". CDC. June 27, 2014. Retrieved 26 June 2014.
- ^ a b c d "CDC urges all US residents to avoid nonessential travel to Liberia, Guinea, and Sierra Leone because of an unprecedented outbreak of Ebola". CDC. July 31, 2014. Retrieved 2 August 2014.
- ^ Ebola Hemorrhagic Fever from Centers for Disease Control and Prevention.P age last updated: January 28, 2014.
- ^ a b c Gatherer D (2014). "The 2014 Ebola virus disease outbreak in West Africa". J. Gen. Virol. 95 (Pt 8): 1619–1624. doi:10.1099/vir.0.067199-0. PMID 24795448.
- ^ a b c d "Ebola Hemorrhagic Fever Signs and Symptoms". CDC. January 28, 2014. Retrieved 2 August 2014.
- ^ a b c Hoenen T, Groseth A, Falzarano D, Feldmann H (May 2006). "Ebola virus: unravelling pathogenesis to combat a deadly disease". Trends in Molecular Medicine. 12 (5): 206–215. doi:10.1016/j.molmed.2006.03.006. PMID 16616875.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Ebola Virus, Clinical Presentation". Medscape. Retrieved 2012-07-30.
- ^ Fisher-Hoch SP, Platt GS, Neild GH, Southee T, Baskerville A, Raymond RT, Lloyd G, Simpson DI (1985). "Pathophysiology of shock and hemorrhage in a fulminating viral infection (Ebola)". J. Infect. Dis. 152 (5): 887–894. doi:10.1093/infdis/152.5.887. PMID 4045253.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c Gatherer, D (2014 Aug). "The 2014 Ebola virus disease outbreak in West Africa". The Journal of general virology. 95 (Pt 8): 1619–1624. PMID 24795448.
{{cite journal}}: Check date values in:|date=(help) - ^ "Ebola Hemorrhagic Fever Risk of Exposure". CDC. August 1, 2014. Retrieved 2 August 2014.
- ^ a b c "Ebola Hemorrhagic Fever Prevention". CDC. July 31, 2014. Retrieved 2 August 2014.
- ^ a b "CDC Telebriefing on Ebola outbreak in West Africa". CDC. July 28, 2014. Retrieved 3 August 2014.
- ^ Jaax N, Jahrling P, Geisbert T, Geisbert J, Steele K, McKee K, Nagley D, Johnson E, Jaax G, Peters C (Dec 1995). "Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory". Lancet. 346 (8991–8992): 1669–1671. doi:10.1016/S0140-6736(95)92841-3. ISSN 0140-6736. PMID 8551825.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jaax NK, Davis KJ, Geisbert TJ, Vogel P, Jaax GP, Topper M, Jahrling PB (Feb 1996). "Timed appearance of lymphocytic choriomeningitis virus after gastric inoculation of mice". Archives of pathology & laboratory medicine. 120 (2): 140–155. ISSN 0003-9985. PMID 8712894.
{{cite journal}}:|first2=missing|last2=(help);|first3=missing|last3=(help);|first4=missing|last4=(help);|first5=missing|last5=(help);|first6=missing|last6=(help);|first7=missing|last7=(help)CS1 maint: multiple names: authors list (link) - ^ Harden, Blaine (2001-02-18). "Dr. Matthew's Passion". New York Times Magazine. Retrieved 2008-02-25.
- ^ Mayo Clinic Staff, Ebola virus and Marburg virus: Causes, Mayo Clinic
- ^ Lashley, edited by Felissa R.; Durham, Jerry D. (2007). Emerging infectious diseases trends and issues (2nd ed. ed.). New York: Springer Pub. Co. p. 141. ISBN 9780826103505.
{{cite book}}:|edition=has extra text (help);|first1=has generic name (help) - ^ Johnson E, Jaax N, White J, Jahrling P (Aug 1995). "Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus". International journal of experimental pathology. 76 (4): 227–236. ISSN 0959-9673. PMC 1997182. PMID 7547435.
{{cite journal}}:|first2=missing|last2=(help);|first3=missing|last3=(help);|first4=missing|last4=(help)CS1 maint: multiple names: authors list (link) - ^ Leffel EK, Reed DS (2004). "Marburg and Ebola viruses as aerosol threats". Biosecurity and bioterrorism : biodefense strategy, practice, and science. 2 (3): 186–191. doi:10.1089/bsp.2004.2.186. ISSN 1538-7135. PMID 15588056.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G (2012). "Transmission of Ebola virus from pigs to non-human primates". Sci Rep. 2: 811. doi:10.1038/srep00811. PMC 3498927. PMID 23155478.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gonzalez JP, Pourrut X, Leroy E (2007). "Ebolavirus and other filoviruses". Current topics in microbiology and immunology. Current Topics in Microbiology and Immunology. 315: 363–387. doi:10.1007/978-3-540-70962-6_15. ISBN 978-3-540-70961-9. PMID 17848072.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Williams E. "African monkey meat that could be behind the next HIV". Health News - Health & Families. The Independent.
25 people in Bakaklion, Cameroon killed due to eating of ape
- ^ "Fruit bats may carry Ebola virus". BBC News. 2005-12-11. Retrieved 2008-02-25.
- ^ a b c Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, Nkoghe D, Gonzalez JP, Leroy EM (2005). "The natural history of Ebola virus in Africa". Microbes and infection / Institut Pasteur. 7 (7–8): 1005–1014. doi:10.1016/j.micinf.2005.04.006. PMID 16002313.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ (Oct 1996). "Experimental inoculation of plants and animals with Ebola virus". Emerging Infectious Diseases. 2 (4): 321–325. doi:10.3201/eid0204.960407. ISSN 1080-6040. PMC 2639914. PMID 8969248.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, Délicat A, Paweska JT, Gonzalez JP, Swanepoel R (2005). "Fruit bats as reservoirs of Ebola virus". Nature. 438 (7068): 575–576. Bibcode:2005Natur.438..575L. doi:10.1038/438575a. PMID 16319873.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pourrut X, Délicat A, Rollin PE, Ksiazek TG, Gonzalez JP, Leroy EM (2007). "Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species". The Journal of infectious diseases. Suppl 2 (s2): S176–S183. doi:10.1086/520541. PMID 17940947.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Starkey, Jerome (5 April 2014) 90 killed as fruit bats spread Ebola virus across West Africa The Times (subscription may be needed), Retrieved 5 April 2014
- ^ Olival KJ, Islam A, Yu M, Anthony SJ, Epstein JH, Khan SA, Khan SU, Crameri G, Wang LF, Lipkin WI, Luby SP, Daszak P (2013). "Ebola virus antibodies in fruit bats, bangladesh". Emerging Infect. Dis. 19 (2): 270–3. doi:10.3201/eid1902.120524. PMC 3559038. PMID 23343532.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Morvan JM, Deubel V, Gounon P, Nakouné E, Barrière P, Murri S, Perpète O, Selekon B, Coudrier D, Gautier-Hion A, Colyn M, Volehkov V (1999). "Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic". Microbes and Infection. 1 (14): 1193–1201. doi:10.1016/S1286-4579(99)00242-7. PMID 10580275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Peterson AT, Bauer JT, Mills JN (2004). "Ecologic and Geographic Distribution of Filovirus Disease". Emerging Infectious Diseases. 10 (1): 40–47. doi:10.3201/eid1001.030125. PMC 3322747. PMID 15078595.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.bbc.co.uk/news/world-africa-26735118
- ^ Pringle, C. R. (2005). "Order Mononegavirales". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 609–614. ISBN 0-12-370200-3Template:Inconsistent citations
{{cite book}}: Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ a b Kiley MP, Bowen ET, Eddy GA, Isaäcson M, Johnson KM, McCormick JB, Murphy FA, Pattyn SR, Peters D, Prozesky OW, Regnery RL, Simpson DI, Slenczka W, Sureau P, van der Groen G, Webb PA, Wulff H (1982). "Filoviridae: A taxonomic home for Marburg and Ebola viruses?". Intervirology. 18 (1–2): 24–32. doi:10.1159/000149300. PMID 7118520.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Geisbert TW, Jahrling PB (1995). "Differentiation of filoviruses by electron microscopy". Virus research. 39 (2–3): 129–150. PMID 8837880.
- ^ Feldmann, H.; Geisbert, T. W.; Jahrling, P. B.; Klenk, H.-D.; Netesov, S. V.; Peters, C. J.; Sanchez, A.; Swanepoel, R.; Volchkov, V. E. (2005). "Family Filoviridae". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 645–653. ISBN 0-12-370200-3Template:Inconsistent citations
{{cite book}}: Invalid|display-authors=9(help); Invalid|ref=harv(help)CS1 maint: postscript (link) - ^ Smith, Tara (2005). Ebola (Deadly Diseases and Epidemics). Chelsea House Publications. ISBN 0-7910-8505-8.
- ^ Sullivan N, Yang ZY, Nabel GJ (2003). "Ebola Virus Pathogenesis: Implications for Vaccines and Therapies" (Free full text). Journal of Virology. 77 (18): 9733–9737. doi:10.1128/JVI.77.18.9733-9737.2003. PMC 224575. PMID 12941881.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Ebola Hemorrhagic Fever Diagnosis". CDC. January 28, 2014. Retrieved 3 August 2014.
- ^ Grolla A, Lucht A, Dick D, Strong JE, Feldmann H (2005). "Laboratory diagnosis of Ebola and Marburg hemorrhagic fever". Bull Soc Pathol Exot. 98 (3): 205–9. PMID 16267962.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Büchen-Osmond, Cornelia (2006-04-25). "ICTVdB Virus Description – 01.025.0.02. Ebolavirus". International Committee on Taxonomy of Viruses. Retrieved 2009-06-02.
- ^ Suzuki Y, Gojobori T (1997). "The origin and evolution of Ebola and Marburg viruses". Molecular Biology and Evolution. 14 (8): 800–6. PMID 9254917.
- ^ Taylor DJ, Leach RW, Bruenn J (2010). "Filoviruses are ancient and integrated into mammalian genomes". BMC Evolutionary Biology. 10: 193. doi:10.1186/1471-2148-10-193. PMC 2906475. PMID 20569424.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Taylor DJ, Dittmar K, Ballinger MJ, Bruenn JA (2011). "Evolutionary maintenance of filovirus-like genes in bat genomes". BMC Evolutionary Biology. 11: 336. doi:10.1186/1471-2148-11-336. PMC 3229293. PMID 22093762.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Longo, DL; Kasper, DL; Jameson, JL; Fauci, AS; Hauser, SL; Loscalzo, J, eds. (2012). "Chapter 197". Harrison's Principles of Internal Medicine (18th ed.). McGraw-Hill. ISBN 0-07-174889-X.
- ^ Gear JH (1989). "Clinical aspects of African viral hemorrhagic fevers". Reviews of infectious diseases. 11 Suppl 4: S777–S782. PMID 2665013.
- ^ Gear JH, Ryan J, Rossouw E (1978). "A consideration of the diagnosis of dangerous infectious fevers in South Africa". South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 53 (7): 235–237. PMID 565951.
{{cite journal}}: Missing pipe in:|journal=(help)CS1 maint: multiple names: authors list (link) - ^ Grolla A, Lucht A, Dick D, Strong JE, Feldmann H (2005). "Laboratory diagnosis of Ebola and Marburg hemorrhagic fever". Bulletin de la Societe de pathologie exotique (1990). 98 (3): 205–209. PMID 16267962.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bogomolov BP (1998). "Differential diagnosis of infectious diseases with hemorrhagic syndrome". Terapevticheskii arkhiv. 70 (4): 63–68. PMID 9612907.
- ^ a b Centers for Disease Control and Prevention and World Health Organization (1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting (PDF). Atlanta, Georgia, US: Centers for Disease Control and Prevention. Retrieved 2013-02-08.
- ^ Ebola Virus: Symptoms, Treatment, and Prevention
- ^ Sompayrac, Lauren (2002). How pathogenic viruses work (3. print. ed.). Boston: Jones and Bartlett Publishers. p. 87. ISBN 9780763720827.
- ^ Alazard-Dany, N; Ottmann Terrangle, M; Volchkov, V (2006 Apr). "[Ebola and Marburg viruses: the humans strike back]". Medecine sciences : M/S. 22 (4): 405–10. PMID 16597410.
{{cite journal}}: Check date values in:|date=(help) - ^ Special Pathogens Branch CDC (2008-01-14). "Known Cases and Outbreaks of Ebola Hemorrhagic Fever". Center for Disease Control and Prevention. Retrieved 2008-08-02.
- ^ Schultz, edited by Kristi Koenig, Carl (2009). Koenig and Schultz's disaster medicine : comprehensive principles and practices. Cambridge: Cambridge University Press. p. 209. ISBN 9780521873673.
{{cite book}}:|first1=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Lewis1, David (Jul 30, 2014). "Liberia shuts schools, considers quarantine to curb Ebola". Reuters. Retrieved 3 August 2014.
{{cite news}}: CS1 maint: numeric names: authors list (link) - ^ Hoenen T, Groseth A, Feldmann H (2012). "Current ebola vaccines". Expert Opinion on Biological Therapy. 12 (7): 859–72. doi:10.1517/14712598.2012.685152. PMC 3422127. PMID 22559078.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Choi JH, Croyle MA (2013). "Emerging targets and novel approaches to Ebola virus prophylaxis and treatment". BioDrugs. 27 (6): 565–83. doi:10.1007/s40259-013-0046-1. PMID 23813435.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Xu L, Sanchez A, Yang Z, Zaki SR, Nabel EG, Nichol ST, Nabel GJ (1998). "Immunization for Ebola virus infection". Nature Medicine. 4 (1): 37–42. doi:10.1038/nm0198-037. PMID 9427604.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang ZY, Roederer M, Koup RA, Jahrling PB, Nabel GJ (2003). "Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates". Nature. 424 (6949): 681–684. doi:10.1038/nature01876. PMID 12904795.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Ströher U, Fritz EA, Hensley LE, Jones SM, Feldmann H (2008). "Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses". Vaccine. 26 (52): 6894–6900. doi:10.1016/j.vaccine.2008.09.082. PMC 3398796. PMID 18930776.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Geisbert TW, Daddario-Dicaprio KM, Lewis MG, Geisbert JB, Grolla A, Leung A, Paragas J, Matthias L, Smith MA, Jones SM, Hensley LE, Feldmann H, Jahrling PB (2008). Kawaoka, Yoshihiro (ed.). "Vesicular Stomatitis Virus-Based Ebola Vaccine is Well-Tolerated and Protects Immunocompromised Nonhuman Primates". PLoS Pathogens. 4 (11): e1000225. doi:10.1371/journal.ppat.1000225. PMC 2582959. PMID 19043556.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H (2009). "Single-Injection Vaccine Protects Nonhuman Primates against Infection with Marburg Virus and Three Species of Ebola Virus". Journal of Virology. 83 (14): 7296–7304. doi:10.1128/JVI.00561-09. PMC 2704787. PMID 19386702.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S (2007). "Ebola Virus‐Like Particle–Based Vaccine Protects Nonhuman Primates against Lethal Ebola Virus Challenge". The Journal of Infectious Diseases. 196: S430–S437. doi:10.1086/520583. PMID 17940980.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Oplinger, Anne A. (2003-11-18). NIAID Ebola vaccine enters human trial. Bio-Medicine.
- ^ a b "Ebola/Marburg Vaccine Development" (Press release). National Institute of Allergy and Infectious Diseases. 2008-09-15.
- ^ Martin JE, Sullivan NJ, Enama ME, Gordon IJ, Roederer M, Koup RA, Bailer RT, Chakrabarti BK, Bailey MA, Gomez PL, Andrews CA, Moodie Z, Gu L, Stein JA, Nabel GJ, Graham BS (2006). "A DNA Vaccine for Ebola Virus is Safe and Immunogenic in a Phase I Clinical Trial". Clinical and Vaccine Immunology. 13 (11): 1267–1277. doi:10.1128/CVI.00162-06. PMC 1656552. PMID 16988008.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bush, L (2005). "Crucell and NIH sign Ebola vaccine manufacturing contract". Pharmaceutical Technology. 29: 28.
{{cite journal}}: Cite has empty unknown parameter:|1=(help); Invalid|ref=harv(help) - ^ Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW (2005). "Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses". Nature Medicine. 11 (7): 786–790. doi:10.1038/nm1258. PMID 15937495.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Phoolcharoen W, Dye JM, Kilbourne J, Piensook K, Pratt WD, Arntzen CJ, Chen Q, Mason HS, Herbst-Kralovetz MM (2011). "A nonreplicating subunit vaccine protects mice against lethal Ebola virus challenge". Proc. Natl. Acad. Sci. U.S.A. 108 (51): 20695–700. Bibcode:2011PNAS..10820695P. doi:10.1073/pnas.1117715108. PMC 3251076. PMID 22143779.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Canadian Press". CBCNews. Canadian Broadcasting Corporation (CBC). 20 March 2009. Retrieved 2 August 2014.
- ^ Tuffs A (2009). "Experimental vaccine may have saved Hamburg scientist from Ebola fever". BMJ. 338: b1223. doi:10.1136/bmj.b1223. PMID 19307268.
- ^ Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Ströher U, Grolla A, Bray M, Fritz EA, Fernando L, Feldmann F, Hensley LE, Geisbert TW (2007). "Effective Post-Exposure Treatment of Ebola Infection". PLoS Pathogens. 3 (1): e2. doi:10.1371/journal.ppat.0030002. PMC 1779298. PMID 17238284.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Geisbert TW, Daddario-DiCaprio KM, Williams KJ, Geisbert JB, Leung A, Feldmann F, Hensley LE, Feldmann H, Jones SM (2008). "Recombinant Vesicular Stomatitis Virus Vector Mediates Postexposure Protection against Sudan Ebola Hemorrhagic Fever in Nonhuman Primates". Journal of Virology. 82 (11): 5664–5668. doi:10.1128/JVI.00456-08. PMC 2395203. PMID 18385248.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bausch DG, Feldmann H, Geisbert TW, Bray M, Sprecher AG, Boumandouki P, Rollin PE, Roth C (2007). "Outbreaks of Filovirus Hemorrhagic Fever: Time to Refocus on the Patient". The Journal of Infectious Diseases. 196: S136–S141. doi:10.1086/520542. PMID 17940941.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jeffs B (2006). "A clinical guide to viral haemorrhagic fevers: Ebola, Marburg and Lassa". Tropical Doctor. 36 (1): 1–4. doi:10.1258/004947506775598914. PMID 16483416.
- ^ Nkoghé D, Formenty P, Nnégué S, Mvé MT, Hypolite I, Léonard P, Leroy E (2004). "Practical guidelines for the management of Ebola infected patients in the field". Medecine tropicale : revue du Corps de sante colonial. 64 (2): 199–204. PMID 15460155.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Sierra Leone Is Epicenter of Ebola as Guinea Clinic Shut". 2014-06-08. Retrieved 2014-07-30.
- ^ http://www.cnn.com/2014/08/04/health/experimental-ebola-serum/index.html?hpt=hp_t2
- ^ "Ebola Outbreak Confirmed in Congo". NewScientist.com. 2007-09-11. Retrieved 2008-02-25.
- ^ Ebola outbreak in Congo. CDC news. 2007-09-12. Retrieved 2009-05-31.
- ^ "Mystery DR Congo fever kills 100". BBC News. 2007-08-31. Retrieved 2008-02-25.
- ^ "Uganda: Deadly Ebola Outbreak Confirmed – UN". UN News Service. 2007-11-30. Retrieved 2008-02-25.
- ^ The IV International Symposium on Filoviruses. l'Institut de recherche pour le développement (IRD). Retrieved 2009-0-31.
{{cite book}}: Check date values in:|accessdate=(help) - ^ World Health Organization (2008-12-27). RD Congo: Fièvre hémorragique à virus Ebola au Kasaï Occidental, Rapport de situation No 1 des 26 & 27 décembre 2008 (in French). Relief Web. Retrieved 2009-06-02.
- ^ "DR Congo: Ebola Outbreak Confirmed, 9 Deaths". December 25, 2008. Retrieved 3 August 2014.
- ^ Ebola alert shuts Angolan border. BBC. 2009-01-06. Retrieved 2009-05-31.
- ^ Eddyn, Melissan (2009-03-27). "Scientist Injects Self With Ebola". Associated Press. Retrieved 2009-05-02.
- ^ Malone, Barry (2011-06-17). "Uganda says Ebola outbreak is over". Reuters. Retrieved 2011-07-06.
- ^ "Congo (DRC): Bushmeat blamed for Ebola outbreak". Norwegian Council for Africa. 2012-08-24. Retrieved 2013-04-15.
- ^ "Outbreak of Ebola in Uganda kills 13". BBC News. July 28, 2012.
- ^ Muhumuza R (2012-07-28). "Officials: Uganda Ebola outbreak kills 14". Health. MSNBC. Retrieved 2013-04-15.
- ^ "Ebola Outbreak Spreads". Associated Press – The Express. July 31, 2012.
{{cite news}}:|access-date=requires|url=(help) - ^ "WHO | Ebola in Uganda – update". Who.int. 2012-08-03. Retrieved 2013-04-15.
- ^ McKenzie D (6 August 2012). "Prisoner with suspected case of Ebola escapes from hospital in Uganda". CNN.com.
- ^ Hsu C (2012-08-03). "WHO: Ebola Outbreak in Uganda is Under Control". US/World. Medical Daily. Retrieved 2013-04-15.
- ^ "Ebola in Uganda – update". WHO. Retrieved 2012-08-10.
- ^ "DRC Confirms Ebola Outbreak". Voanews.com. Retrieved 2013-04-15.
- ^ "WHO | Ebola outbreak in Democratic Republic of Congo". Who.int. 2012-08-17. Retrieved 2013-04-15.
- ^ "WHO | Ebola outbreak in Democratic Republic of Congo – update". Who.int. 2012-08-21. Retrieved 2013-04-15.
- ^ "Ebola outbreak in DRC – Disaster News Network". Disasternews.net. 2012-08-22. Retrieved 2013-04-15.
- ^ Castillo M (2012). "Ebola virus claims 31 lives in Democratic Republic of the Congo". United States: CBS News. Retrieved 14 September 2012.
{{cite journal}}: Cite journal requires|journal=(help); Invalid|ref=harv(help) - ^ "Outbreak of Ebola in Guinea and Liberia". Centers for Disease Control and Prevention. Retrieved 13 April 2014.
- ^ World Health Organization (2014-04-07). "Ebola virus disease, West Africa (Situation as of 7 April 2014) - Guinea". ReliefWeb.
- ^ "Ebola in West Africa: European Union joins effort to stop spread of disease and releases €500 000 in immediate funding". Press Release. European Commission. 2014-04-28.
- ^ "UN agency urges vigilance amid Ebola outbreak in Guinea, Sierra Leone and Liberia". United Nations News Centre.
- ^ Silver M (2013-03-27). "Why Is This Ebola Outbreak Spreading?". National Geographic.
- ^ WHO warns drastic action needed to combat Ebola outbreak | Big News Network.com
- ^ "Ebola virus disease, West Africa – update 25 July 2014". WHO: Outbreak news. World Health Organization. 2014-07-25. Retrieved 2014-07-30.
- ^ http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4238-ebola-virus-disease-west-africa-31-july-2014.html WHO - Ebola virus disease, West Africa – update 31 July 2014
- ^ "Emory Healthcare statement and letter to the Emory Community". Emory Healthcare Statement. Emory University. 2014-08-01.
- ^ Stanglin D (2014-08-01). "2 American Ebola patients head to USA". USA Today.
- ^ Botelho G, Brumfield B, Carter CJ (2014-08-02). "Ebola coming to U.S, as Atlanta hospital prepares". CNN.com.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Harf M (2014-08-01). "Medical Evacuations of Two U.S. Citizens From West Africa". Press Statement. U.S. Department of State.
- ^ "US allays Ebola fears as doctors flown home for treatment". Atlanta News.Net. Retrieved 2 August 2014.
{{cite news}}: Italic or bold markup not allowed in:|publisher=(help) - ^ a b Brown R (2014-07-17). "The virus detective who discovered Ebola in 1976". News Magazine. BBC News.
- ^ Bennett D, Brown D (May 1995). "Ebola virus". BMJ (Clinical research ed.). 310 (6991): 1344–1345. doi:10.1136/bmj.310.6991.1344. PMC 2549737. PMID 7787519.
- ^ King JW (2008-04-02). "Ebola Virus". eMedicine. WebMd. Retrieved 2008-10-06.
- ^ McCormick & Fisher-Hoch 1999, pp. 277–279
- ^ Waterman, Tara (1999). Ebola Reston Outbreaks. Stanford University. Retrieved 2008-08-02.
- ^ McCormick & Fisher-Hoch 1999, pp. 298–299
- ^ Preston, Richard (1994). The Hot Zone. New York: Random House. p. 300. ISBN 978-0679437840.
- ^ "Plague of Athens".
- ^ Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K (2002). "Hemorrhagic fever viruses as biological weapons: medical and public health management". Journal of the American Medical Association. 287 (18): 2391–405. doi:10.1001/jama.287.18.2391. PMID 11988060.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Salvaggio MR, Baddley JW (2004). "Other viral bioweapons: Ebola and Marburg hemorrhagic fever". Dermatologic clinics. 22 (3): 291–302, vi. doi:10.1016/j.det.2004.03.003. PMID 15207310.
- ^ Rouquet P, Froment JM, Bermejo M, Kilbourn A, Karesh W, Reed P, Kumulungui B, Yaba P, Délicat A, Rollin PE, Leroy EM (Feb 2005). "Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003" (Free full text). Emerging Infectious Diseases. 11 (2): 283–290. doi:10.3201/eid1102.040533. ISSN 1080-6040. PMC 3320460. PMID 15752448.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Leroy EM, Rouquet P, Formenty P, Souquière S, Kilbourne A, Froment JM, Bermejo M, Smit S, Karesh W, Swanepoel R, Zaki SR, Rollin PE (2004). "Multiple Ebola virus transmission events and rapid decline of central African wildlife". Science. 303 (5656): 387–390. Bibcode:2004Sci...303..387L. doi:10.1126/science.1092528. PMID 14726594.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Choi, JH; Croyle, MA (2013 Dec). "Emerging targets and novel approaches to Ebola virus prophylaxis and treatment". BioDrugs : clinical immunotherapeutics, biopharmaceuticals and gene therapy. 27 (6): 565–83. PMID 23813435.
{{cite journal}}: Check date values in:|date=(help) - ^ Ebola 'kills over 5,000 gorillas'. BBC. 2006-12-08. Retrieved 2009-05-31.
- ^ Formenty P, Boesch C, Wyers M, Steiner C, Donati F, Dind F, Walker F, Le Guenno B (1999). "Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire". The Journal of infectious diseases. 179. Suppl 1 (s1): S120–S126. doi:10.1086/514296. PMID 9988175.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Weingartl HM, Nfon C, Kobinger G (2013). "Review of Ebola virus infections in domestic animals". Dev Biol (Basel). 135: 211–8. doi:10.1159/000178495. PMID 23689899.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Johansen LM, Brannan JM, Delos SE, Shoemaker CJ, Stossel A, Lear C, Hoffstrom BG, Dewald LE, Schornberg KL, Scully C, Lehár J, Hensley LE, White JM, Olinger GG (2013). "FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection". Sci Transl Med. 5 (190): 190ra79. doi:10.1126/scitranslmed.3005471. PMC 3955358. PMID 23785035.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mupapa K, Massamba M, Kibadi K, Kuvula K, Bwaka A, Kipasa M, Colebunders R, Muyembe-Tamfum JJ (1999). "Treatment of Ebola Hemorrhagic Fever with Blood Transfusions from Convalescent Patients". The Journal of Infectious Diseases. 179: S18–S23. doi:10.1086/514298. PMID 9988160.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Feldmann H, Geisbert TW (2011). "Ebola haemorrhagic fever". The Lancet. 377 (9768): 849–862. doi:10.1016/S0140-6736(10)60667-8. PMID 21084112.
- ^ Saphire, EO (2013 Nov). "An update on the use of antibodies against the filoviruses". Immunotherapy. 5 (11): 1221–33. PMID 24188676.
{{cite journal}}: Check date values in:|date=(help) - ^ "Experimental drug likely saved Ebola patients".
- ^ "Local Biotech Increasing Production of 'ZMapp' Ebola Drug".
- ^ "Experimental drug likely saved Ebola patients". CNN. August 4, 2014.
- ^ "Mystery Ebola virus serum manufactured by San Diego firm". Los Angeles Times. August 4, 2014.
- ^ Geisbert TW, Lee AC, Robbins M, Geisbert JB, Honko AN, Sood V, Johnson JC, de Jong S, Tavakoli I, Judge A, Hensley LE, Maclachlan I (2010). "Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: A proof-of-concept study". The Lancet. 375 (9729): 1896–1905. doi:10.1016/S0140-6736(10)60357-1. PMID 20511019.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Warren TK, Warfield KL, Wells J, Swenson DL, Donner KS, Van Tongeren SA, Garza NL, Dong L, Mourich DV, Crumley S, Nichols DK, Iversen PL, Bavari S (2010). "Advanced antisense therapies for postexposure protection against lethal filovirus infections". Nature Medicine. 16 (9): 991–994. doi:10.1038/nm.2202. PMID 20729866.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- Bibliography
- Klenk, Hans-Dieter (January 1999). Marburg and Ebola Viruses (Current Topics in Microbiology and Immunology). Berlin: Springer-Verlag Telos. ISBN 978-3-540-64729-4.
{{cite book}}: CS1 maint: ref duplicates default (link) - Klenk, Hans-Dieter; Feldmann, Heinz (2004). Ebola and Marburg viruses: molecular and cellular biology (Limited preview). Wymondham, Norfolk, UK: Horizon Bioscience. ISBN 978-0-9545232-3-7.
{{cite book}}: CS1 maint: ref duplicates default (link) - Kuhn, Jens H. (2008). Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement, vol. 20 (Limited preview). Vienna: SpringerWienNewYork. ISBN 978-3-211-20670-6.
{{cite book}}: CS1 maint: ref duplicates default (link) - McCormick, Joseph; Fisher-Hoch, Susan (1999) [1996]. Level 4: Virus Hunters of the CDC (Limited preview). Horvitz, Leslie Alan (Updated [3rd] ed.). Barnes & Noble. ISBN 978-0-7607-1208-5.
{{cite book}}: Unknown parameter|month=ignored (help)CS1 maint: ref duplicates default (link) - Pattyn, S. R. (1978). Ebola Virus Haemorrhagic Fever (Full free text) (1st ed.). Amsterdam: Elsevier/North-Holland Biomedical Press. ISBN 0-444-80060-3.
{{cite book}}: CS1 maint: ref duplicates default (link) - Ryabchikova, Elena I.; Price, Barbara B. (2004). Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy. Columbus, Ohio: Battelle Press. ISBN 978-1-57477-131-2.
{{cite book}}: CS1 maint: ref duplicates default (link)
External links
- ViralZone: Ebola-like viruses – Virological repository from the Swiss Institute of Bioinformatics
- CDC: Ebola hemorrhagic fever – Centers for Disease Control and Prevention, Special Pathogens Branch
- WHO: Ebola haemorrhagic fever – World Health Organization, Global Alert and Response
- Virus Pathogen Database and Analysis Resource (ViPR): Filoviridae
- 3D macromolecular structures of the Ebola virus archived in the EM Data Bank(EMDB)
- Google Map of Ebola Outbreaks
- WHO recommended infection control measures
