COVID-19
Template:Use Commonwealth English
| Coronavirus disease 2019 (COVID-19) | |
|---|---|
| Other names | |
 | |
| Symptoms | |
| Pronunciation | |
| Specialty | Acute respiratory infection[6] |
| Symptoms | Fever, cough, shortness of breath[7] |
| Complications | Pneumonia, ARDS, kidney failure |
| Causes | SARS-CoV-2 |
| Diagnostic method | rRT-PCR testing, immunoassay, CT scan |
| Prevention | Correct handwashing technique, cough etiquette, avoiding close contact with sick people |
| Treatment | Symptomatic and supportive |
| Frequency | 676,609,955[8] |
| Deaths | 6,881,955[8] (3.4% of confirmed cases)[9] |
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the virus strain severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).[10] Worldwide spread of the disease began for the first time in 2019 and has developed into the 2019–20 coronavirus pandemic.[11][12] Common symptoms include fever, cough, and shortness of breath. Muscle pain, sputum production and sore throat are some of the less common symptoms.[7][13] While the majority of cases result in mild symptoms,[14] some progress to pneumonia and multi-organ failure.[11][15] The case fatality rate is estimated at between 1% and 5% but varies by age and other health conditions.[16][17][18]
The infection is spread from one person to others via respiratory droplets produced from the airways, often during coughing.[19][20] Time from exposure to onset of symptoms is generally between two and 14 days, with an average of five days.[21][22][23] The standard method of diagnosis is by reverse transcription polymerase chain reaction (rRT-PCR) from a nasopharyngeal swab or sputum sample. Antibody assays can also be used, using a blood serum sample, with results within a few days.[24] The infection can also be diagnosed from a combination of symptoms, risk factors and a chest CT scan showing features of pneumonia.[25][26]
Recommended measures to prevent the disease include frequent hand washing, maintaining distance from other people, and not touching one's face.[27] Covering the nose and mouth with a tissue or a bent elbow when coughing is also considered effective in preventing the spread of the disease.[27] The use of masks is recommended for those who suspect they have the virus and their caregivers, but mask use is not recommended for the general public.[28][29] There is no vaccine or specific antiviral treatment for COVID-19; management involves treatment of symptoms, supportive care, and experimental measures.[30]
The World Health Organization (WHO) has declared the 2019–20 coronavirus outbreak a pandemic[12] and a Public Health Emergency of International Concern (PHEIC).[31][32] Evidence of local transmission of the disease has been found in multiple countries across all six WHO regions.[33]
Signs and symptoms
| Symptom | Percentage |
|---|---|
| Fever | 87.9% |
| Dry cough | 67.7% |
| Fatigue | 38.1% |
| Sputum production | 33.4% |
| Shortness of breath | 18.6% |
| Muscle pain or joint pain | 14.8% |
| Sore throat | 13.9% |
| Headache | 13.6% |
| Chills | 11.4% |
| Nausea or vomiting | 5% |
| Nasal congestion | 4.8% |
| Diarrhoea | 3.7% |
| Haemoptysis | 0.9% |
| Conjunctival congestion | 0.8% |
Those infected with the virus may either be asymptomatic or develop flu-like symptoms that include fever, cough, and shortness of breath.[7][35][36] Diarrhoea and upper respiratory symptoms such as sneezing, runny nose, or sore throat are less common.[37] Cases can progress to pneumonia, multi-organ failure, and death in the most vulnerable.[11][15]
The incubation period ranges from two to 14 days, with an estimated median incubation period of five to six days, according to the World Health Organization (WHO).[38][39]
One study in China found that CT scans showed ground-glass opacities in 56%, but 18% had no radiological findings. 5% were admitted to intensive care units, 2.3% needed mechanical support of ventilation, and 1.4% died.[40] Bilateral and peripheral ground glass opacities are the most typical CT findings.[41] Consolidation, linear opacities, and reverse halo sign are other radiological findings.[41] Initially, the lesions are confined to one lung, but as the disease progresses, indications manifest in both lungs in 88% of people.[41] It has been noted that children seem to have milder symptoms than adults, but this has not been proven.[42]
Cause
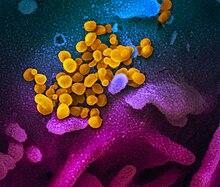
The disease is caused by the virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), previously referred to as the 2019 novel coronavirus (2019-nCoV).[44] It is primarily spread between people via respiratory droplets from coughs and sneezes.[20]
Lungs are the organs most affected by COVID-19 because the virus accesses host cells via the enzyme ACE2, which is most abundant in the type II alveolar cells of the lungs. The virus uses a special surface glycoprotein, called "spike", to connect to ACE2 and intrude the hosting cell.[45] The density of ACE2 in each person is a determinant of the severity of the disease.[46][47]
The virus is thought to have an animal origin.[48] It was first transmitted to humans in Wuhan, China, in November or December 2019, and the primary source of infection became human-to-human transmission by early January 2020.[49][50]
Diagnosis

The WHO has published several testing protocols for the disease.[52][53] The standard method of testing is real-time reverse transcription polymerase chain reaction (rRT-PCR).[54] The test can be done on respiratory samples obtained by various methods, including nasopharyngeal swab or sputum sample.[55] Results are generally available within a few hours to 2 days.[56][57] Blood tests can be used, but these require two blood samples taken two weeks apart and the results have little immediate value.[58] Chinese scientists were able to isolate a strain of the coronavirus and publish the genetic sequence so that laboratories across the world could independently develop polymerase chain reaction (PCR) tests to detect infection by the virus.[11][59][60][61][62][63][64][excessive citations]
COVID-19 testing can also be done with antibody test kits.[65] Antibody assays use a blood serum sample and can provide a positive result even if the person has recovered and the virus is no longer present.[24] The first antibody test was demonstrated by a team at the Wuhan Institute of Virology on 17 February 2020.[66][24] On 25 February, a team from Duke–NUS Medical School in Singapore announced another antibody test for COVID-19 that can provide a result within a few days.[24][67]
Diagnostic guidelines released by Zhongnan Hospital of Wuhan University suggested methods for detecting infections based upon clinical features and epidemiological risk. These involved identifying people who had at least two of the following symptoms in addition to a history of travel to Wuhan or contact with other infected people: fever, imaging features of pneumonia, normal or reduced white blood cell count, or reduced lymphocyte count.[25] A study published by a team at the Tongji Hospital in Wuhan on 26 February 2020 showed that a chest CT scan for COVID-19 has more sensitivity (98%) than the polymerase chain reaction (71%).[26] False negative results may occur due to PCR kit failure, or due to either issues with the sample or issues performing the test. False positive results are likely to be rare.[68]
-
Typical CT imaging findings
-
CT imaging of rapid progression stage
Prevention

Because a vaccine against SARS-CoV-2 is not expected to become available until 2021 at the earliest,[71] a key part of managing the COVID-19 pandemic is trying to decrease the epidemic peak, known as flattening the epidemic curve.[70] This helps decrease the risk of health services being overwhelmed and provides more time for a vaccine and treatment to be developed.[70]
Preventive measures to reduce the chances of infection in locations with an outbreak of the disease are similar to those published for other coronaviruses: stay home, avoid travel and public activities, wash hands with soap and hot water often, practice good respiratory hygiene and avoid touching the eyes, nose, or mouth with unwashed hands.[72][73]
According to the WHO, the use of masks is only recommended if a person is coughing or sneezing or when one is taking care of someone with a suspected infection.[74]
To prevent transmission of the virus, the US Centers for Disease Control and Prevention (CDC) recommends that infected individuals stay home except to get medical care, call ahead before visiting a healthcare provider, wear a face mask when exposed to an individual or location of a suspected infection, cover coughs and sneezes with a tissue, regularly wash hands with soap and water, and avoid sharing personal household items.[75][76] The CDC also recommends that individuals wash hands often with soap and water for at least 20 seconds, especially after going to the toilet or when hands are visibly dirty, before eating and after blowing one's nose, coughing, or sneezing. It further recommended using an alcohol-based hand sanitiser with at least 60% alcohol, but only when soap and water are not readily available.[72] The WHO advises individuals to avoid touching the eyes, nose, or mouth with unwashed hands.[73] Spitting in public places also should be avoided.[77]
Management
There are no antiviral medications specific to COVID-19. Patients are managed with supportive care such as fluid and oxygen support.[79][80] Antiviral drugs are reserved for patients with severe disease.[79] The WHO and National Health Commission have published treatment recommendations for taking care of people who are hospitalised with COVID-19.[81][82] Steroids such as methylprednisolone are not recommended unless the disease is complicated by acute respiratory distress syndrome.[83][84] The CDC recommends that those who suspect they carry the virus wear a facemask.[28]
Management of people infected by the virus includes taking precautions while applying therapeutic manoeuvres, especially when performing procedures like intubation or hand ventilation that can generate aerosols.[85]
Technology
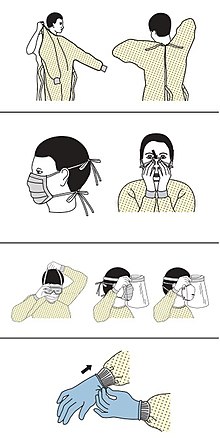
The CDC outlines the specific personal protective equipment and the order in which healthcare providers should put it on when dealing with someone who may have COVID-19: 1) gown, 2) mask or respirator, 3) goggles or a face shield, 4) gloves.[86][87]
In February 2020, China has launched a mobile app to deal with the disease outbreak.[88] Users are asked to enter their name and ID number. The app is able to detect 'close contact' using surveillance data and therefore a potential risk of infection. Every user can also check the status of three other users. If a potential risk is detected, the app not only recommends self-quarantine, it also alerts local health officials.[89]
Research
The WHO recommended volunteers take part in trials of the effectiveness and safety of potential treatments.[90] There is tentative evidence for remdesivir as of March 2020.[91] Lopinavir/ritonavir is also being studied in China.[92] Chloroquine was being trialled in China in February 2020, with preliminary results that seem positive.[93] Nitazoxanide has been recommended for further in vivo study after demonstrating low concentration inhibition of SARS-CoV-2.[94]
Psychological
Infected individuals may experience distress from quarantine, travel restrictions, side effects of treatment, or fear of the infection itself. To address these concerns, the National Health Commission of China published a national guideline for psychological crisis intervention on 27 January 2020.[95][96]
Prognosis

Many of those who die of COVID-19 have preexisting conditions, including hypertension, diabetes and cardiovascular disease.[98] In a study of early cases, the median time from exhibiting initial symptoms to death was 14 days, with a full range of six to 41 days.[99] In a study by the National Health Commission (NHC) of China, men had a death rate of 2.8% while women had a death rate of 1.7%.[16] In those under the age of 50 the risk of death is less than 0.5%, while in those over the age of 70 it is more than 8%.[16] No deaths had occurred in patients under the age of 10 as of 26 February 2020[update].[16] Availability of medical resources and the socioeconomics of a region may also affect mortality.[100]
Histopathological examinations of post-mortem lung samples showed diffuse alveolar damage with cellular fibromyxoid exudates in both lungs. Viral cytopathic changes were observed in the pneumocytes. The lung picture resembled acute respiratory distress syndrome (ARDS).[101]
Epidemiology
Overall mortality and morbidity rates due to infection are not well established; while the case fatality rate (CFR) changes over time in the current outbreak, the proportion of infections that progress to diagnosable disease remains unclear.[102][103] However, preliminary research has yielded case fatality rate numbers between 2% and 3%;[17] in January 2020 the WHO suggested that the case fatality rate was approximately 3%,[104] and 2% in February 2020 in Hubei.[105] Other CFR numbers, which adjust for differences in time of confirmation, death or cured, are respectively 7%[106] and 33% for people in Wuhan 31 January.[107] An unreviewed preprint study by Imperial College London among 55 fatal cases noted that early estimates of mortality may be too high as asymptomatic infections are missed. They estimated a mean infection fatality ratio (IFR, the mortality among infected) ranging from 0.8% when including asymptomatic carriers to 18% when including only symptomatic cases from Hubei province.[108] Pauline Vetter, in an editorial in The BMJ noted that mortality outside of Hubei province seems to be lower than within Hubei.[83] The outbreak in 2019–2020 has caused at least 676,609,955Template:Edit sup[8] confirmed infections and 6,881,955Template:Edit sup[8] deaths.
An observational study of nine people, found no intrauterine vertical transmission from mother to the newborn.[109] Also, a descriptive study in Wuhan found no evidence of viral transmission through vaginal sex (from female to partner), but authors note that transmission during sex might occur through other routes.[110]
Research
Because of its key role in the transmission and progression of the disease, ACE2 has been the focus of a significant proportion of research and various therapeutic approaches have been suggested.[47]
Vaccine
There is no available vaccine, but research into developing a vaccine has been undertaken by various agencies. Previous work on SARS-CoV is being utilised because SARS-CoV-2 and SARS-CoV both use ACE2 enzyme to invade human cells.[111] There are three vaccination strategies being investigated. First, researchers aim to build a whole virus vaccine. The use of such a virus, be it inactive or dead, aims for a prompt immune response of the human body to a new infection with COVID-19. A second strategy, subunit vaccines, aims to create a vaccine that sensitises the immune system to certain subunits of the virus. In the case of SARS-CoV-2 such research focuses on the S-spike protein that helps the virus intrude the ACE2 enzyme. A third strategy is the nucleic acid vaccines (DNA or RNA vaccines, a novel technique for creating a vaccination). Experimental vaccines from any of these strategies would have to be tested for safety and efficacy.[112]
Antiviral
No drug has yet been approved to treat coronavirus infections in humans by the WHO although some are recommended by the Korean and Chinese medical authorities.[113] Trials of many antivirals has been started in patients with COVID-19 including oseltamivir, lopinavir/ritonavir, ganciclovir, favipiravir, baloxavir marboxil, umifenovir, interferon alfa but currently there are no data to support their use.[114] The Koreans recommend lopinavir/ritonavir or chloroquine[115] and the Chinese 7th edition guidelines include interferon, lopinavir/ritonavir, ribavirin, chloroquine and/or umifenovir.[116]
Research into potential treatments for the disease was initiated in January 2020, and several antiviral drugs are already in clinical trials.[117][118] Although completely new drugs may take until 2021 to develop,[119] several of the drugs being tested are already approved for other antiviral indications, or are already in advanced testing.[113]
Remdesivir and chloroquine effectively inhibit the coronavirus in vitro.[94] Remdesivir is being trialled in USA and in China.[114]
Preliminary results from a multicentric trial, announced in a press conference and described by Gao, Tian and Yang, suggested that chloroquine is effective and safe in treating COVID-19 associated pneumonia, "improving lung imaging findings, promoting a virus-negative conversion, and shortening the disease course".[93]
Recent studies have demonstrated that initial spike protein priming by transmembrane protease serine 2 (TMPRSS2) is essential for entry of SARS-CoV-2, SARS-CoV, and MERS-CoV via interaction with the ACE2 receptor.[120][121] These findings suggest that the TMPRSS2 inhibitor Camostat approved for clinical use in Japan for inhibiting fibrosis in liver and kidney disease, postoperative reflux esophagitis, and pancreatitis might constitute an effective off-label treatment option.[120]
Terminology
The process of naming the disease has been called "chaotic".[122]
The World Health Organisation announced on 11 February 2020 that "COVID-19" will be the official name of the disease. World Health Organisation chief Tedros Adhanom Ghebreyesus said "co" stands for "corona", "vi" for "virus" and "d" for "disease", while "19" was for the year, as the outbreak was first identified on 31 December 2019. Tedros said the name had been chosen to avoid references to a specific geographical location (i.e. China), animal species, or group of people in line with international recommendations for naming aimed at preventing stigmatisation.[123][124]
See also
- Coronavirus diseases, a group of closely related syndromes
- Li Wenliang, a doctor at Central Hospital of Wuhan and the first to describe the syndrome, from which he later died
References
- ^ 国家卫生健康委关于新型冠状病毒肺炎暂命名事宜的通知 (in Chinese (China)). National Health Commission. 7 February 2020. Archived from the original on 28 February 2020. Retrieved 9 February 2020.
- ^ Belluz, Julia (20 January 2020). "Wuhan pneumonia outbreak: What we know and don't know". Vox. Archived from the original on 13 January 2020. Retrieved 27 February 2020.
- ^ Cheung, Elizabeth (17 January 2020). "Wuhan pneumonia: Hong Kong widens net for suspected cases but medical workers fear already overstretched hospitals will suffer". South China Morning Post. Archived from the original on 21 January 2020. Retrieved 27 February 2020.
- ^ Chan, Jasper Fuk-Woo; Yuan, Shuofeng; Kok, Kin-Hang; To, Kelvin Kai-Wang; Chu, Hin; Yang, Jin; Xing, Fanfan; Liu, Jieling; Yip, Cyril Chik-Yan; Poon, Rosana Wing-Shan; Tsoi, Hoi-Wah; Lo, Simon Kam-Fai; Chan, Kwok-Hung; Poon, Vincent Kwok-Man; Chan, Wan-Mui; Ip, Jonathan Daniel; Cai, Jian-Piao; Cheng, Vincent Chi-Chung; Chen, Honglin; Hui, Christopher Kim-Ming; Yuen, Kwok-Yung (15 February 2020). "A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster". The Lancet. 395 (10223) (published 24 January 2020): 514–523. doi:10.1016/S0140-6736(20)30154-9. ISSN 0140-6736. PMID 31986261.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ "Wuhan designates hospitals for viral pneumonia treatment as cases rise". The Straits Times. 21 January 2020. Archived from the original on 21 January 2020. Retrieved 27 February 2020.
- ^ See SARS-CoV-2 for more.
- ^ a b c "Coronavirus Disease 2019 (COVID-19) Symptoms". Centers for Disease Control and Prevention. United States. 10 February 2020. Archived from the original on 30 January 2020.
- ^ a b c d "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. Johns Hopkins University. Retrieved 10 March 2023.
- ^ https://www.livescience.com/why-italy-coronavirus-deaths-so-high.html
- ^ "Naming the coronavirus disease (COVID-19) and the virus that causes it". www.who.int. World Health Organization. Archived from the original on 28 February 2020. Retrieved 28 February 2020.
- ^ a b c d Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, Ippolito G, Mchugh TD, Memish ZA, Drosten C, Zumla A, Petersen E. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020 Jan 14;91:264–266. doi:10.1016/j.ijid.2020.01.009. PMID 31953166.

- ^ a b "WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020". World Health Organization (WHO) (Press release). 11 March 2020. Retrieved 12 March 2020.
{{cite press release}}: CS1 maint: url-status (link) - ^
"Q&A on coronaviruses (COVID-19)". World Health Organization. Retrieved 11 March 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Wang, Vivian (5 March 2020). "Most Coronavirus Cases Are Mild. That's Good and Bad News" – via NYTimes.com.
- ^ a b "Q&A on coronaviruses". World Health Organization (WHO). Archived from the original on 20 January 2020. Retrieved 27 January 2020.
- ^ a b c d "Coronavirus Age, Sex, Demographics (COVID-19) - Worldometer". www.worldometers.info. Archived from the original on 27 February 2020. Retrieved 26 February 2020.
- ^ a b "Wuhan Coronavirus Death Rate - Worldometer". www.worldometers.info. Archived from the original on 31 January 2020. Retrieved 2 February 2020.
- ^ "Report 4: Severity of 2019-novel coronavirus (nCoV)" (PDF). Archived (PDF) from the original on 10 February 2020. Retrieved 10 February 2020.
- ^ "Q&A on coronaviruses". World Health Organization (WHO). 11 February 2020. Archived from the original on 20 January 2020. Retrieved 24 February 2020.
The disease can spread from person to person through small droplets from the nose or mouth which are spread when a person with COVID-19 coughs or exhales ... The main way the disease spreads is through respiratory droplets expelled by someone who is coughing.
- ^ a b "2019 Novel Coronavirus (2019-nCoV)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 7 March 2020. Retrieved 18 February 2020.
The virus is thought to spread mainly from person-to-person ... through respiratory droplets produced when an infected person coughs or sneezes.
- ^ "Symptoms of Novel Coronavirus (2019-nCoV) | CDC". www.cdc.gov. 10 February 2020. Archived from the original on 30 January 2020. Retrieved 11 February 2020.
- ^ Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR (February 2020). "Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges". International Journal of Antimicrobial Agents: 105924. doi:10.1016/j.ijantimicag.2020.105924. PMID 32081636.
- ^ Velavan, Thirumalaisamy P.; Meyer, Christian G. (2020). "The COVID-19 epidemic". Tropical Medicine & International Health. n/a (n/a): 278–280. doi:10.1111/tmi.13383. ISSN 1365-3156. PMID 32052514.
- ^ a b c d Normile, Dennis; 2020; Pm, 4:30 (27 February 2020). "Singapore claims first use of antibody test to track coronavirus infections". Science | AAAS. Retrieved 2 March 2020.
{{cite web}}:|last2=has numeric name (help)CS1 maint: numeric names: authors list (link) - ^ a b Jin, Ying-Hui; Cai, Lin; Cheng, Zhen-Shun; Cheng, Hong; Deng, Tong; Fan, Yi-Pin; Fang, Cheng; Huang, Di; Huang, Lu-Qi; Huang, Qiao; Han, Yong; Hu, Bo; Hu, Fen; Li, Bing-Hui; Li, Yi-Rong; Liang, Ke; Lin, Li-Kai; Luo, Li-Sha; Ma, Jing; Ma, Lin-Lu; Peng, Zhi-Yong; Pan, Yun-Bao; Pan, Zhen-Yu; Ren, Xue-Qun; Sun, Hui-Min; Wang, Ying; Wang, Yun-Yun; Weng, Hong; Wei, Chao-Jie; Wu, Dong-Fang; Xia, Jian; Xiong, Yong; Xu, Hai-Bo; Yao, Xiao-Mei; Yuan, Yu-Feng; Ye, Tai-Sheng; Zhang, Xiao-Chun; Zhang, Ying-Wen; Zhang, Yin-Gao; Zhang, Hua-Min; Zhao, Yan; Zhao, Ming-Juan; Zi, Hao; Zeng, Xian-Tao; Wang, Yong-Yan; Wang, Xing-Huan (6 February 2020). "A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version)". Military Medical Research. 7 (1): 4. doi:10.1186/s40779-020-0233-6. ISSN 2095-7467. PMC 7003341. PMID 32029004.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b "CT provides best diagnosis for COVID-19". ScienceDaily. 26 February 2020. Retrieved 2 March 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ a b "Advice for public". www.who.int. Archived from the original on 26 January 2020. Retrieved 25 February 2020.
- ^ a b CDC (11 February 2020). "2019 Novel Coronavirus (2019-nCoV)". Centers for Disease Control and Prevention. Archived from the original on 14 February 2020. Retrieved 15 February 2020.
- ^ "Advice for public". www.who.int. Archived from the original on 26 January 2020. Retrieved 15 February 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 15 February 2020. Archived from the original on 26 February 2020. Retrieved 20 February 2020.
- ^ "Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)". www.who.int. Archived from the original on 31 January 2020. Retrieved 11 February 2020.
- ^ Mahtani S, Berger M, O'Grady S, Iati M (6 February 2020). "Hundreds of evacuees to be held on bases in California; Hong Kong and Taiwan restrict travel from mainland China". The Washington Post. Archived from the original on 7 February 2020. Retrieved 11 February 2020.
- ^ "Coronavirus disease 2019 (COVID-19) Situation Report – 47" (PDF). World Health Organization. Archived (PDF) from the original on 8 March 2020. Retrieved 8 March 2020.
- ^ World Health Organization. "Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)" (PDF). pp. 11–12. Retrieved 5 March 2020.
- ^ Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. (February 2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". Lancet. 395 (10223): 507–13. doi:10.1016/S0140-6736(20)30211-7. PMID 32007143.
- ^ Hessen, Margaret Trexler (27 January 2020). "Novel Coronavirus Information Center: Expert guidance and commentary". Elsevier Connect. Archived from the original on 30 January 2020. Retrieved 31 January 2020.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMID 31986264.
- ^ "WHO COVID-19 situation report 29" (PDF). World Health Organization. 19 February 2020. Archived (PDF) from the original on 2 March 2020. Retrieved 26 February 2020.
- ^ "Q&A on coronaviruses (COVID-19): How long is the incubation period for COVID-19?". www.who.int. Archived from the original on 20 January 2020. Retrieved 26 February 2020.
- ^ Guan, Wei-jie; Ni, Zheng-yi; Hu, Yu; Liang, Wen-hua; Ou, Chun-quan; He, Jian-xing; Liu, Lei; Shan, Hong; Lei, Chun-liang; Hui, David S.C.; Du, Bin; Li, Lan-juan; Zeng, Guang; Yuen, Kwok-Yung; Chen, Ru-chong; Tang, Chun-li; Wang, Tao; Chen, Ping-yan; Xiang, Jie; Li, Shi-yue; Wang, Jin-lin; Liang, Zi-jing; Peng, Yi-xiang; Wei, Li; Liu, Yong; Hu, Ya-hua; Peng, Peng; Wang, Jian-ming; Liu, Ji-yang; Chen, Zhong; Li, Gang; Zheng, Zhi-jian; Qiu, Shao-qin; Luo, Jie; Ye, Chang-jiang; Zhu, Shao-yong; Zhong, Nan-shan (28 February 2020). "Clinical Characteristics of Coronavirus Disease 2019 in China". New England Journal of Medicine. Massachusetts Medical Society. doi:10.1056/nejmoa2002032. ISSN 0028-4793. PMID 32109013.
- ^ a b c Bernheim, Adam; Mei, Xueyan; Huang, Mingqian; Yang, Yang; Fayad, Zahi A.; Zhang, Ning; Diao, Kaiyue; Lin, Bin; Zhu, Xiqi; Li, Kunwei; Li, Shaolin; Shan, Hong; Jacobi, Adam; Chung, Michael (20 February 2020). "Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection". Radiology. Radiological Society of North America (RSNA): 200463. doi:10.1148/radiol.2020200463. ISSN 0033-8419. PMID 32077789.
- ^ CDC (11 February 2020). "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. Retrieved 2 March 2020.
- ^ "New Images of Novel Coronavirus SARS-CoV-2 Now Available". NIH: National Institute of Allergy and Infectious Diseases. 13 February 2020. Retrieved 1 March 2020 – via niaid.nih.gov.
- ^ Gorbalenya, Alexander E. (11 February 2020). "Severe acute respiratory syndrome-related coronavirus – The species and its viruses, a statement of the Coronavirus Study Group". bioRxiv: 2020.02.07.937862. doi:10.1101/2020.02.07.937862. Archived from the original on 11 February 2020. Retrieved 11 February 2020.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses". Nature Microbiology. Retrieved 11 March 2020.
- ^ Zhang, Haibo; Penninger, Josef M.; Li, Yimin; Zhong, Nanshan; Slutsky, Arthur S. (3 March 2020). "Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target". Intensive Care Medicine. Springer Science and Business Media LLC. doi:10.1007/s00134-020-05985-9. ISSN 0342-4642. PMID 32125455.
- ^ a b Xu, Hao; Zhong, Liang; Deng, Jiaxin; Peng, Jiakuan; Dan, Hongxia; Zeng, Xin; Li, Taiwen; Chen, Qianming (24 February 2020). "High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa". International Journal of Oral Science. 12 (1). Springer Science and Business Media LLC: 8. doi:10.1038/s41368-020-0074-x. ISSN 1674-2818. PMC 7039956. PMID 32094336.
- ^ Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. (23 January 2020). "Discovery of a novel coronavirus associated with the recent pneumonia outbreak in humans and its potential bat origin". bioRxiv: 2020.01.22.914952. doi:10.1101/2020.01.22.914952. Archived from the original on 24 January 2020. Retrieved 5 February 2020.
- ^ "The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) - China, 2020" (PDF). China CDC Weekly. 2. 20 February 2020. Archived (PDF) from the original on 18 February 2020. Retrieved 19 February 2020 – via unpublished master.
- ^ Heymann, David L; Shindo, Nahoko (22 February 2020). "COVID-19: what is next for public health?". The Lancet. 395 (10224): 542–545. doi:10.1016/S0140-6736(20)30374-3. ISSN 0140-6736. PMID 32061313. Retrieved 2 March 2020.
- ^ CDC (5 February 2020). "CDC Tests for 2019-nCoV". Centers for Disease Control and Prevention. Archived from the original on 14 February 2020. Retrieved 12 February 2020.
- ^ Schirring, Lisa (16 January 2020). "Japan has 1st novel coronavirus case; China reports another death". CIDRAP. Archived from the original on 20 January 2020. Retrieved 16 January 2020.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases: Interim guidance". World Health Organization. Archived from the original on 20 January 2020. Retrieved 28 January 2020.
- ^ "2019 Novel Coronavirus (2019-nCoV) Situation Summary". Centers for Disease Control and Prevention. 30 January 2020. Archived from the original on 26 January 2020. Retrieved 30 January 2020.
- ^ "Real-Time RT-PCR Panel for Detection 2019-nCoV". Centers for Disease Control and Prevention. 29 January 2020. Archived from the original on 30 January 2020. Retrieved 1 February 2020.
- ^ "Curetis Group Company Ares Genetics and BGI Group Collaborate to Offer Next-Generation Sequencing and PCR-based Coronavirus (2019-nCoV) Testing in Europe". GlobeNewswire News Room. 30 January 2020. Archived from the original on 31 January 2020. Retrieved 1 February 2020.
- ^ Brueck, Hilary (30 January 2020). "There's only one way to know if you have the coronavirus, and it involves machines full of spit and mucus". Business Insider. Archived from the original on 1 February 2020. Retrieved 1 February 2020.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases". Archived from the original on 21 February 2020. Retrieved 26 February 2020.
- ^ "Undiagnosed pneumonia – China (HU) (01): wildlife sales, market closed, RFI Archive Number: 20200102.6866757". Pro-MED-mail. International Society for Infectious Diseases. Archived from the original on 22 January 2020. Retrieved 13 January 2020.
- ^ Cohen J, Normile D (January 2020). "New SARS-like virus in China triggers alarm" (PDF). Science. 367 (6475): 234–235. doi:10.1126/science.367.6475.234. PMID 31949058. Archived (PDF) from the original on 11 February 2020. Retrieved 11 February 2020.
- ^ "Severe acute respiratory syndrome coronavirus 2 isolate Wuhan-Hu-1, complete genome". NCBI. Nature. 11 February 2020. Archived from the original on 21 January 2020. Retrieved 25 February 2020.
- ^ "Severe acute respiratory syndrome coronavirus 2 data hub". NCBI. Retrieved 4 March 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Sequences". NCBI. Retrieved 4 March 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Genomic epidemiology of SARS-CoV2". GISAID. Retrieved 5 March 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "China Makes Over 1.7 Million Covid-19 Testing Kits per Day, Official Says". Yicai Global.
- ^ Zhang, Wei; Du, Rong-Hui; Li, Bei; Zheng, Xiao-Shuang; Yang, Xing-Lou; Hu, Ben; Wang, Yan-Yi; Xiao, Geng-Fu; Yan, Bing; Shi, Zheng-Li; Zhou, Peng (1 January 2020). "Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes". Emerging Microbes & Infections. 9 (1): 386–389. doi:10.1080/22221751.2020.1729071. PMID 32065057.
- ^ "Duke-NUS used COVID-19 antibody tests to establish link between church clusters in a world-first". CNA. Retrieved 2 March 2020.
- ^ Bai, Yan; Yao, Lingsheng; Wei, Tao; Tian, Fei; Jin, Dong-Yan; Chen, Lijuan; Wang, Meiyun (21 February 2020). "Presumed Asymptomatic Carrier Transmission of COVID-19". JAMA. doi:10.1001/jama.2020.2565. PMID 32083643. Retrieved 8 March 2020.
- ^ Wiles, Siouxsie (9 March 2020). "The three phases of Covid-19 – and how we can make it manageable". The Spinoff. Retrieved 9 March 2020.
- ^ a b c Anderson, Roy M; Heesterbeek, Hans; Klinkenberg, Don; Hollingsworth, T Déirdre (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". The Lancet. doi:10.1016/S0140-6736(20)30567-5.
A key issue for epidemiologists is helping policy makers decide the main objectives of mitigation—eg, minimising morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on scale and antiviral drug therapies.
- ^ Grenfell, Rob; Drew, Trevor (17 February 2020). "Here's Why It's Taking So Long to Develop a Vaccine for the New Coronavirus". Science Alert. Archived from the original on 28 February 2020. Retrieved 26 February 2020.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Centers for Disease Control (3 February 2020). "Coronavirus Disease 2019 (COVID-19): Prevention & Treatment". Archived from the original on 15 December 2019. Retrieved 10 February 2020.
- ^ a b World Health Organization. "Advice for Public". Archived from the original on 26 January 2020. Retrieved 10 February 2020.
- ^ "When and how to use masks". www.who.int. Retrieved 8 March 2020.
- ^ https://www.cdc.gov/coronavirus/2019-ncov/about/prevention.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fabout%2Fprevention-treatment.html.
{{cite web}}: Missing or empty|title=(help) - ^ Centers for Disease Control and Prevention (11 February 2020). "What to do if you are sick with 2019 Novel Coronavirus (2019-nCoV)". Archived from the original on 14 February 2020. Retrieved 13 February 2020.
- ^ M, Serena Josephine (14 February 2020). "Watch out! Spitting in public places too can spread infections". The Hindu. ISSN 0971-751X. Retrieved 12 March 2020.
- ^ "SEQUENCE FOR PUTTING ON PERSONAL PROTECTIVE EQUIPMENT (PPE)" (PDF). CDC. Retrieved 8 March 2020.
- ^ a b Dale Fisher; David Heymann. "Q&A: The novel coronavirus outbreak causing COVID-19". Nature (journal). Retrieved 11 March 2020.
- ^ Kui L, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. (February 2020). "Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province". Chinese Medical Journal: 1. doi:10.1097/CM9.0000000000000744. PMID 32044814.
- ^ Cheng ZJ, Shan J (February 2020). "2019 Novel coronavirus: where we are and what we know" (PDF). Infection. doi:10.1007/s15010-020-01401-y. PMID 32072569. Archived (PDF) from the original on 19 February 2020. Retrieved 26 February 2020.
- ^ "Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected". www.who.int. Archived from the original on 31 January 2020. Retrieved 13 February 2020.
- ^ a b Vetter, Pauline; Eckerle, Isabella; Kaiser, Laurent (19 February 2020). "Covid-19: a puzzle with many missing pieces". BMJ. 368: m627. doi:10.1136/bmj.m627. ISSN 1756-1833. PMID 32075791. Retrieved 29 February 2020.
- ^ "Novel Coronavirus - COVID-19: What Emergency Clinicians Need to Know". www.ebmedicine.net. Retrieved 9 March 2020.
- ^ Cheung, Jonathan Chun-Hei; Ho, Lap Tin; Cheng, Justin Vincent; Cham, Esther Yin Kwan; Lam, Koon Ngai (2020). "Staff safety during emergency airway management for COVID-19 in Hong Kong". The Lancet Respiratory Medicine. Elsevier BV. doi:10.1016/s2213-2600(20)30084-9. ISSN 2213-2600. PMID 32105633.
- ^ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Retrieved 8 March 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Retrieved 11 March 2020.
- ^ "China launches coronavirus 'close contact' app". BBC News. 11 February 2020. Retrieved 7 March 2020.
- ^ Chen, Angela. "China's coronavirus app could have unintended consequences". MIT Technology Review. Retrieved 7 March 2020.
- ^ Nebehay, Stephanie; Kelland, Kate; Liu, Roxanne (5 February 2020). "WHO: 'no known effective' treatments for new coronavirus". Thomson Reuters. Archived from the original on 5 February 2020. Retrieved 5 February 2020.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Ko, WC; Rolain, JM; Lee, NY; Chen, PL; Huang, CT; Lee, PI; Hsueh, PR (5 March 2020). "Arguments in favor of remdesivir for treating SARS-CoV-2 infections". International journal of antimicrobial agents: 105933. doi:10.1016/j.ijantimicag.2020.105933. PMID 32147516.
- ^ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Retrieved 11 March 2020.
- ^ a b Gao J, Tian Z, Yang X (February 2020). "Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies". Bioscience Trends. doi:10.5582/bst.2020.01047. PMID 32074550.
- ^ a b Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. (February 2020). "Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro". Cell Research. 30 (3): 269–271. doi:10.1038/s41422-020-0282-0. PMC 7054408. PMID 32020029.
- ^ Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH (March 2020). "Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed". The Lancet. Psychiatry. 7 (3): 228–229. doi:10.1016/S2215-0366(20)30046-8. PMID 32032543.
- ^ Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. (March 2020). "The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus". The Lancet. Psychiatry. 7 (3): e14. doi:10.1016/S2215-0366(20)30047-X. PMID 32035030.
- ^ The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020. China CDC Weekly, 2020, 2(8): 113–122.
- ^ "WHO Director-General's statement on the advice of the IHR Emergency Committee on Novel Coronavirus". who.int.
- ^ Wang W, Tang J, Wei F (April 2020). "Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China". Journal of Medical Virology. 92 (4): 441–447. doi:10.1002/jmv.25689. PMID 31994742.
- ^ Ji, Yunpeng; Ma, Zhongren; Peppelenbosch, Maikel P; Pan, Qiuwei (25 February 2020). "Potential association between COVID-19 mortality and health-care resource availability". The Lancet Global Health. 0. doi:10.1016/S2214-109X(20)30068-1. ISSN 2214-109X. PMID 32109372. Retrieved 8 March 2020.
- ^ Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). World Health Organization (WHO), 16–24 February 2020
- ^ "Limited data on coronavirus may be skewing assumptions about severity". STAT. 30 January 2020. Archived from the original on 1 February 2020. Retrieved 1 February 2020.
- ^ Sparrow, Annie. "How China's Coronavirus Is Spreading—and How to Stop It". Foreign Policy. Archived from the original on 31 January 2020. Retrieved 2 February 2020.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "WHOが"致死率3%程度" 専門家「今後 注意が必要」". NHK. 24 January 2020. Archived from the original on 26 January 2020. Retrieved 3 February 2020.
- ^ Boseley, Sarah (17 February 2020). "Coronavirus causes mild disease in four in five patients, says WHO". The Guardian. Archived from the original on 18 February 2020. Retrieved 18 February 2020.
- ^ Diao, Ying; Liu, Xiaoyun; Wang, Tao; Zeng, Xiaofei; Dong, Chen; Zhou, Changlong; Zhang, Yuanming; She, Xuan; Liu, Dingfu; Hu, Zhongli (20 February 2020). "Estimating the cure rate and case fatality rate of the ongoing epidemic COVID-19". doi:10.1101/2020.02.18.20024513.
{{cite journal}}: Cite journal requires|journal=(help) - ^ "2019-nCoV: preliminary estimates of the confirmed-case-fatality-ratio and infection-fatality-ratio, and initial pandemic risk assessment". institutefordiseasemodeling.github.io. Retrieved 1 March 2020.
- ^ "Report 4: Severity of 2019-novel coronavirus (nCoV)" (PDF). Archived (PDF) from the original on 10 February 2020. Retrieved 10 February 2020.
- ^ Chen, Huijun; Guo, Juanjuan; Wang, Chen; Luo, Fan; Yu, Xuechen; Zhang, Wei; Li, Jiafu; Zhao, Dongchi; Xu, Dan; Gong, Qing; Liao, Jing; Yang, Huixia; Hou, Wei; Zhang, Yuanzhen (12 February 2020). "Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records". The Lancet. 395 (10226): 809–815. doi:10.1016/S0140-6736(20)30360-3. ISSN 0140-6736.
- ^ Cui, Pengfei; Chen, Zhe; Wang, Tian; Dai, Jun; Zhang, Jinjin; Ding, Ting; Jiang, Jingjing; Liu, Jia; Zhang, Cong; Shan, Wanying; Wang, Sheng; Rong, Yueguang; Chang, Jiang; Miao, Xiaoping; Ma, Xiangyi; Wang, Shixuan (27 February 2020), Clinical features and sexual transmission potential of SARS-CoV-2 infected female patients: a descriptive study in Wuhan, China, Cold Spring Harbor Laboratory, doi:10.1101/2020.02.26.20028225
- ^ Cascella, Marco; Rajnik, Michael; Cuomo, Arturo; Dulebohn, Scott C.; Di Napoli, Raffaela (8 March 2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". Retrieved 11 March 2020.
- ^ Chen, Wen-Hsiang; Strych, Ulrich; Hotez, Peter J; Bottazzi, Maria Elena (3 March 2020). "The SARS-CoV-2 Vaccine Pipeline: an Overview". Current Tropical Medicine Reports. Springer Science and Business Media LLC. doi:10.1007/s40475-020-00201-6. ISSN 2196-3045.
- ^ a b Li, Guangdi; De Clercq, Erik (2020). "Therapeutic options for the 2019 novel coronavirus (2019-nCoV)". Nature Reviews Drug Discovery. 19 (3): 149–150. doi:10.1038/d41573-020-00016-0. PMID 32127666.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Beeching, Nicholas J.; Fletcher, Tom E.; Fowler, Robert (2020). "COVID-19" (PDF). BMJ Best Practices. BMJ.
{{cite web}}: CS1 maint: url-status (link) - ^ "Physicians work out treatment guidelines for coronavirus". m.koreabiomed.com (in Korean). 13 February 2020.
- ^ "Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (Provisional 7th Edition)". China Law Translate. 4 March 2020.
- ^ Steenhuysen, Julie; Kelland, Kate (24 January 2020). "With Wuhan virus genetic code in hand, scientists begin work on a vaccine". Reuters. Archived from the original on 25 January 2020. Retrieved 25 January 2020.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Praveen Duddu. Coronavirus outbreak: Vaccines/drugs in the pipeline for Covid-19 Archived 19 February 2020 at the Wayback Machine. clinicaltrialsarena.com 19 February 2020.
- ^ Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV). Biosci Trends. 28 January 2020. doi:10.5582/bst.2020.01020
- ^ a b Hoffmann, Markus; Kleine-Weber, Hannah; Krüger, Nadine; Müller, Marcel; Drosten, Christian; Pöhlmann, Stefan (31 January 2020). "The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells". bioRxiv: 2020.01.31.929042. doi:10.1101/2020.01.31.929042.
- ^ Iwata-Yoshikawa, Naoko; Okamura, Tadashi; Shimizu, Yukiko; Hasegawa, Hideki; Takeda, Makoto; Nagata, Noriyo (15 March 2019). "TMPRSS2 Contributes to Virus Spread and Immunopathology in the Airways of Murine Models after Coronavirus Infection". Journal of Virology. 93 (6). doi:10.1128/JVI.01815-18. ISSN 0022-538X. PMC 6401451. PMID 30626688.
- ^ Enserink, Martin (12 February 2020). "Update: 'A bit chaotic.' Christening of new coronavirus and its disease name create confusion". American Association for the Advancement of Science. Science Magazine. Archived from the original on 20 February 2020. Retrieved 27 February 2020.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Novel coronavirus named 'Covid-19': WHO". TODAYonline. Retrieved 11 February 2020.
- ^ "The coronavirus spreads racism against—and among—ethnic Chinese". The Economist. 17 February 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
External links
- Centers for Disease Control (CDC): Coronavirus Disease 2019 (COVID-19)
- World Health Organization (WHO): Coronavirus disease (COVID-19) outbreak
- Steps to Prevent COV19 for the general population, by the US Centers for Disease Control and Prevention
- Preventing COVID-19 Spread in Communities, by the US Centers for Disease Control and Prevention
- Information for Healthcare Professionals, by the US Centers for Disease Control and Prevention
- "SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Sequences". National Center for Biotechnology Information (NCBI).
- "Coronavirus: Latest news and resources". BMJ.
- "Novel Coronavirus Information Center". Elsevier.
- "COVID-19 Resource Centre". Lancet.
- "SARS-CoV-2 and COVID-19". Nature.
- "Coronavirus (Covid-19)". NEJM.
- "Covid-19: Novel Coronavirus Content Free to Access". Wiley.
- "Coronavirus Disease 2019 (COVID-19)". JAMA Network.


