Oncology
This article needs additional citations for verification. (July 2022) |
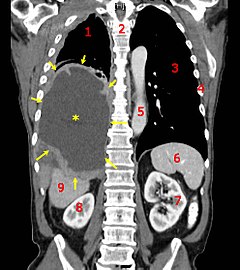 A coronal CT scan showing a malignant mesothelioma, indicated by the asterisk and the arrows | |
| Focus | Cancerous tumor |
|---|---|
| Subdivisions | Medical oncology, radiation oncology, surgical oncology |
| Significant tests | Tumor markers, TNM staging, CT scans, MRI |
| Occupation | |
|---|---|
Occupation type | Specialty |
Activity sectors | Medicine |
| Description | |
Education required |
|
Fields of employment | Hospitals, Clinics, Clinical research centers |
Oncology is a branch of medicine that deals with the study, treatment, diagnosis and prevention of cancer. A medical professional who practices oncology is an oncologist.[1] The name's etymological origin is the Greek word ὄγκος (ónkos), meaning "tumor", "volume" or "mass".[2] Oncology is concerned with:
- The diagnosis of any cancer in a person (pathology)
- Therapy (e.g. surgery, chemotherapy, radiotherapy and other modalities)
- Follow-up of cancer patients after successful treatment
- Palliative care of patients with terminal malignancies
- Ethical questions surrounding cancer care
- Screening efforts:
- of populations, or
- of the relatives of patients (in types of cancer that are thought to have a hereditary basis, such as breast cancer)
Diagnosis
Medical histories remain an important screening tool: the character of the complaints and nonspecific symptoms (such as fatigue, weight loss,[3] unexplained anemia,[4] fever of unknown origin, paraneoplastic phenomena and other signs) may warrant further investigation for malignancy. Occasionally, a physical examination may find the location of a malignancy.
Diagnostic methods include:
- Biopsy or resection; these are methods by which suspicious neoplastic growths can be removed in part or in whole, and evaluated by a pathologist to determine malignancy. This is currently the gold standard for the diagnosis of cancer and is crucial in guiding the next step in management (active surveillance, surgery, radiation therapy, chemotherapy or a combination of these)[5]
- Endoscopy, either upper or lower gastrointestinal, cystoscopy, bronchoscopy, or nasendoscopy; to localise areas suspicious for malignancy and biopsy when necessary.[6]
- X-rays, CT scanning, MRI scanning, ultrasound and other radiological techniques to localise and guide biopsy.
- Scintigraphy, single photon emission computed tomography (SPECT), positron emission tomography (PET) and other methods of nuclear medicine to identify areas suspicious for malignancy.
- Blood tests, including tumor markers, which can increase the suspicion of certain types of cancers.
Apart from diagnoses, these modalities (especially imaging by CT scanning) are often used to determine operability, i.e. whether it is surgically possible to remove a tumor in its entirety.
Currently, a tissue diagnosis (from a biopsy) by a pathologist is essential for the proper classification of cancer and to guide the next step of treatment. On extremely rare instances when this is not possible, "empirical therapy" (without an exact diagnosis) may be considered, based on the available evidence (e.g. history, x-rays and scans.)
On very rare occasions, a metastatic lump or pathological lymph node is found (typically in the neck) for which a primary tumor cannot be found. However, immunohistochemical markers often give a strong indication of the primary malignancy. This situation is referred to as "malignacy of unknown primary", and again, treatment is empirical based on past experience of the most likely origin.[7]
Therapy
Depending upon the cancer identified, followup and palliative care will be administered at that time. Certain disorders (such as ALL or AML) will require immediate admission and chemotherapy, while others will be followed up with regular physical examination and blood tests.
Often, surgery is attempted to remove a tumor entirely. This is only feasible when there is some degree of certainty that the tumor can in fact be removed. When it is certain that parts will remain, curative surgery is often impossible, e.g. when there are metastases, Occasionally, when the tumor has invaded a structure that cannot be operated upon without risking the patient's life. Occasionally surgery can improve survival even if not all tumour tissue has been removed; the procedure is referred to as "debulking" (i.e. reducing the overall amount of tumour tissue). Surgery is also used for the palliative treatment of some of cancers, e.g. to relieve biliary obstruction, or to relieve the problems associated with some cerebral tumors. The risks of surgery must be weighed against the benefits.
Chemotherapy and radiotherapy are used as a first-line radical therapy in a number of malignancies. They are also used for adjuvant therapy, i.e. when the macroscopic tumor has already been completely removed surgically but there is a reasonable statistical risk that it will recur. Chemotherapy and radiotherapy are commonly used for palliation, where disease is clearly incurable: in this situation the aim is to improve the quality of life and to prolong it.
Hormone manipulation is well established, particularly in the treatment of breast and prostate cancer.
There is currently a rapid expansion in the use of monoclonal antibody treatments, notably for lymphoma (Rituximab) and breast cancer (Trastuzumab).
Vaccine and other immunotherapies are the subject of intensive research.
Palliative care
Approximately 50% of all cancer cases in the Western world can be treated to remission with radical treatment. For pediatric patients, that number is much higher. A large number of cancer patients will die from the disease, and a significant proportion of patients with incurable cancer will die of other causes. There may be ongoing issues with symptom control associated with progressive cancer, and also with the treatment of the disease. These problems may include pain, nausea, anorexia, fatigue, immobility, and depression. Not all issues are strictly physical: personal dignity may be affected. Moral and spiritual issues are also important.
While many of these problems fall within the remit of the oncologist, palliative care has matured into a separate, closely allied speciality to address the problems associated with advanced disease. Palliative care is an essential part of the multidisciplinary cancer care team. Palliative care services may be less hospital-based than oncology, with nurses and doctors who are able to visit the patient at home.
Ethical issues
There are a number of recurring ethical questions and dilemmas in oncological practice. These include:
- What information to give the patient regarding disease extent/progression/prognosis.
- Entry into clinical trials, especially in the face of terminal illness.
- Withdrawal of active treatment.
- "Do Not Resuscitate" orders and other end of life issues.
These issues are closely related to the patients' personality, religion, culture, and family life. Though these issues are complex and emotional, the answers are often achieved by the patient seeking counsel from trusted personal friends and advisors. It requires a degree of sensitivity and very good communication on the part of the oncology team to address these problems properly.
Progress and research
There is a tremendous amount of research being conducted on all frontiers of oncology, ranging from cancer cell biology, radiation therapy to chemotherapy treatment regimens and optimal palliative care and pain relief. In the past decade, the advent of next-generation sequencing and whole-genome sequencing has completely changed our understanding of cancers. Identification of novel genetic/molecular markers will dramatically change how we diagnose and treat cancer, which will pave the way for personalized medicine.
Therapeutic trials often involve patients from many different hospitals in a particular region. In the UK, patients are often enrolled in large studies coordinated by Cancer Research UK (CRUK),[8] Medical Research Council (MRC),[9] the European Organisation for Research and Treatment of Cancer (EORTC)[10] or the National Cancer Research Network (NCRN).
The most valued companies worldwide whose leading products are in Oncology include Pfizer (United States), Roche (Switzerland), Merck (United States), AstraZeneca (United Kingdom), Novartis (Switzerland) and Bristol-Myers Squibb (United States) who are active in the treatment areas Kinase inhibitors, Antibodies, Immuno-oncology and Radiopharmaceuticals.[11]
Specialties
- The four main divisions:
- Medical oncology: focuses on treatment of cancer with chemotherapy, targeted therapy, immunotherapy, and hormonal therapy.[12]
- Surgical oncology: focuses on treatment of cancer with surgery.[13]
- Radiation oncology: focuses on treatment of cancer with radiation.[13]
- Clinical oncology: focuses on treatment of cancer with both systemic therapies and radiation.[14]
- Sub-specialties in Oncology:
- Neuro-oncology: focuses on cancers of brain.
- Ocular oncology: focuses on cancers of eye.[15]
- Head & Neck oncology: focuses on cancers of oral cavity, nasal cavity, oropharynx, hypopharynx and larynx.[16]
- Thoracic oncology: focuses on cancers of lung, mediastinum, oesophagus and pleura.[17]
- Breast oncology: focuses on cancers of breast.
- Gastrointestinal oncology: focuses on cancers of stomach, colon, rectum, anal canal, liver, gallbladder, pancreas.[18]
- Bone & Musculoskeletal oncology: focuses on cancers of bones and soft tissue.[19]
- Dermatological oncology: focuses on the medical and surgical treatment of skin, hair, sweat gland, and nail cancers
- Genitourinary oncology: focuses on cancers of genital and urinary system.[20]
- Gynecologic oncology: focuses on cancers of the female reproductive system.[21]
- Pediatric oncology: concerned with the treatment of cancer in children.[22]
- Adolescent and young adult (AYA) oncology.[23]
- Hemato oncology: focuses on cancers of blood and stem cell transplantation.
- Preventive oncology: focuses on epidemiology & prevention of cancer.[24]
- Geriatric oncology: focuses on cancers in elderly population.[25]
- Pain & Palliative oncology: focuses on treatment of end stage cancer to help alleviate pain and suffering.[26]
- Molecular oncology: focuses on molecular diagnostic methods in oncology.[27]
- Nuclear medicine oncology: focuses on diagnosis and treatment of cancer with radiopharmaceuticals.
- Psycho-oncology: focuses on psychosocial issues on diagnosis and treatment of cancer patients.
- Veterinary oncology: focuses on treatment of cancer in animals.[28]
- Emerging specialties:
- Cardiooncology is a branch of cardiology that addresses the cardiovascular impact of cancer and its treatments.[29]
See also
- Organizations
References
- ^ Maureen McCutcheon. Where Have My Eyebrows Gone?. Cengage Learning, 2001. ISBN 0766839346. Page 5.
- ^ Types of Oncologists Archived 2017-07-26 at the Wayback Machine, American Society of Clinical Oncology (ASCO).
- ^ Alfred E. Chang & authors. Oncology: An Evidence-Based Approach. Springer Science & Business Media, 2007. ISBN 0387310568. Page 1488.
- ^ Alice Villalobos, Laurie Kaplan. Canine and Feline Geriatric Oncology: Honoring the Human-Animal Bond. John Wiley & Sons, 2008. ISBN 0470344075. Page 77.
- ^ "How biopsy procedures are used to diagnose cancer". Mayo Clinic. Archived from the original on 2023-06-13. Retrieved 2023-06-13.
- ^ "Endoscopy". British Medical Association Complete Family Health Encyclopedia. Dorling Kindersley Limited. 1990.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 104: Metastatic malignant disease of unknown primary origin: Diagnosis and management of metastatic malignant disease of unknown primary origin. London, 2010.
- ^ "Cancer Research UK". Cancer Research UK. 10 May 2021. Archived from the original on 2022-12-30. Retrieved 2022-12-30.
- ^ "Home - Medical Research Council". Archived from the original on 2017-09-12. Retrieved 2004-03-29.
- ^ "European Organisation For Research And Treatment Of Cancer". EORTC. January 17, 2017. Archived from the original on October 28, 2022. Retrieved March 2, 2020.
- ^ "Top Global Pharmaceutical Company Report" (PDF). The Pharma 1000. November 2021. Archived (PDF) from the original on 2022-03-15. Retrieved 29 December 2022.
- ^ Kennedy, B. J. (1997-12-01). "Medical oncology as a discipline". Oncology. 54 (6): 459–462. doi:10.1159/000227603. ISSN 0030-2414. PMID 9394841.
- ^ a b "Types of Oncologists". Cancer.Net : American Society of Clinical Oncology (ASCO). 2011-05-09. Archived from the original on 2013-06-01. Retrieved 25 May 2013.
- ^ "What is clinical oncology? | the Royal College of Radiologists". Archived from the original on 2021-08-11. Retrieved 2021-08-11.
- ^ Natarajan, Sundaram (2015-02-01). "Ocular oncology – A multidisciplinary specialty". Indian Journal of Ophthalmology. 63 (2): 91. doi:10.4103/0301-4738.154364. ISSN 0301-4738. PMC 4399140. PMID 25827536.
- ^ Manganaris, Argyris; Black, Myles; Balfour, Alistair; Hartley, Christopher; Jeannon, Jean-Pierre; Simo, Ricard (2009-07-01). "Sub-specialty training in head and neck surgical oncology in the European Union". European Archives of Oto-Rhino-Laryngology. 266 (7): 1005–1010. doi:10.1007/s00405-008-0832-4. ISSN 1434-4726. PMID 19015865. S2CID 20700214.
- ^ Harish, Krishnamachar; Kirthi Koushik, Agrahara Sreenivasa (2015-05-01). "Multidisciplinary teams in thoracic oncology-from tragic to strategic". Annals of Translational Medicine. 3 (7): 89. doi:10.3978/j.issn.2305-5839.2015.01.31. ISSN 2305-5839. PMC 4430737. PMID 26015931.
- ^ Mulder, Chris Jacob Johan; Peeters, Marc; Cats, Annemieke; Dahele, Anna; Droste, Jochim Terhaar sive (2011-03-07). "Digestive oncologist in the gastroenterology training curriculum". World Journal of Gastroenterology. 17 (9): 1109–1115. doi:10.3748/wjg.v17.i9.1109. ISSN 1007-9327. PMC 3063902. PMID 21556128.
- ^ Weber, Kristy L.; Gebhardt, Mark C. (2003-04-01). "What's new in musculoskeletal oncology". The Journal of Bone and Joint Surgery. American Volume. 85-A (4): 761–767. doi:10.2106/00004623-200304000-00029. ISSN 0021-9355. PMID 12672857.
- ^ Bukowski, Ronald M. (2011-10-10). "Genitourinary Oncology: Current Status and Future Challenges". Frontiers in Oncology. 1: 32. doi:10.3389/fonc.2011.00032. ISSN 2234-943X. PMC 3355990. PMID 22649760.
- ^ Benedetti-Panici, P.; Angioli, R. (2004-01-01). "Gynecologic oncology specialty". European Journal of Gynaecological Oncology. 25 (1): 25–26. ISSN 0392-2936. PMID 15053057.
- ^ Wolff, J. A. (1991-06-01). "History of pediatric oncology". Pediatric Hematology and Oncology. 8 (2): 89–91. doi:10.3109/08880019109033436. ISSN 0888-0018. PMID 1863546.
- ^ Shaw, Peter H.; Reed, Damon R.; Yeager, Nicholas; Zebrack, Bradley; Castellino, Sharon M.; Bleyer, Archie (April 2015). "Adolescent and Young Adult (AYA) Oncology in the United States: A Specialty in Its Late Adolescence". Journal of Pediatric Hematology/Oncology. 37 (3): 161–169. doi:10.1097/MPH.0000000000000318. ISSN 1536-3678. PMID 25757020. S2CID 27695404.
- ^ Mkrtchyan, L. N. (2010-06-01). "On a new strategy of preventive oncology". Neurochemical Research. 35 (6): 868–874. doi:10.1007/s11064-009-0110-x. ISSN 1573-6903. PMID 20119639. S2CID 582313.
- ^ Vijaykumar, D. K.; Anupama, R.; Gorasia, Tejal Kishor; Beegum, T. R. Haleema; Gangadharan, P. (2012-01-01). "Geriatric oncology: The need for a separate subspecialty". Indian Journal of Medical and Paediatric Oncology. 33 (2): 134–136. doi:10.4103/0971-5851.99755. ISSN 0971-5851. PMC 3439792. PMID 22988358.
- ^ Epstein, A. S.; Morrison, R. S. (2012-04-01). "Palliative oncology: identity, progress, and the path ahead". Annals of Oncology. 23 (Suppl 3): 43–48. doi:10.1093/annonc/mds087. ISSN 1569-8041. PMC 3493143. PMID 22628415.
- ^ Jenkins, Robert (2001-04-01). "Principles of Molecular Oncology". American Journal of Human Genetics. 68 (4): 1068. doi:10.1086/319526. ISSN 0002-9297. PMC 1275628.
- ^ Breen, Matthew (2009-08-01). "Update on genomics in veterinary oncology". Topics in Companion Animal Medicine. 24 (3): 113–121. doi:10.1053/j.tcam.2009.03.002. ISSN 1938-9736. PMC 2754151. PMID 19732729.
- ^ Ghosh, AK; Walker, JM (2 January 2017). "Cardio-oncology". British Journal of Hospital Medicine. 78 (1): C11–C13. doi:10.12968/hmed.2017.78.1.C11. PMID 28067553.
Further reading
- Watson, Ian R.; Takahashi, Koichi; Futreal, P. Andrew; Chin, Lynda (2013). "Emerging patterns of somatic mutations in cancer". Nat Rev Genet. 14 (10): 703–718. doi:10.1038/nrg3539. PMC 4014352. PMID 24022702.
- Meyerson, Matthew; Gabriel, Stacey; Getz, Gad (2010). "Advances in understanding cancer genomes through second-generation sequencing". Nat Rev Genet. 11 (10): 685–696. doi:10.1038/nrg2841. PMID 20847746. S2CID 2544266.
- Katsanis, Sara Huston; Katsanis, Nicholas (2013). "Molecular genetic testing and the future of clinical genomics". Nat Rev Genet. 14 (6): 415–426. doi:10.1038/nrg3493. PMC 4461364. PMID 23681062.
- Mardis, Elaine R. (2012). "Applying next-generation sequencing to pancreatic cancer treatment". Nat Rev Gastroenterol Hepatol. 9 (8): 477–486. doi:10.1038/nrgastro.2012.126. PMID 22751458. S2CID 9981262.
- Mukherjee, Siddhartha (2011). The Emperor of All Maladies: A Biography of Cancer. Fourth Estate. ISBN 978-0-00-725092-9.
- Vickers, Andrew (1 March 2004). "Alternative Cancer Cures: "Unproven" or "Disproven"?". CA: A Cancer Journal for Clinicians. 54 (2): 110–118. CiteSeerX 10.1.1.521.2180. doi:10.3322/canjclin.54.2.110. PMID 15061600. S2CID 35124492.
External links
- "Comprehensive Cancer Information". National Cancer Institute. January 1980. Retrieved 2016-01-16.
- "NCCN - Evidence-Based Cancer Guidelines, Oncology Drug Compendium, Oncology Continuing Medical Education". National Comprehensive Cancer Network. Retrieved 2016-01-16.
- "European Society for Medical Oncology | ESMO". www.esmo.org. Retrieved 2016-01-16.
