Dipalmitoylphosphatidylcholine
| |
| Identifiers | |
|---|---|
3D model (JSmol)
|
|
| ChemSpider | |
| ECHA InfoCard | 100.018.322 |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C40H80NO8P | |
| Molar mass | 734.053 g·mol−1 |
| Surface tension: | |
| 4.6 ± 0.5 x 10−10 M[1] | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
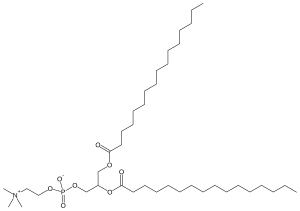
Dipalmitoylphosphatidylcholine (DPPC) is a phospholipid (and a lecithin) consisting of two palmitic acids attached to a phosphatidylcholine head-group.
It is the main constituent of pulmonary surfactants, which reduces the work of breathing and prevents alveolar collapse during breathing. It also plays an important role in the study of liposomes and human bilayers.
Lung surfactant
Lung surfactant (LS) is a surface active material produced by most air-breathing animals with the aim of reducing the surface tension of water when gas exchange occurs, given that the inhalation and exhalation movements may cause damage if there is not enough energy to sustain it.
The monolayer formed by the LS on the interface is composed mainly by phospholipids (80%), proteins (12%) and neutral lipids (8%). Among these phospholipids, the prevailing is phosphatidylcholine (PC, or lecithin) (70–85%), which composes a pool where 50% of the material is DPPC.[2]
DPPC already has the capacity to minimize the tension, but it requires the presence of proteins and other lipids from the surfactant to ease the adsorption in the air-liquid interphase.[3]
That DPPC is a variant of lecithin and its structure is based on a hydrophilic head and hydrophobic tails grants it such properties. The polar and hydrophilic head is caused by the choline radical, oriented towards the alveolar liquid, and the non-polar and hydrophobic tails are due to the palmitic acid chains, oriented towards the outer side.
Biosynthesis
The synthesis of phospholipids from pulmonary surfactant takes place in the endoplasmic reticulum of type II pneumocytes. Pulmonary surfactant has a protein and a lipid composition. Specifically, it has been found that phosphatidylcholine is the most abundant phospholipid (70%–85%) and it mostly disaturates in the form of dipalmitoylphosphatidylcholine (DPPC).
The novo synthesis of phosphatidylcholine in the lung occurs mainly from the formation of CDP-choline. The passage from CDP-choline to phosphatidylcholine is catalyzed by Choline-phosphate cytidyltransferase. Although the main enzyme acting on its synthesis is Choline-phosphate cytidyltransferase, there are certain conditions under which the enzymes choline kinase, glycerol-3-phosphate acyltransferase and phosphatidate phosphatase may play a regulatory role.
From the novo biosynthesis, we obtain 45% of the total DPPC of the pulmonary surfactant. The rest is formed by disacylation and reacylation mechanisms from unsaturated acyl chains of phosphatidylcholine.[4] The elimination of the acyl chain occurs by transacylation, thus obtaining a lysophospholipid. After the disacylation or transacylation process, lysophosphatidylcholine is obtained, resulting in DPPC after reacillating it with palinitoilCoa by means of aciltransferated lysophosphatidylcholine.
Characteristics

Temperature
This phospholipid is found in a solid/gel phase at 37 °C (at the effective temperature of the human body). Its melting point is around 41.3 °C. Therefore, when the temperature is above 41 °C, DPPC is no longer found in a gel phase but in a liquid one.[5]
It has been demonstrated that DPPC bilayers have different properties depending on the temperature when studied in contact with silica surfaces.
Layer thickness remains the same at 25 °C and at 39 °C. However, when the temperature is further increased to 55 °C, the DPPC bilayer structure changes significantly, which causes a decrease in the layer thickness. The reason of this trait is that, in fact, at 55 °C DPPC is found in a liquid disordered state, whereas at a lower temperature it is found in a gel state.
Temperature affects the layer´s roughness too, which starts to change slightly when temperature is lowered to 25 °C.
Finally, the load bearing capacity of this bilayer is higher when the temperature exceeds the phase transition temperature (due to its increased fluidity). When this molecule is found in a liquid state, where the fluidity is much higher, it is thought that the bilayer develops a self-healing capacity.[6]
Amphipathic behaviour

DPPC is an amphipathic lipid. This characteristic is due to its hydrophilic head, composed by the phosphatidylcholine group, and its hydrophobic tail, formed by two palmitic acids. This trait allows DPPC to easily form micelles, monolayers, bilayers and liposomes spontaneously in contact with a polar solvent.
Surfactant
DPPC is the main phospholipid of pulmonary surfactant, and it is surface-active due to its amphipathic behaviour and its adsorption capacity.[7] However, DPPC adsorption is not quite effective at human body temperature, because at 37 °C it is found in a gel phase. So, the presence of some unsaturated phospholipids (such as dioleoylphosphatidylcholine or phosphatidylglycerol) and cholesterol is required in the surfactant to increase its fluidity, so it adsorbs more efficiently.[8] Therefore, when this mixture contacts water, for example, it accumulates in the interphase water and air, causing a significant diminution of water surface-tension. A thin, superficial pellicule of surfactant is created in the interphase. The molecules composing the surfactant (DPPC) feel attracted by the liquid molecules (in this case, H20 molecules) which causes the diminution of surface-tension.
Current uses
Research uses
DPPC is usually used for research purposes, such as creating liposomes and bilayers which are involved in bigger studies. The Langmuir–Blodgett technique allows the synthesis of liposomal DPPC bilayers. Currently, this liposomes are used in the study of the properties of this phosphatidilcoline and the mechanism of drug delivery in the human body.
Furthermore, that vesicle fusion dynamics are different for lipids in the gel phase versus the fluid phase, allows scientists to use DPPC along with DOPC in Atomic Force Microscopy and Atomic Force Spectroscopy.[9][10]
Pharmaceutical uses
DPPc is routinely used in formulation of some medicines commonly used for RDS treatment in newborns. Current synthetic surfactants are combinations of DPPC along with other phospholipids,[11] neutral lipids] and lipoproteins.
The treatment of respiratory distress syndrome with surfactants for preterm infants was developed in the 1960s and recent studies have demonstrated an improvement in clinical outcomes.[12] The first treatment administered to some newborns with RDS was with surfactant phospholipids, specifically with dipalmitoylphosphatidylcholine by means of an aerosol (Robillard, 1964).[full citation needed] This treatment proved to be ineffective, as the administration of DPPC alone did not achieve any beneficial effects. Subsequently, various studies were carried out to obtain more efficient drugs for the treatment of this disease.
Pulmonary surfactants can be classified into three types:[13]
Firstly, we have the first generation of protein-free synthetic surfactants. This first generation contains only DPPC. The best known is colfosceril palmitate.[13]
Secondly, we have the second generation of natural surfactants of animal origin. These were obtained from cattle or pigs' lungs. The surfactants extracted from bovines were Infasurf and Alvofact, those from porcine extracts were Curosurf and from modified bovine extracts were Survanta (Beractant). Unlike the ones from the first generation, newborns with RDS had less oxygen requirement and ventilatory support within 72 hours of drug administration.
Thirdly, we have the third generation of synthetic peptides or recombinant proteins. These use a mixture of different components. DPPC is used as an agent to decrease surface tension and the rest of the aggregates increase adsorption. The best known are Venicute and Surfaxin[13]. They are still under development so there is no evidence about its advantages over the second generation.
It is also used for liposome formation for drug delivery.[14]
DPPC related illnesses
Surfactant Dysfunction Disorder is a disease that affects newborn children whose pulmonary surfactant is insufficient for adequate breathing causing respiratory distress syndrome.[15]
Despite DPPC being one of the major components of lung surfactant, most of the genetic errors that are linked with surfactant dysfunction disorder are not linked to DPPC. The main causes of this disease are differences in the production of surfactant proteins B and C due to genetic conditions.
However, there is a genetic condition that is related to DPPC which causes a deficiency in the production of ABCA1 protein which is crucial in the transportation of phospholipids and, therefore, DPPC to the lamellar bodies of the alveolar cells where DPPC interacts with surfactant proteins to form surfactant.[16]
Current studies cannot find a correlation between the percentage of DPPC in lung surfactant with the age of gestation, although there is a proven relationship between the percentage of DPPC and POPC in babies with respiratory distress syndrome compared with babies without this condition. These connections suggest that a particular surfactant composition will lead to respiratory distress syndrome, irrespective of gestational age.
The correlation between DPPC percentage and respiratory distress syndrome is why DPPC is used to make drugs to treat newborn infants with the disease.[17]
In addition, DPPC has been demonstrated to be related to infection of polarized cells by a specific kind of human adenovirus (HAdV-C2). Some studies have shown that disaturated DPPC apparently boosts infection of A59 cells with HAdV-C2 (possibly permitting the virus entry by the apical side of polarized cells).[18]
References
- ^ Smith, Ross; Tanford, Charles (June 1972). "The critical micelle concentration of l-α-dipalmitoylphosphatidylcholine in water and water/methanol solutions". Journal of Molecular Biology. 67 (1): 75–83. doi:10.1016/0022-2836(72)90387-7. PMID 5042465.
- ^ Stachowicz-Kuśnierz, Anna; Seidler, Tomasz; Rogalska, Ewa; Korchowiec, Jacek; Korchowiec, Beata (2020-02-01). "Lung surfactant monolayer – A good natural barrier against dibenzo-p-dioxins". Chemosphere. 240: 124850. doi:10.1016/j.chemosphere.2019.124850. ISSN 0045-6535. PMID 31561163.
- ^ "Dipalmitoylphosphatidylcholine - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2019-10-24.
- ^ Fernández Ruano, D. Miguel Luis (2000). Caracterización del complejo surfactante pulmonar: Estudio de la estructura y función de la proteína A (SP-A) (PDF). Madrid: Universidad Complutense de Madrid. pp. 10–11.
- ^ "Dipalmitoylphosphatidylcholine - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2019-10-25.
- ^ Wang, Min; Zander, Thomas; Liu, Xiaoyan; Liu, Chao; Raj, Akanksha; Florian Wieland, D. C.; Garamus, Vasil M.; Willumeit-Römer, Regine; Claesson, Per Martin; Dėdinaitė, Andra (2015-05-01). "The effect of temperature on supported dipalmitoylphosphatidylcholine (DPPC) bilayers: Structure and lubrication performance". Journal of Colloid and Interface Science. 445: 84–92. Bibcode:2015JCIS..445...84W. doi:10.1016/j.jcis.2014.12.042. ISSN 0021-9797. PMID 25596372.
- ^ Bai, Xuan; Xu, Lu; Tang, Jenny Y.; Zuo, Yi Y.; Hu, Guoqing (2019-10-01). "Adsorption of Phospholipids at the Air–Water Surface". Biophysical Journal. 117 (7): 1224–1233. Bibcode:2019BpJ...117.1224B. doi:10.1016/j.bpj.2019.08.022. ISSN 1542-0086. PMC 6818144. PMID 31519299.
- ^ Jackson, J. Craig (2012-01-01), Gleason, Christine A.; Devaskar, Sherin U. (eds.), "Chapter 46 - Respiratory Distress in the Preterm Infant", Avery's Diseases of the Newborn (Ninth Edition), W.B. Saunders, pp. 633–646, ISBN 9781437701340, retrieved 2019-10-25
- ^ Panzuela, S.; Tieleman, D. P.; Mederos, L.; Velasco, E. (2019-10-22). "Molecular Ordering in Lipid Monolayers: An Atomistic Simulation". Langmuir. 35 (42): 13782–13790. arXiv:1903.06659. Bibcode:2019arXiv190306659P. doi:10.1021/acs.langmuir.9b02635. ISSN 0743-7463. PMID 31553617.
- ^ Attwood, Simon J.; Choi, Youngjik; Leonenko, Zoya (2013-02-06). "Preparation of DOPC and DPPC Supported Planar Lipid Bilayers for Atomic Force Microscopy and Atomic Force Spectroscopy". International Journal of Molecular Sciences. 14 (2): 3514–3539. doi:10.3390/ijms14023514. ISSN 1422-0067. PMC 3588056. PMID 23389046.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Athenstaedt, K. (2010). "Neutral Lipids in Yeast: Synthesis, Storage and Degradation". Handbook of Hydrocarbon and Lipid Microbiology. pp. 471–480. doi:10.1007/978-3-540-77587-4_35. ISBN 978-3-540-77584-3.
- ^ Soll, Roger; Ozek, Eren (2010-01-20). "Prophylactic protein free synthetic surfactant for preventing morbidity and mortality in preterm infants". The Cochrane Database of Systematic Reviews (1): CD001079. doi:10.1002/14651858.CD001079.pub2. ISSN 1469-493X. PMC 7059181. PMID 20091513.
- ^ a b c Chattás, Lic. Guillermina (October 2013). "Administración de surfactante exógeno" (PDF). Revista Enfermería Neonatal. Nº 16: 10–17 – via Fundasamin.
- ^ Li, Jing; Wang, Xuling; Zhang, Ting; Wang, Chunling; Huang, Zhenjun; Luo, Xiang; Deng, Yihui (2015). "A review on phospholipids and their main applications in drug delivery systems". Asian Journal of Pharmaceutical Sciences. 10 (2): 81–98. doi:10.1016/j.ajps.2014.09.004.
- ^ Reference, Genetics Home. "Surfactant dysfunction". Genetics Home Reference. Retrieved 2019-10-24.
- ^ Reference, Genetics Home. "ABCA3 gene". Genetics Home Reference. Retrieved 2019-10-24.
- ^ Ashton, M. R.; Postle, A. D.; Hall, M. A.; Smith, S. L.; Kelly, F. J.; Normand, I. C. (April 1992). "Phosphatidylcholine composition of endotracheal tube aspirates of neonates and subsequent respiratory disease". Archives of Disease in Childhood. 67 (4 Spec No): 378–382. doi:10.1136/adc.67.4_spec_no.378. ISSN 1468-2044. PMC 1590480. PMID 1586174.
- ^ Luisoni, Stefania; Greber, Urs F. (2016-01-01), Curiel, David T. (ed.), "2 - Biology of Adenovirus Cell Entry: Receptors, Pathways, Mechanisms", Adenoviral Vectors for Gene Therapy (Second Edition), Academic Press, pp. 27–58, ISBN 9780128002766, retrieved 2019-10-25
