Dental sealant
Dental sealants (also termed pit and fissure sealants,[1] or simply fissure sealants)[2] are a dental treatment intended to prevent tooth decay. Teeth have recesses on their biting surfaces; the back teeth have fissures (grooves) and some front teeth have cingulum pits. It is these pits and fissures which are most vulnerable to tooth decay, partly because food sticks in them and they are hard to clean areas. Dental sealants are materials placed in these pits and fissures to fill them in, creating a smooth surface that is easy to clean. Dental sealants are mainly used in children who are at higher risk of tooth decay, and typically they are placed as soon as the adult molar teeth come through.
Background

Dental caries is an upset of the balance between loss and gain of minerals from a tooth surface.[3] The loss of minerals from our teeth occurs from the bacteria within our mouths fermenting foods and producing acids, whereas the tooth gains minerals from our saliva and fluoride that is present within our mouths.[3] When this balance is skewed due to frequent intake of fermentable carbohydrates, poor oral hygiene and lack of fluoride consumption there is a continuous loss and little gain of minerals over a long period of time, which can ultimately cause what we know as tooth decay.[3]
In our oral cavity, biting surfaces of back teeth are most susceptible to caries due to the presence of grooves & fissures which favours formation and retention of plaque.
Fissure sealants are a preventive treatment that is part of the minimal intervention dentistry approach to dental care.[4] This approach facilitates prevention and early intervention, in order to prevent or stop the dental caries process before it reaches the ends stage of the disease, which is also known as the "hole" or cavitation of a tooth.[4] Once the tooth is cavitated it requires a dental restoration in order to repair the damage, this emphasizes the importance of prevention in preserving our teeth for a lifetime of chewing.
Preventive treatment options for dental caries besides fissure sealants, involve promoting & education on toothbrushing technique with fluoride toothpaste, use of fluoride supplements & application of topical fluorides onto tooth surface.
The aim of fissure sealants is to prevent or arrest the development of dental caries.[5] Preventing tooth decay from the pits and fissures of the teeth is achieved by the fissure sealants providing a physical barricade to protect natural tooth surfaces and grooves, inhibiting build-up of bacteria & food trapped within such fissures & grooves. Fissure sealants also provide a smooth surface that is easily accessible for both our natural protective factor, saliva and the toothbrush bristles when cleaning our teeth.[5] Multiple oral health care professionals including a dentist, dental therapist, dental hygienist, an oral health therapist and dental assistants (in some states in the USA) are able to apply dental sealants to teeth.[5]
Dental sealants are a plastic material placed in the pits and fissures (the recesses on the chewing surfaces) of primary (baby) or permanent (adult) molar & premolar teeth at the back of the mouth. These molar teeth are considered the most susceptible teeth to dental caries due to the anatomy of the chewing surfaces of these teeth, which unfortunately inhibits protection from saliva and fluoride and instead favours plaque accumulation.[6]
History
There have been many attempts made within past decades to prevent the development of caries, in particular occlusal caries as it was once generally accepted that pits and fissures of teeth would become infected with bacteria within 10 years of erupting into the mouth.[7][8] G.V. Black, the creator of modern dentistry, informed that more than 40% of caries incidences in permanent teeth occurred in pits and fissures due to being able to retain food and plaque.[9]
One of the first attempts to prevent occlusal caries occurred as early as 1905 by Willoughby D. Miller.[7] Miller, a pioneer of dentistry, was applying silver nitrate to surfaces of teeth, chemically treating the biofilm with its antibacterial functions against both Streptococcus mutans and Actinomyces naeslundii, which are both carious pathogens.[7][8][9][10] Silver nitrate, which was also being practiced by H. Klein and J.W. Knutson in the 1940s, was being used in attempt to prevent and arrest occlusal caries.[9][11]
In 1921, T.P. Hyatt, a pioneer researcher, was the first person to recommend prophylactic odontotomy (preventive operation).[7][9][12] This procedure involved creating Class 1 cavity preps of teeth that were considered at risk of developing occlusal caries, which included all pits and fissures.[7][9][12] The widening of the pits and fissures were then filled with amalgam.[7][9][12]
C.F Bödecker, a dentist and researcher, also made attempts to prevent occlusal caries. Initially, in 1926 Bödecker would use a large round bur to smooth out the fissures. 1929, Bödecker attempted to prevent occlusal caries by cleaning the pit and fissures with an explorer and then sealing the pits and fissures with dental cement, such as oxyphosphate cement.[7] Bödecker then later became an advocator for prophylactic odontotomy procedures (preventive operations).[7][12]
It was in 1955, that M.G. Buonocore gave insight to the benefits of etching enamel with phosphoric acid.[7][8][9] His studies demonstrated that resin could be bonded to enamel through acid etching, increasing adhesion whilst also creating an improved marginal integrity of resin restorative material.[7][9] It was this bonding system that lead to the future successful creation of fissure sealants.[8][12]
In 1966, E.I. Cueto created the first sealant material, which was methyl cyanoacrylate.[7][13] However, this material was susceptible to bacterial breakdown over time, therefore was not an acceptable sealing material.[7] Bunonocore made further advances in 1970 by developing bisphenol-a glycidyl dimethacrylate, which is a viscous resin commonly known as BIS-GMA.[13] This material was used as the basis for many resin-based sealant/composite material developments in dentistry, as it is resistant to bacterial breakdown and forms a steady bond with etched enamel.[7][13]
In 1974, glass ionomer cement fissure seals (GIC) were introduced by J.W. McLean and A.D. Wilson.[13]
Modern sealant materials
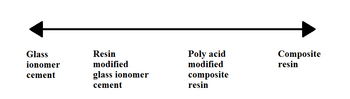
Modern dental sealants generally are either resin based or glass ionomer based.[1] Hybrid materials such as polyacid modified resin ("compomer") which lies between these two categories.[1]
Resin based sealants
It is customary to refer to the development of resin based sealants in generations:[13][14]
- First generation: set with UV curing.[14] They are no longer marketed.[13]
- Second generation: chemical-curing (autopolymerized).[13][14]
- Third generation: visible light-cured.[13][14]
- Fourth generation: contain fluoride.[13][14]
As part of the wider debate over the safety of bisphenol A (BPA), concerns have been raised over the use of resin based sealants.[13] BPA is a xenoestrogen, i.e. it mimics the relative bioactivity of estrogen, a female sex hormone. Pure BPA is rarely present in dental sealants, however they may contain BPA derivatives.[13] There is very little research about the potential estrogen-like effects of BPA derivatives.[13] A transient presence of BPA in saliva has been reported immediately following placement of some resin based sealants.[13] The longest duration of salivary BPA was 3 hours after placement, so there is little risk of chronic low-dose BPA exposure. The currently available evidence suggests that there is no risk of estrogen-like side effects with resin based sealants.[13] Several national dental organizations have published position statements regarding the safety of resin based dental materials, e.g. the American Dental Association,[nb 1] the Australian Dental Association,[nb 2] the British Dental Association,[nb 3] and the Canadian Dental Association.[nb 4]
Glass ionomer sealants
GIC materials bond both to enamel and dentine after being cleaned with polyacrylic acid conditioner.[7] Some other advantages GIC’s have is that they contain fluoride and are less moisture sensitive, with suggestions being made that despite having poor retention, they may prevent occlusal caries even after the sealant has fallen out due to their ability to release fluoride.[7][13][15]
Resin based sealants versus Glass ionomer sealants
It was shown that GIC materials were more effective in prevention of development of caries despite the higher non-successful rate compared to resin based sealants.[16] This may be accounted for due to the fluoride-releasing property of GIC which increases salivary fluoride level that may aid in preventing dental caries.
Resin-based sealants are normally the preferred choice of material for denture sealants. GIC material may be used as a provisional protective material when there are concerns regarding adequate moisture control.[17]
Effectiveness
Sealants are accepted as an effective preventive method for caries, and as long as the sealant remains adhered to the tooth, cavities can be prevented. It is for this reason that sealant success is now measured by the length of time a sealant remains on the tooth, rather than the decay experienced in sealed and unsealed teeth. The ability of a pit and fissure sealant to prevent dental caries is highly dependent on its ability to retain on the tooth surface.
It has been demonstrated that use of adhesive systems before applying dental sealants may improve retention.[18] Traditional retention of a sealant on tooth surface is through acid etching.
The most common reason for sealant failure is salivary contamination during sealing placement. Other factors include clinician inexperience, lack of client co-operation, and less effective sealant material used. [19]
Sealants may be in conjunction with fluoride varnish as a preventive method which is shown to be significantly more successful than fluoride varnish alone.[20]
Various factors can help contribute to the retention of fissure sealants. These include:
- Isolation of teeth from saliva
- Not placing sealants on partially erupted teeth as there is gingival tissue on the crown
- Good operator techniques
- Preparation of the fissure by cleaning out plaque and debris prior to placement [21]
Longevity
Although sealants do wear naturally and may become damaged over time, they have the potential to remain effective for five years or longer, despite the heavy pressures endured by teeth during chewing each day. Longevity of the dental sealants is also dependent on the type of material used for the fissure sealant.[22] It is not uncommon for fissure sealants to be retained into adulthood. It is believed that bacteria and food particles may eventually become entrapped under the dental sealants, and can thus cause decay in the very teeth intended to be protected.
This article needs additional citations for verification. (July 2015) |
Fissure sealants are inspected during routine dental visits to ensure that they are retained in the fissures of the teeth. One of the major causes to the loss of sealants in the first year is salivary contamination.[21]
On the basis of limited evidence both GIC and resin materials are equally acceptable in caries prevention, however retention rates between GIC and Resin have been shown to differ.[15] Resin has been shown to be the superior product for retention. A 2-year clinical trial comparing GIC and Resin for fissure sealants demonstrated that the GIC had a total loss rate of 31.78%, in contrast to the resin which had a total loss rate of 5.96% The study did acknowledge that GIC had its therapeutic advantages other than retention, this included the benefit of fluoride release and its use on partially erupted teeth.[23] Though GIC has poorer retention rates, the fact that they release active fluoride in the surrounding enamel is very important. They can exert a cariostatic effect and increased release of fluoride, and for these reasons GIC is more of a fluoride vehicle rather than a traditional fissure sealant.[24] All three materials are as effective as each other if the correct techniques are used to complete the procedure.[15]
Indications and contraindications
Indications for the use of dental sealants are individual patients or teeth that are at high risk of dental caries.
This includes patients with:
- A history of dental caries
- Deep retentive pits and fissures
- Early signs of dental caries
- Poor plaque control
- Enamel defects, such as enamel hypoplasia
- Orthodontics appliances.[25]
Contraindications for the use of dental sealants are individual patients or teeth that are at a low risk of dental caries:
This includes patients with:
- A balanced diet low in sugars or carbohydrates
- Exceptional oral hygiene
- Teeth with shallow, self-cleansing pits and fissures
- Teeth that a partially erupted without adequate moisture control (operators may choose to use GIC in these cases)
- Teeth with previously restored pits and fissures.[25]
Clinical procedure

The exact technique is dependent upon the material used and good application technique will increase retention of sealants which means sealants can last longer on the teeth. [26] Generally, each quadrant is treated separately by using four-handed technique with an assistant and to follow the manufacturer’s recommendations.[27] The patients should wear safety glasses for protection from chemicals and curing light. Once the patient is prepared, the surface of the tooth must be cleaned to allow maximum contact of the etch and the dental sealant with the enamel surface. A rubber dam may be used to prevent saliva from contaminating the intended site to be sealed, although often these are not used, especially for younger children. Moisture control is more of an issue with resin based sealants than with glass ionomer sealants. The surface is cleaned and dried.
Resin sealants require an phosphoric acid solution ("etch") to create microscopic porosity into which the sealant material can flow thereby increasing retention, increasing surface area and improving the strength of the bond between the sealant and the tooth surface.[28] Etching time varies from 15-60 second depending on the product. After that, the tooth must be rinsed and dried thoroughly for 15-20 seconds. Chalky appearance on the dried tooth means the tooth has been properly etched. If the tooth does not have this chalky appearance, the etching process must be repeated. The sealant is then applied to the tooth and either set with a curing light or left to dry by itself. Compared to a typical dental filling, where an injection of local anesthetic and use of a dental drill may be involved, fissure sealants are quick and painless. The sealant material is carefully placed into the prepared pits and fissures by using a disposable instrument provided by the manufacturer. Overfilling on the tooth should be prevented to minimize occlusal adjustment. The material is left for 10 seconds after the placement prior to curing to allow optimum penetration of the sealant materials into the pores created by the etching procedure. Usually, curing is 20-30 seconds. Glass ionomer do not require light curing, however they will set faster with the usage of a curing light.[29]
Resin-based sealants require an absolutely dry surface until polymerization is complete, so it is essential to avoid salivary contamination of the sealant site. A rubber dam or cotton roll isolation technique can be used to isolate the sealant site from saliva which is the common reason for sealant failure. Glass ionomer sealants have the advantage of not needing a dry field to be effective. In fact, the application procedure for glass ionomers can involve pressing a saliva-moistened finger onto the occlusal surface to push the sealant material into the pits and fissures.
Notes
- ^ Policy statement of the American Dental Association on Bisphenol A (BPA): "[B]ased on current evidence, the ADA does not believe there is a basis for health concerns relative to BPA exposure from any dental material."[1]
- ^ Policy statement of the Australian Dental Association on BPA (2014)[2]
- ^ Position statement of the British Dental Association on Bisphenol (2005): "More research is needed into the extent of any dental exposure (to bisphenol A) and into the general effects of Bisphenol A exposure, but as the majority of sealants and filling materials only contain Bis-GMA, there will be no resultant oestrogenic effect from using these materials."[3]
- ^ Canadian Dental Association page on frequently asked questions regarding BPA [4]
References
- ^ a b c Hiiri, A; Ahovuo-Saloranta, A; Nordblad, A; Mäkelä, M (17 March 2010). "Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents". The Cochrane database of systematic reviews (3): CD003067. doi:10.1002/14651858.CD003067.pub3. PMID 20238319.
- ^ Scheller-Sheridan, C (8 May 2013). Basic Guide to Dental Materials. John Wiley & Sons. pp. 74–78. ISBN 978-1-118-70831-6.
- ^ a b c Featherstone, JDB (2008). "Dental caries: A dynamic disease process". Australian Dental Journal. 53 (3): 286–91. doi:10.1111/j.1834-7819.2008.00064.x. PMID 18782377.
- ^ a b White J.M., & Eakle W.S. Rationale and Treatment Approach in Minimally Invasive Dentistry. Journal of the American Dental Association, 2000.
- ^ a b c Fissure sealants. http://www.dentalhealth.ie/download/pdf/fissure_sealant_booklet.pdf. Dental Health. Retrieved 2014-04-11.
- ^ Welbury, R; Raadal, M; Lygidakis, NA; European Academy of Paediatric, Dentistry (September 2004). "EAPD guidelines for the use of pit and fissure sealants" (PDF). European Journal of Paediatric Dentistry. 5 (3): 179–84. PMID 15471528.
- ^ a b c d e f g h i j k l m n o Avinash, J.; Marya, C.M.; Dhingra, S.; Gupta, P.; Kataria, S.; Meenu; Bhatia, H. P. (2010). "Pit and Fissure Sealants: An Unused Caries Prevention Tool" (PDF). Journal of Oral Health and Community Dentistry. 4 (1): 1–6.
- ^ a b c d Feigal, R. J.; Donly, K. J. (2006). "The Use of Pit and Fissure Sealants". Pediatric Dentistry. 28 (2): 143–150.
- ^ a b c d e f g h https://scholarworks.iupui.edu/bitstream/handle/1805/2078/view.pdf
- ^ Donovan, T. E.; Anderson, M.; Becker, W.; Cagna, D. R.; Carr, G. B.; Albouy, J.; Metz, J.; Eichmiller, F.; McKee, J. R. (2013). "Annual Review of selected dental literature: Report of the Committee on Scientific Investigation of the American Academy of Restorative Dentistry". The Journal of Prosthetic Dentistry. 110 (3): 161–210. doi:10.1016/S0022-3913(13)60358-3. PMID 24029608.
- ^ Knight, G. M.; McIntyre, J. M.; Craig, G. G.; Zilm, P. S.; Gully, N. J. (2005). "An in vitro model to measure the effect of a silver fluoride and potassium iodine treatment on the permeability of demineralized dentine to streptococcus mutans". Australian Dental Journal. 50 (4): 242–5. doi:10.1111/j.1834-7819.2005.tb00367.x. PMID 17016889.
- ^ a b c d e Zero, D. T. (2013). "How the introduction of the acid-etch technique revolutionized dental practice". The Journal of the American Dental Association. 144 (9): 990–994. doi:10.14219/jada.archive.2013.0224.
- ^ a b c d e f g h i j k l m n o Ahovuo-Saloranta, A; Forss, H; Walsh, T; Hiiri, A; Nordblad, A; Mäkelä, M; Worthington, HV (28 March 2013). "Sealants for preventing dental decay in the permanent teeth". The Cochrane database of systematic reviews. 3 (3): CD001830. doi:10.1002/14651858.CD001830.pub4. PMID 23543512.
- ^ a b c d e Hiremath, SS (15 August 2011). Textbook of Preventive and Community Dentistry. Elsevier India. pp. 428–432. ISBN 978-81-312-2530-1.
- ^ a b c Seth, S (2011). "Glass ionomer cement and resin-based fissure sealants are equally effective in caries prevention". JADA. 142 (5): 551–552. doi:10.14219/jada.archive.2011.0225.
- ^ "A 48-month randomised controlled trial of caries prevention effect of a one-time application of glass ionomer sealant versus resin sealant". PubMed.gov. June 2016. PMID 27086573.
- ^ "Dental Sealants Guidelines Development: 2002-2014". Paediatric Dentistry. 37 (2, March/April 2015).
- ^ Richards, Derek (1/12/2015). "Fissure sealants - are self-etch sealants more effective?".
{{cite web}}: Check date values in:|date=(help) - ^ Locker, D; Jokovic, A; Kay, EJ (2003). "Prevention. Part 8: The use of pit and fissure sealants in preventing caries in the permanent dentition of children". British Dental Journal. 195 (7): 375–8. doi:10.1038/sj.bdj.4810556. PMID 14551623.
- ^ "Pit & fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents". Cochcrane Library. 18 January 2016. doi:10.1002/14651858.CD003067.pub4/full (inactive 2016-11-22).
{{cite web}}: CS1 maint: DOI inactive as of November 2016 (link) - ^ a b Azarpazhooh, A; Main, PA (2008). "Pit and Fissure Sealants in the Prevention of Dental Caries in Children and Adolescents: A Systematic Review". Journal of the Canadian Dental Association. 74 (2): 171–7. PMID 18353204.
- ^ Deery, C (2012). "Pit and fissure sealant retention". Evidence-Based Dentistry. 13 (1): 9–10. doi:10.1038/sj.ebd.6400837. PMID 22436807.
- ^ Forss, H; Saarni, U-M; Seppä, L (1994). "Comparison of glass-ionomer and resin-based fissure sealants: a 2-year clinical trial". Community Dentistry and Oral Epidemiology. 22 (1): 21–4. doi:10.1111/j.1600-0528.1994.tb01563.x. PMID 8143437.
- ^ Beun, S.; Bailly, C.; Devaux, J.; Leloup, G. (2012). "Physical, mechanical and rheological characterisation of resin-based pit and fissure sealants compared to flowable resin composites". Dental Materials. 28 (4): 349–359. doi:10.1016/j.dental.2011.11.001.
- ^ a b Beauchamp, J. CPW; Crall, J.J.; Donly, K.; Feigal, R.; Gooch, B.; Ismail, A.; Kohn, W.; Siegal, M.; Simonsen, R. (2008). "Evidence-based clinical recommendations for the use of pit-and-fissure sealants: A report of the American Dental Association Council on Scientific Affairs". JADA: 139.
- ^ Griffin, Susan O.; Jones, Kari; Gray, Shellie Kolavic; Malvitz, Dolores M.; Gooch, Barbara F. (2008-04-01). "Exploring Four-Handed Delivery and Retention of Resin-Based Sealants". The Journal of the American Dental Association. 139 (3): 281–289. doi:10.14219/jada.archive.2008.0157. ISSN 0002-8177.
- ^ Griffin, Susan O.; Jones, Kari; Gray, Shellie Kolavic; Malvitz, Dolores M.; Gooch, Barbara F. (2008-04-01). "Exploring Four-Handed Delivery and Retention of Resin-Based Sealants". The Journal of the American Dental Association. 139 (3): 281–289. doi:10.14219/jada.archive.2008.0157. ISSN 0002-8177.
- ^ Frankenberger, R.; Tay, F. R. (2005). "Self-etch vs etch-and-rinse adhesives: Effect of thermo-mechanical fatigue loading on marginal quality of bonded resin composite restorations". Dental Materials. 21 (5): 397–412. doi:10.1016/j.dental.2004.07.005. PMID 15826696.
- ^ "Pit and Fissure Sealants: An Overview" (PDF).
{{cite journal}}: Cite journal requires|journal=(help)
