Internal urethral sphincter
| Internal urethral sphincter | |
|---|---|
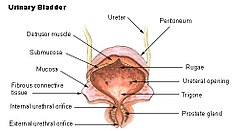 The urinary bladder, with the position of the internal urethral sphincter shown as the internal urethral orifice. | |
 Cross-section through the pelvis and the pubic arc, seen from in front, with surrounding soft tissues and bone shown. | |
| Details | |
| Origin | The inferior ramus of the pubic bone |
| Insertion | Perineal raphe |
| Nerve | Sympathetic fibers from T10-L2 through the inferior hypogastric plexus then vesical nervous plexus |
| Actions | Constricts proximal urethra, maintains urinary continence |
| Identifiers | |
| Latin | Musculus sphincter urethrae internus |
| TA98 | A09.2.03.009 A09.4.02.013 |
| TA2 | 3444, 3428 |
| FMA | 45769 |
| Anatomical terms of muscle | |
The internal urethral sphincter is a urethral sphincter muscle which constricts the internal urethral orifice. It is located at the junction of the urethra with the urinary bladder and is continuous with the detrusor muscle,[1][2] but anatomically and functionally fully independent from it.[3] It is composed of smooth muscle, so it is under the control of the autonomic nervous system, specifically the sympathetic nervous system.
Function
This is the primary muscle for maintaining continence of urine, a function shared with the external urethral sphincter which is under voluntary control. It prevents urine leakage as the muscle is tonically contracted via sympathetic fibers traveling through the inferior hypogastric plexus and vesical nervous plexus.[4] Specifically, it is controlled by the hypogastric nerve, predominantly via the alpha-1 receptor.[5]
During urination, the preganglionic neurons of this sympathetic pathway are inhibited via signals arising in the pontine micturition center and traveling through the descending reticulospinal tracts, allowing the muscle to relax. During ejaculation, the muscle contracts to prevent reflux of semen into the urinary bladder, a phenomenon called retrograde ejaculation.[6]
Spasms of the internal urethral sphincter are associated with penile erection.[7] Because the internal urethral sphincter is under involuntary control, it is believed to play a role in paruresis, in which a person who perceives oneself to be under observation is unable to urinate.
See also
- Detrusor muscle
- External sphincter muscle of female urethra
- External sphincter muscle of male urethra
- Urination#Physiology
References
![]() This article incorporates text in the public domain from page 429-431 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 429-431 of the 20th edition of Gray's Anatomy (1918)
- ^ Jung J, Ahn HK, and Huh Y (September 2012). "Clinical and Functional Anatomy of the Urethral Sphincter". Int Neurourol J. 16 (3): 102–106. doi:10.5213/inj.2012.16.3.102. PMC 3469827. PMID 23094214.
{{cite journal}}: Invalid|ref=harv(help) - ^ Sam P, LaGrange CA (February 2019). "Anatomy, Abdomen and Pelvis, Sphincter Urethrae". StatPearls [Internet]. PMID 29494045.
- ^ Dorschner W, Stolzenburg JU, Neuhaus J (2001). "Structure and function of the bladder neck". Advances in Anatomy, Embryology, and Cell Biology. 159: III–XII, 1–109. doi:10.1007/978-3-642-56879-4. ISBN 978-3-540-67998-1. PMID 11417142., page 29, Preview Amazon.
- ^ Shah AP, Mevcha A, Wilby D, Alatsatianos A, Hardman JC, Jacques S, Wilton JC (November 2014). "Continence and micturition: An anatomical basis" (PDF). Clin. Anat. 27 (8): 1275–1283. doi:10.1002/ca.22388. PMID 24615792.
{{cite journal}}: Invalid|ref=harv(help) - ^ Chancellor, M. B.; Yoshimura, N. (2004). "Neurophysiology of Stress Urinary Incontinence". Rev Urol. 6 Suppl 3: S19-28. PMC 1472861. PMID 16985861.
- ^ Moore, Keith L.; Dalley, Arthur F.; Agur, A. M. R. (2013-02-13). Clinically Oriented Anatomy. Lippincott Williams & Wilkins. p. 366. ISBN 9781451119459.
- ^ J. B. Macalpine (November 1934). "The Musculature of the Bladder-neck of the Male in Health and Disease". Proceedings of the Royal Society of Medicine. 28 (1): 39–56. doi:10.1177/003591573402800112. PMC 2205523. PMID 19990023.
