Portal:Viruses
The Viruses Portal
Welcome!
Viruses are small infectious agents that can replicate only inside the living cells of an organism. Viruses infect all forms of life, including animals, plants, fungi, bacteria and archaea. They are found in almost every ecosystem on Earth and are the most abundant type of biological entity, with millions of different types, although only about 6,000 viruses have been described in detail. Some viruses cause disease in humans, and others are responsible for economically important diseases of livestock and crops.
Virus particles (known as virions) consist of genetic material, which can be either DNA or RNA, wrapped in a protein coat called the capsid; some viruses also have an outer lipid envelope. The capsid can take simple helical or icosahedral forms, or more complex structures. The average virus is about 1/100 the size of the average bacterium, and most are too small to be seen directly with an optical microscope.
The origins of viruses are unclear: some may have evolved from plasmids, others from bacteria. Viruses are sometimes considered to be a life form, because they carry genetic material, reproduce and evolve through natural selection. However they lack key characteristics (such as cell structure) that are generally considered necessary to count as life. Because they possess some but not all such qualities, viruses have been described as "organisms at the edge of life".
Selected disease
Influenza, or flu, is an infectious disease caused by some orthomyxoviruses, that affects birds and some mammals including humans, horses and pigs. Influenza is predominantly transmitted through the air by coughs or sneezes, creating aerosols containing the virus. It can also be transmitted by contact with bird droppings or nasal secretions, or by touching contaminated surfaces. As the virus can be inactivated by soap, frequent hand washing reduces the risk of infection. Around a third of cases show no symptoms. The most common symptoms include fever, runny nose, sore throat, muscle pains, headache, cough and fatigue. Influenza is occasionally associated with nausea and vomiting, particularly in children. Pneumonia is a rare complication which can be life-threatening.
Influenza spreads around the world in seasonal epidemics, resulting in about 3–5 million cases of severe illness annually, and about 250,000–500,000 deaths, mainly in the young, the old and those with other health problems. Annual influenza vaccinations are recommended for those at high risk. Sporadic influenza pandemics have been recorded since at least the 16th century. The Spanish flu pandemic of 1918–20 is estimated to have killed 50–100 million people.
Selected image
HIV-1 budding from lymphocytes in culture. HIV establishes a latent infection in several types of immune cell and causes profound immunodeficiency.
Credit: C. Goldsmith (1984)
In the news
26 February: In the ongoing pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), more than 110 million confirmed cases, including 2.5 million deaths, have been documented globally since the outbreak began in December 2019. WHO
18 February: Seven asymptomatic cases of avian influenza A subtype H5N8, the first documented H5N8 cases in humans, are reported in Astrakhan Oblast, Russia, after more than 100,0000 hens died on a poultry farm in December. WHO
14 February: Seven cases of Ebola virus disease are reported in Gouécké, south-east Guinea. WHO
7 February: A case of Ebola virus disease is detected in North Kivu Province of the Democratic Republic of the Congo. WHO
4 February: An outbreak of Rift Valley fever is ongoing in Kenya, with 32 human cases, including 11 deaths, since the outbreak started in November. WHO
21 November: The US Food and Drug Administration (FDA) gives emergency-use authorisation to casirivimab/imdevimab, a combination monoclonal antibody (mAb) therapy for non-hospitalised people twelve years and over with mild-to-moderate COVID-19, after granting emergency-use authorisation to the single mAb bamlanivimab earlier in the month. FDA 1, 2
18 November: The outbreak of Ebola virus disease in Équateur Province, Democratic Republic of the Congo, which started in June, has been declared over; a total of 130 cases were recorded, with 55 deaths. UN
Selected article
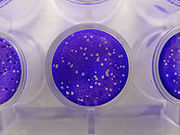
Virus quantification is necessary for viral vaccine production, and is used to manage people infected with HIV, hepatitis B and C, and cytomegalovirus. A wide range of traditional and modern methods are used. Plaque assays (pictured) infect a monolayer of host cells with dilutions of the virus and count the number of holes or plaques, where cells have lysed and infected their neighbours. For viruses that do not lyse their host cell, plaques of cells showing cytopathic effects can be counted or viral proteins can be immunostained with fluorescent-labelled antibodies. These methods quantify infectious virus, while others, such as electron microscopy, return a higher concentration because they count all virus particles, whether or not they are viable. Other assays, such as the haemagglutinin assay, quantify viral proteins.
Often slow and labour intensive, traditional methods have been complemented by modern technologies that greatly reduce quantification time, including quantitative polymerase chain reaction, flow cytometry, enzyme-linked immunosorbent assays and tunable resistive pulse sensing.
Selected outbreak
The West African Ebola epidemic was the most widespread outbreak of the disease to date. Beginning in Meliandou in southern Guinea in December 2013, it spread to adjacent Liberia and Sierra Leone, affecting the cities of Conakry and Monrovia, with minor outbreaks in Mali and Nigeria. Cases reached a peak in October 2014 and the epidemic was under control by late 2015, although occasional cases continued to occur into April 2016. Ring vaccination with the then-experimental vaccine rVSV-ZEBOV was trialled in Guinea.
More than 28,000 suspected cases were reported with more than 11,000 deaths; the case fatality rate was around 40% overall and around 58% in hospitalised patients. Early in the epidemic nearly 10% of the dead were healthcare workers. The outbreak left about 17,000 survivors, many of whom reported long-lasting post-recovery symptoms. Extreme poverty, dysfunctional healthcare systems, distrust of government after years of armed conflict, local burial customs of washing the body, the unprecedented spread of Ebola to densely populated cities, and the delay in response of several months all contributed to the failure to control the epidemic.
Selected quotation
| “ | Some scientists visualize the virus as an ill-defined shape emerging bashfully out of a dense and golden cloud. This is a beautiful and romantic vision. Virology should, however, not be too Turnerian. Nor should it be an abstract art. The portrait of a virus should not produce an aesthetic emotion by means of an organic disturbance. | ” |
Recommended articles
Viruses & Subviral agents: bat virome • elephant endotheliotropic herpesvirus • HIV • introduction to viruses![]() • Playa de Oro virus • poliovirus • prion • rotavirus
• Playa de Oro virus • poliovirus • prion • rotavirus![]() • virus
• virus![]()
Diseases: colony collapse disorder • common cold • croup • dengue fever![]() • gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza
• gastroenteritis • Guillain–Barré syndrome • hepatitis B • hepatitis C • hepatitis E • herpes simplex • HIV/AIDS • influenza![]() • meningitis
• meningitis![]() • myxomatosis • polio
• myxomatosis • polio![]() • pneumonia • shingles • smallpox
• pneumonia • shingles • smallpox
Epidemiology & Interventions: 2007 Bernard Matthews H5N1 outbreak • Coalition for Epidemic Preparedness Innovations • Disease X • 2009 flu pandemic • HIV/AIDS in Malawi • polio vaccine • Spanish flu • West African Ebola virus epidemic
Virus–Host interactions: antibody • host • immune system![]() • parasitism • RNA interference
• parasitism • RNA interference![]()
Methodology: metagenomics
Social & Media: And the Band Played On • Contagion • "Flu Season" • Frank's Cock![]() • Race Against Time: Searching for Hope in AIDS-Ravaged Africa
• Race Against Time: Searching for Hope in AIDS-Ravaged Africa![]() • social history of viruses
• social history of viruses![]() • "Steve Burdick" • "The Time Is Now" • "What Lies Below"
• "Steve Burdick" • "The Time Is Now" • "What Lies Below"
People: Brownie Mary • Macfarlane Burnet![]() • Bobbi Campbell • Aniru Conteh • people with hepatitis C
• Bobbi Campbell • Aniru Conteh • people with hepatitis C![]() • HIV-positive people
• HIV-positive people![]() • Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock
• Bette Korber • Henrietta Lacks • Linda Laubenstein • Barbara McClintock![]() • poliomyelitis survivors
• poliomyelitis survivors![]() • Joseph Sonnabend • Eli Todd • Ryan White
• Joseph Sonnabend • Eli Todd • Ryan White![]()
Selected virus
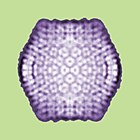
Sputnik virophage is a subviral agent, discovered in 2008, that infects Acanthamoeba protozoa. It is a satellite virus of giant viruses of the Mimiviridae family. It requires a mimivirus to infect the cell simultaneously to replicate, hijacking the virus factories that mimivirus creates and impairing its replication. Sputnik was the first satellite to be shown to inhibit the replication of its associated helper virus. Such viruses have been termed "virophages" or "virus eaters" – by analogy with bacteriophages, viruses that parasitise bacteria – but the distinction between virophages and classical satellite viruses that infect plants, arthropods and mammals is disputed. Three Sputnik types are now known, and other virophages have since been discovered, now classified in the Lavidaviridae family, including the Zamilon, Mavirus and Organic Lake virophages. All virophages that have been characterised infect protists and all rely on nucleocytoplasmic large DNA viruses as helpers.
Sputnik's non-enveloped icosahedral capsid is 74 nm in diameter, and contains a circular double-stranded DNA genome of 18.3 kb. Three of its 21 predicted protein-coding genes are thought to derive from Acanthamoeba polyphaga mimivirus, suggesting that virophages and giant viruses can swap genes during their joint infection of Acanthamoeba, and also that virophages might mediate horizontal gene transfer between giant viruses.
Did you know?
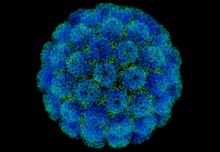
- ...that coccolithovirus (pictured, arrow), a giant double-stranded DNA virus, has 472 protein-coding genes, and was the largest known marine virus by genome until the 2013 discovery of Pandoravirus salinus?
- ...that Tony Minson developed a new way of disabling viruses for vaccines?
- ...that the Oscar Award-nominated film The Final Inch, a documentary about efforts to eradicate the poliovirus, is the first film project from Google's philanthropic division Google.org?
- ...that a June 5, 1981, report by Joel Weisman in MMWR about five gay men with an unusual illness is recognized as the start of the AIDS pandemic and "the first report on AIDS in the medical literature"?
- ...that elastomeric respirators are used not only to protect against COVID-19 and tear gas, but also as fashion items?
Selected biography
George Keble Hirst (2 March 1909 – 22 January 1994) was an American virologist who was among the first to study the molecular biology and genetics of animal viruses.
Hirst started to work on influenza virus in 1940, only a few years after it had been isolated. He soon discovered that the virus caused red blood cells to clump together. This phenomenon could be used to diagnose influenza, which had previously required growing the virus in ferrets. He invented the haemagglutination assay, a simple method for quantifying viruses, and later the haemagglutination inhibition assay, which measures virus-specific antibodies in serum. In 1942, he discovered the neuraminadase enzyme, showing for the first time that viruses could contain enzymes. Neuraminidase is the target of the neuraminidase inhibitor class of antiviral drugs, including oseltamivir and zanamivir. In 1962, he was also the first to propose the then-revolutionary idea that virus genomes can consist of discontinuous segments.
He co-founded Virology in 1955, the first English-language journal to focus on viruses, and directed the Public Health Research Institute in New York City for nearly 25 years (1956–81).
In this month
5 June 1981: First report of HIV/AIDS (symbol pictured) appeared in medical literature
6 June 1997: Gene silencing in plants shown to be a viral defence mechanism
7–13 June 1962: Donald Caspar and Aaron Klug proposed the quasi-equivalence principle of virus structure
7–13 June 1962: André Lwoff proposed a viral classification scheme based on nature of genome, type of symmetry and presence of envelope
7–13 June 1962: George Hirst proposed that the influenza virus genome is segmented
9 June 1981: The American Society for Virology was founded
13 June 2012: First case of Middle East respiratory syndrome coronavirus (MERS-CoV) occurred in Saudi Arabia
18 June 1981: A vaccine against foot-and-mouth disease was the first genetically engineered vaccine
21 June 1996: Nevirapine approved, first NNRTI for HIV/AIDS
26 June 1993: Clinical trial of hepatitis B virus drug fialuridine terminated; the drug caused several fatalities due to lactic acidosis
28 June 2011: FAO declared rinderpest eradicated
30 June 1985: Ryan White was denied re-admittance to his school after an AIDS diagnosis, in a case that changed public perceptions of the disease
Selected intervention
The first Ebola vaccine was approved in 2019. Developed by the Public Health Agency of Canada, rVSV-ZEBOV is based on an attenuated recombinant vesicular stomatitis virus, genetically modified to express a surface glycoprotein of Zaire ebolavirus, and is estimated to be 97.5% effective. In the Kivu Ebola epidemic of 2018–20, a ring vaccination strategy was employed to protect direct and indirect contacts of infected people, as well as health workers, and around 300,000 people were vaccinated with rVSV-ZEBOV. A second vaccine was approved in 2020; this uses two different doses – a vector based on human adenovirus serotype 26 used to prime, boosted around eight weeks later by modified vaccinia Ankara (based on a heavily attenuated vaccinia virus) – and is not suitable for response to an outbreak. The efficacy is unknown. Multiple other vaccine candidates are in development to prevent Ebola, including replication-deficient adenovirus vectors, replication-competent human parainfluenza 3 vectors, and virus-like nanoparticle preparations.
Subcategories
Subcategories of virology:
Topics
Things to do
- Comment on what you like and dislike about this portal
- Join the Viruses WikiProject
- Tag articles on viruses and virology with the project banner by adding {{WikiProject Viruses}} to the talk page
- Assess unassessed articles against the project standards
- Create requested pages: red-linked viruses | red-linked virus genera
- Expand a virus stub into a full article, adding images, citations, references and taxoboxes, following the project guidelines
- Create a new article (or expand an old one 5-fold) and nominate it for the main page Did You Know? section
- Improve a B-class article and nominate it for Good Article
 or Featured Article
or Featured Article status
status - Suggest articles, pictures, interesting facts, events and news to be featured here on the portal
WikiProjects & Portals
 WikiProject Viruses
Related WikiProjects
WikiProject Viruses
Related WikiProjects
Medicine • Microbiology • Molecular & Cellular Biology • Veterinary Medicine
Related PortalsAssociated Wikimedia
The following Wikimedia Foundation sister projects provide more on this subject:
-
Commons
Free media repository -
Wikibooks
Free textbooks and manuals -
Wikidata
Free knowledge base -
Wikinews
Free-content news -
Wikiquote
Collection of quotations -
Wikisource
Free-content library -
Wikispecies
Directory of species -
Wikiversity
Free learning tools -
Wiktionary
Dictionary and thesaurus