Odevixibat: Difference between revisions
| Line 117: | Line 117: | ||
Odevixibat is > 99% protein-bound in-vitro. <ref name=":0" /> A dose of Odevixibat that is 7.2 mg reaches a Cmax concentration of 0.47 ng/mL with an AUC (0-24h) of 2.19 h*ng/mL. <ref name=":1" /> Adult and pediatric patients given the therapeautic dose of Odevixibat did not display plasma concentrations of the drug. <ref name=":2" /> Odevixibat is eliminated majorly unchanged. <ref name=":1" /> Odevixibat has an average half-life of 2.36 hours.<ref name=":0" /> |
Odevixibat is > 99% protein-bound in-vitro. <ref name=":0" /> A dose of Odevixibat that is 7.2 mg reaches a Cmax concentration of 0.47 ng/mL with an AUC (0-24h) of 2.19 h*ng/mL. <ref name=":1" /> Adult and pediatric patients given the therapeautic dose of Odevixibat did not display plasma concentrations of the drug. <ref name=":2" /> Odevixibat is eliminated majorly unchanged. <ref name=":1" /> Odevixibat has an average half-life of 2.36 hours.<ref name=":0" /> |
||
The peak plasma time ranges from 1 to 5 hours after a single 7.2-mg dose in healthy adults. In healthy adults receiving a single 7.2-mg dose, the peak plasma concentration is 0.47 ng/mL, and the area under the concentration-time curve (AUC) is 2.19 ng·hr/mL. The plasma concentration of odevixibat in patients aged 6 months to 17 years ranges from 0.06 to 0.72 ng/mL. With once-daily dosing, there is no accumulation of odevixibat. |
The peak plasma time ranges from 1 to 5 hours after a single 7.2-mg dose in healthy adults. In healthy adults receiving a single 7.2-mg dose, the peak plasma concentration is 0.47 ng/mL, and the area under the concentration-time curve (AUC) is 2.19 ng·hr/mL. The plasma concentration of odevixibat in patients aged 6 months to 17 years ranges from 0.06 to 0.72 ng/mL. With once-daily dosing, there is no accumulation of odevixibat. <ref>{{Cite journal |last=Yu |first=Songlin |last2=Wang |first2=Danchen |last3=Yu |first3=Jialei |last4=Yin |first4=Yicong |last5=Xie |first5=Shaowei |last6=Cheng |first6=Qian |last7=Wang |first7=Xi |last8=Liu |first8=Wei |last9=Qiu |first9=Ling |last10=Cheng |first10=Xinqi |date=2021-03-31 |title=Plasma or serum, which is the better choice for the measurement of metanephrines? |url=http://dx.doi.org/10.1080/00365513.2021.1904280 |journal=Scandinavian Journal of Clinical and Laboratory Investigation |volume=81 |issue=3 |pages=250–253 |doi=10.1080/00365513.2021.1904280 |issn=0036-5513}}</ref> |
||
Odevixibat is metabolized through a process called mono-hydroxylation.The drug is primarily eliminated through the feces (97% unchanged), with a minimal amount excreted in the urine (0.002%). |
Odevixibat is metabolized through a process called mono-hydroxylation.The drug is primarily eliminated through the feces (97% unchanged), with a minimal amount excreted in the urine (0.002%). <ref>{{Cite journal |last=Ray |first=Katrina |date=2022-07-25 |title=Positive phase III results for odevixibat for progressive familial intrahepatic cholestasis |url=http://dx.doi.org/10.1038/s41575-022-00667-x |journal=Nature Reviews Gastroenterology & Hepatology |volume=19 |issue=9 |pages=556–556 |doi=10.1038/s41575-022-00667-x |issn=1759-5045}}</ref> |
||
Consuming a high-fat meal (800-1000 calories with approximately 50% of the total caloric content from fat) the peak plasma concentration is decreased by 72%, the AUC by 62%, and delays the peak plasma time by 3 to 4.5 hours. However, the impact of food on systemic exposures to odevixibat [C1]is not clinically significant. |
Consuming a high-fat meal (800-1000 calories with approximately 50% of the total caloric content from fat) the peak plasma concentration is decreased by 72%, the AUC by 62%, and delays the peak plasma time by 3 to 4.5 hours. However, the impact of food on systemic exposures to odevixibat [C1]is not clinically significant. <ref>{{Cite journal |last=Taylor |first=Lesley |last2=Gidal |first2=Barry |last3=Blakey |first3=Graham |last4=Tayo |first4=Bola |last5=Morrison |first5=Gilmour |date=2018-10-30 |title=A Phase I, Randomized, Double-Blind, Placebo-Controlled, Single Ascending Dose, Multiple Dose, and Food Effect Trial of the Safety, Tolerability and Pharmacokinetics of Highly Purified Cannabidiol in Healthy Subjects |url=http://dx.doi.org/10.1007/s40263-018-0578-5 |journal=CNS Drugs |volume=32 |issue=11 |pages=1053–1067 |doi=10.1007/s40263-018-0578-5 |issn=1172-7047}}</ref> |
||
== Adverse effects == |
== Adverse effects == |
||
| Line 130: | Line 130: | ||
== History == |
== History == |
||
Preclinical studies and early clinical trials were conducted to evaluate the safety and efficacy of odevixibat, to establish the appropriate dosage, assess its mechanism of action, and evaluate its effects on bile acid levels and symptoms in patients with PFIC. A 24-week clinical trial, played a crucial role in demonstrating the effectiveness and safety of odevixibat in treating pruritus in children with PFIC. |
Preclinical studies and early clinical trials were conducted to evaluate the safety and efficacy of odevixibat, to establish the appropriate dosage, assess its mechanism of action, and evaluate its effects on bile acid levels and symptoms in patients with PFIC. A 24-week clinical trial, played a crucial role in demonstrating the effectiveness and safety of odevixibat in treating pruritus in children with PFIC. <ref>{{Cite journal |last=Ray |first=Katrina |date=2022-07-25 |title=Positive phase III results for odevixibat for progressive familial intrahepatic cholestasis |url=http://dx.doi.org/10.1038/s41575-022-00667-x |journal=Nature Reviews Gastroenterology & Hepatology |volume=19 |issue=9 |pages=556–556 |doi=10.1038/s41575-022-00667-x |issn=1759-5045}}</ref> |
||
placebo-controlled, phase 3 trial - The Lancet Gastroenterology & Hepatology) |
|||
The US [[Food and Drug Administration]] granted the application for odevixibat [[orphan drug]] designation.<ref name="New Drug Therapy Approvals 2021" /> |
The US [[Food and Drug Administration]] granted the application for odevixibat [[orphan drug]] designation.<ref name="New Drug Therapy Approvals 2021" /> |
||
Odevixibat was granted its initial approval on July 16, 2021, in the European Union (EU) for the treatment of Progressive Familial Intrahepatic Cholestasis (PFIC) in patients aged 6 months and older. Subsequently, on July 20, 2021, it received approval in the United States for the treatment of pruritus (itching) in patients aged 3 months and older with PFIC |
Odevixibat was granted its initial approval on July 16, 2021, in the European Union (EU) for the treatment of Progressive Familial Intrahepatic Cholestasis (PFIC) in patients aged 6 months and older. Subsequently, on July 20, 2021, it received approval in the United States for the treatment of pruritus (itching) in patients aged 3 months and older with PFIC. <ref>{{Cite journal |last=Deeks |first=Emma D. |date=2021-09-09 |title=Odevixibat: First Approval |url=http://dx.doi.org/10.1007/s40265-021-01594-y |journal=Drugs |volume=81 |issue=15 |pages=1781–1786 |doi=10.1007/s40265-021-01594-y |issn=0012-6667}}</ref> |
||
== Society and culture == |
== Society and culture == |
||
Revision as of 14:34, 15 June 2023
 | |
| Clinical data | |
|---|---|
| Trade names | Bylvay |
| Other names | A4250 |
| License data |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
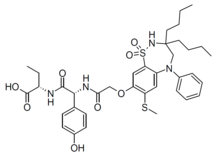
| Formula | C37H48N4O8S2 |
| Molar mass | 740.93 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Odevixibat, sold under the trade name Bylvay, is a medication for the treatment of progressive familial intrahepatic cholestasis (PFIC).[1][4] It is taken by mouth.[1]
Odevixibat serves as a non-surgical option to help patients with PFIC by disturbing the enterohepatic circulation. Odevixibat is a reversible, potent, selective, small molecule inhibitor of the ileal bile acid transporter (IBAT).[4][5][6]
The most common side effects include diarrhea, abdominal pain, hemorrhagic diarrhea, soft feces, and hepatomegaly (enlarged liver).[4]
Odevixibat was approved for medical use in the United States and in the European Union in July 2021.[1][2][3][7][8] The U.S. Food and Drug Administration considers it to be a first-in-class medication.[9]
Medical uses
In the United States, odevixibat is indicated for the treatment of pruritus in people three months of age and older with progressive familial intrahepatic cholestasis (PFIC).[1] In the European Union it is indicated in people six months of age and older.[2][3] In a phase 3, randomized control trial, it showed Odevixibat effectively reduced pruritis and serum bile acids in children with PFIC.[1]
Mechanism of action
Odevixibat is a reversible inhibitor of the ileal sodium/bile acid co-transporter which is the transporter responsible for reabsorption of the majority of bile acids in the distal ileum. [10] The reduced absorption of the bile acids in the distal ileum compounds and leads to a decrease in stimulation of FXR, decreasing the inhibition of bile acid synthesis.[11]
Pharmacokinetics
Odevixibat is > 99% protein-bound in-vitro. [11] A dose of Odevixibat that is 7.2 mg reaches a Cmax concentration of 0.47 ng/mL with an AUC (0-24h) of 2.19 h*ng/mL. [12] Adult and pediatric patients given the therapeautic dose of Odevixibat did not display plasma concentrations of the drug. [8] Odevixibat is eliminated majorly unchanged. [12] Odevixibat has an average half-life of 2.36 hours.[11]
The peak plasma time ranges from 1 to 5 hours after a single 7.2-mg dose in healthy adults. In healthy adults receiving a single 7.2-mg dose, the peak plasma concentration is 0.47 ng/mL, and the area under the concentration-time curve (AUC) is 2.19 ng·hr/mL. The plasma concentration of odevixibat in patients aged 6 months to 17 years ranges from 0.06 to 0.72 ng/mL. With once-daily dosing, there is no accumulation of odevixibat. [13]
Odevixibat is metabolized through a process called mono-hydroxylation.The drug is primarily eliminated through the feces (97% unchanged), with a minimal amount excreted in the urine (0.002%). [14]
Consuming a high-fat meal (800-1000 calories with approximately 50% of the total caloric content from fat) the peak plasma concentration is decreased by 72%, the AUC by 62%, and delays the peak plasma time by 3 to 4.5 hours. However, the impact of food on systemic exposures to odevixibat [C1]is not clinically significant. [15]
Adverse effects
Common side effects of Odevixibat include diarrhea, stomach pain, vomiting, abnormal liquid function tests, and a deficiency in vitamins A,D, E and K. [11]
Contraindications
Odevixibat cannot be given to a child on a liquid diet. [12]
History
Preclinical studies and early clinical trials were conducted to evaluate the safety and efficacy of odevixibat, to establish the appropriate dosage, assess its mechanism of action, and evaluate its effects on bile acid levels and symptoms in patients with PFIC. A 24-week clinical trial, played a crucial role in demonstrating the effectiveness and safety of odevixibat in treating pruritus in children with PFIC. [16]
The US Food and Drug Administration granted the application for odevixibat orphan drug designation.[9]
Odevixibat was granted its initial approval on July 16, 2021, in the European Union (EU) for the treatment of Progressive Familial Intrahepatic Cholestasis (PFIC) in patients aged 6 months and older. Subsequently, on July 20, 2021, it received approval in the United States for the treatment of pruritus (itching) in patients aged 3 months and older with PFIC. [17]
Society and culture
Legal status
In May 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommended granting a marketing authorization in the European Union for odevixibat for the treatment of PFIC in people aged six months or older.[4][18] It was approved for medical use in the European Union in July 2021.[2][3]
References
- ^ a b c d e "Bylvay- odevixibat capsule, coated pellets". DailyMed. Retrieved 28 July 2021.
- ^ a b c d "Bylvay EPAR". European Medicines Agency (EMA). 20 April 2021. Retrieved 28 July 2021.
- ^ a b c d "Bylvay". Union Register of medicinal products. Retrieved 23 July 2021.
- ^ a b c d "First treatment for rare liver disease". European Medicines Agency (EMA) (Press release). 21 May 2021. Retrieved 21 May 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ "Odevixibat". Albireo Pharma. Retrieved 21 May 2021.
- ^ Karpen SJ, Kelly D, Mack C, Stein P (September 2020). "Ileal bile acid transporter inhibition as an anticholestatic therapeutic target in biliary atresia and other cholestatic disorders". Hepatology International. 14 (5): 677–689. doi:10.1007/s12072-020-10070-w. PMID 32653991. S2CID 220481607.
- ^ "Odevixibat: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 23 July 2021.
- ^ a b "Albireo Announces FDA Approval of Bylvay (odevixibat), the First Drug Treatment for Patients With Progressive Familial Intrahepatic Cholestasis (PFIC)". Albireo Pharma (Press release). 20 July 2021. Retrieved 23 July 2021 – via GlobeNewswire.
- ^ a b Advancing Health Through Innovation: New Drug Therapy Approvals 2021 (PDF). U.S. Food and Drug Administration (FDA) (Report). 13 May 2022. Archived from the original on 6 December 2022. Retrieved 22 January 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Odevixibat". go.drugbank.com. Retrieved 13 June 2022.
- ^ a b c d "Odevixibat Uses, Side Effects & Warnings". Drugs.com. Retrieved 11 June 2022.
- ^ a b c "Odevixibat Uses, Side Effects & Warnings". Drugs.com. Retrieved 11 June 2022.
- ^ Yu, Songlin; Wang, Danchen; Yu, Jialei; Yin, Yicong; Xie, Shaowei; Cheng, Qian; Wang, Xi; Liu, Wei; Qiu, Ling; Cheng, Xinqi (31 March 2021). "Plasma or serum, which is the better choice for the measurement of metanephrines?". Scandinavian Journal of Clinical and Laboratory Investigation. 81 (3): 250–253. doi:10.1080/00365513.2021.1904280. ISSN 0036-5513.
- ^ Ray, Katrina (25 July 2022). "Positive phase III results for odevixibat for progressive familial intrahepatic cholestasis". Nature Reviews Gastroenterology & Hepatology. 19 (9): 556–556. doi:10.1038/s41575-022-00667-x. ISSN 1759-5045.
- ^ Taylor, Lesley; Gidal, Barry; Blakey, Graham; Tayo, Bola; Morrison, Gilmour (30 October 2018). "A Phase I, Randomized, Double-Blind, Placebo-Controlled, Single Ascending Dose, Multiple Dose, and Food Effect Trial of the Safety, Tolerability and Pharmacokinetics of Highly Purified Cannabidiol in Healthy Subjects". CNS Drugs. 32 (11): 1053–1067. doi:10.1007/s40263-018-0578-5. ISSN 1172-7047.
- ^ Ray, Katrina (25 July 2022). "Positive phase III results for odevixibat for progressive familial intrahepatic cholestasis". Nature Reviews Gastroenterology & Hepatology. 19 (9): 556–556. doi:10.1038/s41575-022-00667-x. ISSN 1759-5045.
- ^ Deeks, Emma D. (9 September 2021). "Odevixibat: First Approval". Drugs. 81 (15): 1781–1786. doi:10.1007/s40265-021-01594-y. ISSN 0012-6667.
- ^ "Bylvay: Pending EC decision". European Medicines Agency (EMA). 19 May 2021. Archived from the original on 21 May 2021. Retrieved 21 May 2021.
External links
- "Odevixibat". Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT03566238 for "This Study Will Investigate the Efficacy and Safety of A4250 in Children With PFIC 1 or 2 (PEDFIC 1)" at ClinicalTrials.gov
