Adenocarcinoma in situ of the lung: Difference between revisions
Typo/Style: Changed possessive BAC's to plural BACs |
m →Cite journal with Wikipedia template filling, tweak cites, partial |
||
| Line 17: | Line 17: | ||
==Classification== |
==Classification== |
||
[[File:Bronchioloalveolar carcinoma.jpg|thumb|Gross pathology photograph from the lungs of a patient who died of widespread bilateral BAC. A cut surface of the formalin-inflated lungs shows multiple, small, gray-white nodules with absence of necrosis, hemorrhage, or architectural distortion. The bronchi course normally through the lung tissue, and the presence of air bronchograms radiographically in such cases is not surprising.]] |
[[File:Bronchioloalveolar carcinoma.jpg|thumb|Gross pathology photograph from the lungs of a patient who died of widespread bilateral BAC. A cut surface of the formalin-inflated lungs shows multiple, small, gray-white nodules with absence of necrosis, hemorrhage, or architectural distortion. The bronchi course normally through the lung tissue, and the presence of air bronchograms radiographically in such cases is not surprising.]] |
||
Lung cancers are an extremely [[heterogeneous]] family of malignant [[neoplasms]],<ref name='RoggliVollmer'>Roggli VL, Vollmer RT, Greenberg SD, McGavran MH, Spjut HJ, Yesner R |
Lung cancers are an extremely [[heterogeneous]] family of malignant [[neoplasms]],<ref name='RoggliVollmer'>{{cite journal |author=Roggli VL, Vollmer RT, Greenberg SD, McGavran MH, Spjut HJ, Yesner R |title=Lung cancer heterogeneity: a blinded and randomized study of 100 consecutive cases |journal=Hum. Pathol. |volume=16 |issue=6 |pages=569–79 |year=1985 |month=June |pmid=2987102 }}</ref> with well over 50 different histological variants recognized under the 2004 revision of the [[World Health Organization]] ("WHO-2004") typing system, currently the most widely used lung cancer classification scheme.<ref name='who2004' /> Because these variants can have widely differing genetic, biological, and clinical properties, including response to treatment, correct classification of lung cancer cases are necessary to assure that lung cancer patients receive optimum management.<ref name='RossiMarchioni'>{{cite journal |author=Rossi G, Marchioni A, Sartori1 G, Longo L, Piccinini S, Cavazza A |title=Histotype in non-small cell lung cancer therapy and staging: The emerging role of an old and underrated factor |journal=Curr Resp Med Rev |volume=3 |pages=69–77 |year=2007 |doi=10.2174/157339807779941820 |url=http://www.ingentaconnect.com/content/ben/crmr/2007/00000003/00000001/art00011}}</ref><ref name='Vincent'>{{cite journal |author=Vincent MD |title=Optimizing the management of advanced non-small-cell lung cancer: a personal view |journal=Curr Oncol |volume=16 |issue=4 |pages=9–21 |year=2009 |month=August |pmid=19672420 |pmc=2722061 |url=http://www.current-oncology.com/index.php/oncology/article/view/465/374;}}</ref> |
||
Approximately 98% of lung cancers are [[carcinoma]], which are tumors composed of cells with [[epithelial]] characteristics.<ref name='TravisTravis'>Travis WD, Travis LB, |
Approximately 98% of lung cancers are [[carcinoma]], which are tumors composed of cells with [[epithelial]] characteristics.<ref name='TravisTravis'>{{cite journal |author=Travis WD, Travis LB, Devesa SS |title=Lung cancer |journal=Cancer |volume=75 |issue=1 Suppl |pages=191–202 |year=1995 |month=January |pmid=8000996 }}</ref> 8 major groups of lung carcinomas are recognized in WHO-2004:<ref name='who2004'>{{cite book |title=Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart |editor1-last=Travis |editor1-first=William D |editor2-last=Brambilla |editor2-first=Elisabeth |editor3-last=Muller-Hermelink |editor3-first=H Konrad |editor4-last=Harris |editor4-first=Curtis C |publisher=IARC Press |location=Lyon |year=2004 |series=World Health Organization Classification of Tumours |isbn=92 832 2418 3 |url=http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/bb10-cover.pdf |accessdate=27 March 2010}}</ref> |
||
*Squamous Cell Carcinoma |
*Squamous Cell Carcinoma |
||
| Line 32: | Line 32: | ||
In WHO-2004, BACs are one of four specific histologic subtypes of [[lung cancer|lung adenocarcinoma]], along with [[acinar adenocarcinoma]], [[papillary adenocarcinoma]], and [[solid adenocarcinoma with mucin production]]. However, approximately 80% of adenocarcinomas are found to contain two (or more) of these four subtypes. Multiphasic tumors such as these are classified into a fifth "subtype", termed [[adenocarcinoma with mixed subtypes]].<ref name='who2004'>Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC (Eds.): World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. IARC Press: Lyon 2004.</ref> |
In WHO-2004, BACs are one of four specific histologic subtypes of [[lung cancer|lung adenocarcinoma]], along with [[acinar adenocarcinoma]], [[papillary adenocarcinoma]], and [[solid adenocarcinoma with mucin production]]. However, approximately 80% of adenocarcinomas are found to contain two (or more) of these four subtypes. Multiphasic tumors such as these are classified into a fifth "subtype", termed [[adenocarcinoma with mixed subtypes]].<ref name='who2004'>Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC (Eds.): World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. IARC Press: Lyon 2004.</ref> |
||
There are other classification systems that have been proposed for lung cancers, including BACs and other forms of adenocarcinoma. The Noguchi classification system for small adenocarcinomas has received considerable attention, particularly in Japan, but has not been nearly as widely applied and recognized as the WHO system.<ref name='NoguchiMorikawa'>Noguchi M, Morikawa A, Kawasaki M, |
There are other classification systems that have been proposed for lung cancers, including BACs and other forms of adenocarcinoma. The Noguchi classification system for small adenocarcinomas has received considerable attention, particularly in Japan, but has not been nearly as widely applied and recognized as the WHO system.<ref name='NoguchiMorikawa'>{{cite journal |author=Noguchi M, Morikawa A, Kawasaki M, ''et al.'' |title=Small adenocarcinoma of the lung. Histologic characteristics and prognosis |journal=Cancer |volume=75 |issue=12 |pages=2844–52 |year=1995 |month=June |pmid=7773933 }}</ref> |
||
Like other forms of lung carcinoma, BAC possesses unique clinical and pathological features, prognosis, and responses to different treatments.<ref name=' VarlottoFlickinger'>Varlotto JM, Flickinger JC, Recht A, Nikolov MC, DeCamp MM. Comparison of survival and disease-specific survival in surgically resected, lymph node-positive bronchioloalveolar carcinoma versus nonsmall cell lung cancer. ''Cancer'' 2008; 112:1547-54.</ref> |
Like other forms of lung carcinoma, BAC possesses unique clinical and pathological features, prognosis, and responses to different treatments.<ref name=' VarlottoFlickinger'>Varlotto JM, Flickinger JC, Recht A, Nikolov MC, DeCamp MM. Comparison of survival and disease-specific survival in surgically resected, lymph node-positive bronchioloalveolar carcinoma versus nonsmall cell lung cancer. ''Cancer'' 2008; 112:1547-54.</ref> |
||
| Line 44: | Line 44: | ||
BAC is the only lung cancer, besides Carcinoid, not associated with smoking,(more common in non-smokers, women and Asians).<ref>{{cite journal |author=Raz DJ, He B, Rosell R, Jablons DM |title=Bronchioloalveolar carcinoma: a review |journal=Clin Lung Cancer |volume=7 |issue=5 |pages=313–22 |year=2006 |month= March|pmid=16640802 |doi=10.3816/CLC.2006.n.012 }}</ref> The criteria for diagnosing BAC have changed since 1999.<ref name="WHO1999"/> Under the new definition, BAC is not considered to be an invasive tumor by [[Surgical pathology|pathologists]], but as one form of [[carcinoma in situ]] (CIS). Like other forms of CIS, BAC may progress and become overtly invasive, exhibiting [[malignant]], often lethal, behavior. Major surgery, either a [[lobectomy]] or a [[pneumonectomy]], is usually needed to control it, and like other forms of [[non-small cell lung carcinoma]], recurrences are frequent. Therefore, [[Oncology|oncologists]] classify it among the other malignant tumors, which are [[cancer|invasive tumors]].<ref name="who2004"/> |
BAC is the only lung cancer, besides Carcinoid, not associated with smoking,(more common in non-smokers, women and Asians).<ref>{{cite journal |author=Raz DJ, He B, Rosell R, Jablons DM |title=Bronchioloalveolar carcinoma: a review |journal=Clin Lung Cancer |volume=7 |issue=5 |pages=313–22 |year=2006 |month= March|pmid=16640802 |doi=10.3816/CLC.2006.n.012 }}</ref> The criteria for diagnosing BAC have changed since 1999.<ref name="WHO1999"/> Under the new definition, BAC is not considered to be an invasive tumor by [[Surgical pathology|pathologists]], but as one form of [[carcinoma in situ]] (CIS). Like other forms of CIS, BAC may progress and become overtly invasive, exhibiting [[malignant]], often lethal, behavior. Major surgery, either a [[lobectomy]] or a [[pneumonectomy]], is usually needed to control it, and like other forms of [[non-small cell lung carcinoma]], recurrences are frequent. Therefore, [[Oncology|oncologists]] classify it among the other malignant tumors, which are [[cancer|invasive tumors]].<ref name="who2004"/> |
||
Under the new, more restrictive WHO criteria for lung cancer classification, BAC is now diagnosed much less frequently than it was in the past.<ref name="who2004"/> Recent studies suggest that BAC comprises between 3% and 5% of all lung carcinomas in the U.S.<ref name='ZellOu'>Zell JA, Ou SH, Ziogas A, Anton-Culver H |
Under the new, more restrictive WHO criteria for lung cancer classification, BAC is now diagnosed much less frequently than it was in the past.<ref name="who2004"/> Recent studies suggest that BAC comprises between 3% and 5% of all lung carcinomas in the U.S.<ref name='ZellOu'>{{cite journal |author=Zell JA, Ou SH, Ziogas A, Anton-Culver H |title=Epidemiology of bronchioloalveolar carcinoma: improvement in survival after release of the 1999 WHO classification of lung tumors |journal=J. Clin. Oncol. |volume=23 |issue=33 |pages=8396–405 |year=2005 |month=November |pmid=16293870 |doi=10.1200/JCO.2005.03.0312 |url=http://www.jco.org/cgi/pmidlookup?view=long&pmid=16293870}}</ref><ref name='ReadPage'>{{cite journal |author=Read WL, Page NC, Tierney RM, Piccirillo JF, Govindan R |title=The epidemiology of bronchioloalveolar carcinoma over the past two decades: analysis of the SEER database |journal=Lung Cancer |volume=45 |issue=2 |pages=137–42 |year=2004 |month=August |pmid=15246183 |doi=10.1016/j.lungcan.2004.01.019 |url=http://linkinghub.elsevier.com/retrieve/pii/S0169500204000546}}</ref> |
||
==Variants of BAC== |
==Variants of BAC== |
||
BAC occurs in two major histopathological variants, '''mucinous''' BAC (m-BAC, 20%-25% of cases)<ref name='YoussemBeasley'>Yousem SA, Beasley MB |
BAC occurs in two major histopathological variants, '''mucinous''' BAC (m-BAC, 20%-25% of cases)<ref name='YoussemBeasley'>{{cite journal |author=Yousem SA, Beasley MB |title=Bronchioloalveolar carcinoma: a review of current concepts and evolving issues |journal=Arch. Pathol. Lab. Med. |volume=131 |issue=7 |pages=1027–32 |year=2007 |month=July |pmid=17616987 |doi=10.1043/1543-2165(2007)131[1027:BCAROC]2.0.CO;2 |url=http://www.archivesofpathology.org/doi/full/10.1043/1543-2165(2007)131[1027:BCAROC]2.0.CO;2}}</ref><ref name='RazHe'>{{cite journal |author=Raz DJ, He B, Rosell R, Jablons DM |title=Current concepts in bronchioloalveolar carcinoma biology |journal=Clin. Cancer Res. |volume=12 |issue=12 |pages=3698–704 |year=2006 |month=June |pmid=16778095 |doi=10.1158/1078-0432.CCR-06-0457 |url=http://clincancerres.aacrjournals.org/cgi/pmidlookup?view=long&pmid=16778095}}</ref> and '''non mucinous''' BAC (nm-BAC, 75%-80% of cases).<ref name='RazHe'/><ref>{{cite journal |author=Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL |title=Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings |journal=Radiographics |volume=17 |issue=6 |pages=1345–57 |date=1 November 1997|pmid=9397450 |url=http://radiographics.rsnajnls.org/cgi/reprint/17/6/1345 }}</ref> Very rarely, BAC can also occur as a '''"mixed mucinous and non-mucinous"''' (or "indeterminant") variant.<ref name="who2004"/> |
||
==Incidence== |
==Incidence== |
||
The incidence of bronchiolo-alveolar carcinoma has been reported to vary from |
The incidence of bronchiolo-alveolar carcinoma has been reported to vary from 4–24% of all lung cancer patietnts.<ref name='ReadPage'>{{cite journal|last=Read|first=WL|coauthors=Page, NC, Tierney, RM, Piccirillo, JF, Govindan, R|title=The epidemiology of bronchioloalveolar carcinoma over the past two decades: analysis of the SEER database.|journal=Lung cancer (Amsterdam, Netherlands)|date=August 2004|volume=45|issue=2|pages=137–42|pmid=15246183}}</ref> An analysis of Surveillance epidemiology and End results registry ( SEER) by Read ''et al.'' revealed that although the incidence of BAC has increased over the past two decade it still constitutes less than 4% of NSCLC in every time interval.<ref name='ReadPage'/> This difference in the incidence has been attributed to complex histopathology of cancer. While pure BAC is rare, the increase in incidence as seen in various studies can be due to unclear histological classification till WHO came up with its classification in 1999 and then in 20044. |
||
Another distinguishing feature about BAC is that it afflicts men and women in equal proportions, some recent studies even suggest slightly higher incidence among women. <ref |
Another distinguishing feature about BAC is that it afflicts men and women in equal proportions, some recent studies even suggest slightly higher incidence among women. <ref name='ZellOu'/><ref name='ReadPage'/> |
||
==Histogenesis== |
==Histogenesis== |
||
Nonmucinous BAC is thought to derive from a transformed cell in the [[distal]] airways and terminal respiratory units, and often shows features of [[Clara cell]] or [[Type II pneumocyte]] differentiation.<ref name="YoussemBeasley"/> Mucinous BAC, in contrast, probably derives from a transformed glandular cell in distal bronchioles.<ref name='ChilosiMurer'>Chilosi M, Murer B |
Nonmucinous BAC is thought to derive from a transformed cell in the [[distal]] airways and terminal respiratory units, and often shows features of [[Clara cell]] or [[Type II pneumocyte]] differentiation.<ref name="YoussemBeasley"/> Mucinous BAC, in contrast, probably derives from a transformed glandular cell in distal bronchioles.<ref name='ChilosiMurer'>{{cite journal |author=Chilosi M, Murer B |title=Mixed adenocarcinomas of the lung: place in new proposals in classification, mandatory for target therapy |journal=Arch. Pathol. Lab. Med. |volume=134 |issue=1 |pages=55–65 |year=2010 |month=January |pmid=20073606 |doi=10.1043/1543-2165-134.1.55 |url=http://www.archivesofpathology.org/doi/full/10.1043/1543-2165-134.1.55}}</ref> |
||
Type-I [[cystic adenomatoid malformation]] (CAM) has recently been identified as a precursor lesion for the development of mucinous BAC, but these cases are rare.<ref name='ScialpiCappabianca'>Scialpi M, Cappabianca S, Rotondo A, Scalera GB, Barberini F, Cagini L, Donato S, Brunese L, Piscioli I, Lupattelli L. Pulmonary congenital cystic disease in adults. Spiral computed tomography findings with pathologic correlation and management. ''Radiol Med'' 2010 Jan 7. [abstract] [Epub ahead of print]</ref><ref name='AbecasisGomes'>Abecasis F, Gomes Ferreira M, Oliveira A, Vaz Velho H |
Type-I [[cystic adenomatoid malformation]] (CAM) has recently been identified as a precursor lesion for the development of mucinous BAC, but these cases are rare.<ref name='ScialpiCappabianca'>Scialpi M, Cappabianca S, Rotondo A, Scalera GB, Barberini F, Cagini L, Donato S, Brunese L, Piscioli I, Lupattelli L. Pulmonary congenital cystic disease in adults. Spiral computed tomography findings with pathologic correlation and management. ''Radiol Med'' 2010 Jan 7. [abstract] [Epub ahead of print]</ref><ref name='AbecasisGomes'>{{cite journal |author=Abecasis F, Gomes Ferreira M, Oliveira A, Vaz Velho H |title=[Bronchioloalveolar carcinoma associated with congenital pulmonary airway malformation in an asymptomatic adolescent] |language=Portuguese |journal=Rev Port Pneumol |volume=14 |issue=2 |pages=285–90 |year=2008 |pmid=18363023 }}</ref> |
||
Rarely, BAC may develop a rhabdoid morphology due to the development of dense perinuclear inclusions.<ref name='SongJang'>Song DE, Jang SJ, Black J, Ro JY |
Rarely, BAC may develop a rhabdoid morphology due to the development of dense perinuclear inclusions.<ref name='SongJang'>{{cite journal |author=Song DE, Jang SJ, Black J, Ro JY |title=Mucinous bronchioloalveolar carcinoma of lung with a rhabdoid component—report of a case and review of the literature |journal=Histopathology |volume=51 |issue=3 |pages=427–30 |year=2007 |month=September |pmid=17727492 |doi=10.1111/j.1365-2559.2007.02784.x |url=http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0309-0167&date=2007&volume=51&issue=3&spage=427}}</ref> |
||
==Treatment== |
==Treatment== |
||
| Line 66: | Line 66: | ||
The treatment of choice in any patient with BAC is complete surgical resection, typically via [[lobectomy]] or [[pneumonectomy]], with concurrent ipsilateral lymphadenectomy.<ref name="RazHe"/> |
The treatment of choice in any patient with BAC is complete surgical resection, typically via [[lobectomy]] or [[pneumonectomy]], with concurrent ipsilateral lymphadenectomy.<ref name="RazHe"/> |
||
Non-mucinous BACs are highly associated with classical EGFR mutations, and thus are often responsive to targeted chemotherapy with erlotinib and gefinitib. K-ras mutations are rare in nm-BAC.<ref name='FinbergSequist'>Finberg KE, Sequist LV, Joshi VA, |
Non-mucinous BACs are highly associated with classical EGFR mutations, and thus are often responsive to targeted chemotherapy with erlotinib and gefinitib. K-ras mutations are rare in nm-BAC.<ref name='FinbergSequist'>{{cite journal |author=Finberg KE, Sequist LV, Joshi VA, ''et al.'' |title=Mucinous differentiation correlates with absence of EGFR mutation and presence of KRAS mutation in lung adenocarcinomas with bronchioloalveolar features |journal=J Mol Diagn |volume=9 |issue=3 |pages=320–6 |year=2007 |month=July |pmid=17591931 |pmc=1899415 |doi=10.2353/jmoldx.2007.060182 |url=http://linkinghub.elsevier.com/retrieve/pii/S1525-1578(10)60400-X}}</ref> |
||
Mucinous BAC, in contrast, is much more highly associated with K-ras mutations and wild-type EGFR, and are thus usually insensitive to the EGFR tyrosine kinase inhibitors.<ref name='SakumaMatsukuma'>Sakuma Y, Matsukuma S, Yoshihara M, |
Mucinous BAC, in contrast, is much more highly associated with K-ras mutations and wild-type EGFR, and are thus usually insensitive to the EGFR tyrosine kinase inhibitors.<ref name='SakumaMatsukuma'>{{cite journal |author=Sakuma Y, Matsukuma S, Yoshihara M, ''et al.'' |title=Distinctive evaluation of nonmucinous and mucinous subtypes of bronchioloalveolar carcinomas in EGFR and K-ras gene-mutation analyses for Japanese lung adenocarcinomas: confirmation of the correlations with histologic subtypes and gene mutations |journal=Am. J. Clin. Pathol. |volume=128 |issue=1 |pages=100–8 |year=2007 |month=July |pmid=17580276 |doi=10.1309/WVXFGAFLAUX48DU6 |url=http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17580276}}</ref> In fact, there is some evidence suggest that administration of EGFR-pathway inhibitors to patients with K-ras mutated BACs may even be harmful.<ref name='Vincent'/> |
||
==Recurrence== |
==Recurrence== |
||
| Line 76: | Line 76: | ||
==Prognosis and Survival== |
==Prognosis and Survival== |
||
Taken as a class, long-term survival rates in BAC tend to be higher than those of other forms of NSCLC.<ref name='BreathnachKwiatkowski'>Breathnach OS, Kwiatkowski DJ, Finkelstein DM, |
Taken as a class, long-term survival rates in BAC tend to be higher than those of other forms of NSCLC.<ref name='BreathnachKwiatkowski'>{{cite journal |author=Breathnach OS, Kwiatkowski DJ, Finkelstein DM, ''et al.'' |title=Bronchioloalveolar carcinoma of the lung: recurrences and survival in patients with stage I disease |journal=J. Thorac. Cardiovasc. Surg. |volume=121 |issue=1 |pages=42–7 |year=2001 |month=January |pmid=11135158 |doi=10.1067/mtc.2001.110190 |url=http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(01)52573-8}}</ref><ref name='GroverPiantadosi'>{{cite journal |author=Grover FL, Piantadosi S |title=Recurrence and survival following resection of bronchioloalveolar carcinoma of the lung--The Lung Cancer Study Group experience |journal=Ann. Surg. |volume=209 |issue=6 |pages=779–90 |year=1989 |month=June |pmid=2543339 |pmc=1494125 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0003-4932&volume=209&issue=6&spage=779}}</ref> BAC generally carries a better prognosis than other forms of NSCLC, which can be partially attributed to localized presentation of the disease. <ref name='ReadPage'/> Though other factors might play a role. Prognosis of BAC depends upon the histological subtype and extent at presentation but are generally same as other NSCLC.<ref>{{cite journal|last=Barkley|first=JE|coauthors=Green, MR|title=Bronchioloalveolar carcinoma.|journal=Journal of clinical oncology : official journal of the American Society of Clinical Oncology|date=1996 Aug|volume=14|issue=8|pages=2377–86|pmid=8708731}}</ref> |
||
Recent research has made it clear that nonmucinous and mucinous BACs are very different types of lung cancer.<ref name="YoussemBeasley"/><ref name='GarfieldCadranel'>Garfield DH, Cadranel J, West HL |
Recent research has made it clear that nonmucinous and mucinous BACs are very different types of lung cancer.<ref name="YoussemBeasley"/><ref name='GarfieldCadranel'>{{cite journal |author=Garfield DH, Cadranel J, West HL |title=Bronchioloalveolar carcinoma: the case for two diseases |journal=Clin Lung Cancer |volume=9 |issue=1 |pages=24–9 |year=2008 |month=January |pmid=18282354 |doi=10.3816/CLC.2008.n.004 |url=http://linkinghub.elsevier.com/retrieve/pii/S1525-7304(11)70125-5}}</ref> Mucinous BAC is much more likely to present with multiple unilateral tumors and/or in a unilateral or bilateral pneumonic form than nonmucinous BAC.<ref name='YoussemBeasley'/> The overall prognosis for patients with mucinous BAC is significantly worse than patients with nonmucinous BAC.<ref name="ZellOu"/><ref name='FurakTrojan'>{{cite journal |author=Furák J, Troján I, Szoke T, ''et al.'' |title=Bronchioloalveolar lung cancer: occurrence, surgical treatment and survival |journal=Eur J Cardiothorac Surg |volume=23 |issue=5 |pages=818–23 |year=2003 |month=May |pmid=12754039 |url=http://ejcts.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12754039}}</ref> |
||
Although data are scarce, some studies suggest that survival rates are even lower in the mixed mucinous/non-mucinous variant than in the monophasic forms.<ref name="FurakTrojan"/> |
Although data are scarce, some studies suggest that survival rates are even lower in the mixed mucinous/non-mucinous variant than in the monophasic forms.<ref name="FurakTrojan"/> |
||
| Line 104: | Line 104: | ||
[[cs:Bronchioloalveolární karcinom]] |
[[cs:Bronchioloalveolární karcinom]] |
||
[[de:Bronchioloalveoläres Karzinom]] |
[[de:Bronchioloalveoläres Karzinom]] |
||
{{cite journal |author=Scialpi M, Cappabianca S, Rotondo A, ''et al.'' |title=Pulmonary congenital cystic disease in adults. Spiral computed tomography findings with pathologic correlation and management |journal=Radiol Med |volume=115 |issue=4 |pages=539–50 |year=2010 |month=June |pmid=20058095 |doi=10.1007/s11547-010-0467-6 }} |
|||
Revision as of 03:57, 14 April 2012
| Adenocarcinoma in situ of the lung | |
|---|---|
| Specialty | Oncology |
Bronchioloalveolar carcinoma (BAC) is a term describing certain variants of lung cancer arising in the distal bronchioles or alveoli that initially exhibit a specific non-invasive growth pattern.
Classification

Lung cancers are an extremely heterogeneous family of malignant neoplasms,[1] with well over 50 different histological variants recognized under the 2004 revision of the World Health Organization ("WHO-2004") typing system, currently the most widely used lung cancer classification scheme.[2] Because these variants can have widely differing genetic, biological, and clinical properties, including response to treatment, correct classification of lung cancer cases are necessary to assure that lung cancer patients receive optimum management.[3][4]
Approximately 98% of lung cancers are carcinoma, which are tumors composed of cells with epithelial characteristics.[5] 8 major groups of lung carcinomas are recognized in WHO-2004:[2]
- Squamous Cell Carcinoma
- Small Cell Carcinoma
- Adenocarcinoma
- Large Cell Carcinoma
- Adenosquamous Carcinoma
- Sarcomatoid Carcinoma
- Carcinoid Tumor
- Salivary Gland-like Carcinoma
In WHO-2004, BACs are one of four specific histologic subtypes of lung adenocarcinoma, along with acinar adenocarcinoma, papillary adenocarcinoma, and solid adenocarcinoma with mucin production. However, approximately 80% of adenocarcinomas are found to contain two (or more) of these four subtypes. Multiphasic tumors such as these are classified into a fifth "subtype", termed adenocarcinoma with mixed subtypes.[2]
There are other classification systems that have been proposed for lung cancers, including BACs and other forms of adenocarcinoma. The Noguchi classification system for small adenocarcinomas has received considerable attention, particularly in Japan, but has not been nearly as widely applied and recognized as the WHO system.[6]
Like other forms of lung carcinoma, BAC possesses unique clinical and pathological features, prognosis, and responses to different treatments.[7]
Diagnosis
The criteria for diagnosing BACs have changed since 1999.[8][9] Under the new definition, BAC is defined as a tumor that grows in a lepidic (that is, a scaly covering) fashion along pre-existing airway structures, without detectable invasion or destruction of the underlying tissue, blood vessels, or lymphatics.[10] Because invasion must be ruled out, BAC can be diagnosed only after complete sectioning and examination of the entire tumor, not using biopsy or cytology samples. BAC is considered a pre-invasive malignant lesion that, after further mutation and progression, eventually generates an invasive adenocarcinoma. Therefore, it is considered a form of carcinoma in situ (CIS).
Epidemiology
BAC is the only lung cancer, besides Carcinoid, not associated with smoking,(more common in non-smokers, women and Asians).[11] The criteria for diagnosing BAC have changed since 1999.[10] Under the new definition, BAC is not considered to be an invasive tumor by pathologists, but as one form of carcinoma in situ (CIS). Like other forms of CIS, BAC may progress and become overtly invasive, exhibiting malignant, often lethal, behavior. Major surgery, either a lobectomy or a pneumonectomy, is usually needed to control it, and like other forms of non-small cell lung carcinoma, recurrences are frequent. Therefore, oncologists classify it among the other malignant tumors, which are invasive tumors.[2]
Under the new, more restrictive WHO criteria for lung cancer classification, BAC is now diagnosed much less frequently than it was in the past.[2] Recent studies suggest that BAC comprises between 3% and 5% of all lung carcinomas in the U.S.[12][13]
Variants of BAC
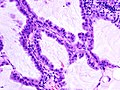
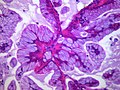
BAC occurs in two major histopathological variants, mucinous BAC (m-BAC, 20%-25% of cases)[14][15] and non mucinous BAC (nm-BAC, 75%-80% of cases).[15][16] Very rarely, BAC can also occur as a "mixed mucinous and non-mucinous" (or "indeterminant") variant.[2]
Incidence
The incidence of bronchiolo-alveolar carcinoma has been reported to vary from 4–24% of all lung cancer patietnts.[13] An analysis of Surveillance epidemiology and End results registry ( SEER) by Read et al. revealed that although the incidence of BAC has increased over the past two decade it still constitutes less than 4% of NSCLC in every time interval.[13] This difference in the incidence has been attributed to complex histopathology of cancer. While pure BAC is rare, the increase in incidence as seen in various studies can be due to unclear histological classification till WHO came up with its classification in 1999 and then in 20044. Another distinguishing feature about BAC is that it afflicts men and women in equal proportions, some recent studies even suggest slightly higher incidence among women. [12][13]
Histogenesis
Nonmucinous BAC is thought to derive from a transformed cell in the distal airways and terminal respiratory units, and often shows features of Clara cell or Type II pneumocyte differentiation.[14] Mucinous BAC, in contrast, probably derives from a transformed glandular cell in distal bronchioles.[17]
Type-I cystic adenomatoid malformation (CAM) has recently been identified as a precursor lesion for the development of mucinous BAC, but these cases are rare.[18][19]
Rarely, BAC may develop a rhabdoid morphology due to the development of dense perinuclear inclusions.[20]
Treatment
The treatment of choice in any patient with BAC is complete surgical resection, typically via lobectomy or pneumonectomy, with concurrent ipsilateral lymphadenectomy.[15]
Non-mucinous BACs are highly associated with classical EGFR mutations, and thus are often responsive to targeted chemotherapy with erlotinib and gefinitib. K-ras mutations are rare in nm-BAC.[21]
Mucinous BAC, in contrast, is much more highly associated with K-ras mutations and wild-type EGFR, and are thus usually insensitive to the EGFR tyrosine kinase inhibitors.[22] In fact, there is some evidence suggest that administration of EGFR-pathway inhibitors to patients with K-ras mutated BACs may even be harmful.[4]
Recurrence
When BAC recurs after surgery, the recurrences are local in about three-quarters of cases, a rate higher than other forms of NSCLC, which tends to recur distantly.[15]
Prognosis and Survival
Taken as a class, long-term survival rates in BAC tend to be higher than those of other forms of NSCLC.[23][24] BAC generally carries a better prognosis than other forms of NSCLC, which can be partially attributed to localized presentation of the disease. [13] Though other factors might play a role. Prognosis of BAC depends upon the histological subtype and extent at presentation but are generally same as other NSCLC.[25]
Recent research has made it clear that nonmucinous and mucinous BACs are very different types of lung cancer.[14][26] Mucinous BAC is much more likely to present with multiple unilateral tumors and/or in a unilateral or bilateral pneumonic form than nonmucinous BAC.[14] The overall prognosis for patients with mucinous BAC is significantly worse than patients with nonmucinous BAC.[12][27]
Although data are scarce, some studies suggest that survival rates are even lower in the mixed mucinous/non-mucinous variant than in the monophasic forms.[27]
In non-mucinous BAC, neither Clara cell nor Type II pneumocyte differentiation appears to affect survival or prognosis.[14]
Additional images
Mucinous BAC
References
- ^ Roggli VL, Vollmer RT, Greenberg SD, McGavran MH, Spjut HJ, Yesner R (1985). "Lung cancer heterogeneity: a blinded and randomized study of 100 consecutive cases". Hum. Pathol. 16 (6): 569–79. PMID 2987102.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e f Travis, William D; Brambilla, Elisabeth; Muller-Hermelink, H Konrad; Harris, Curtis C, eds. (2004). Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (PDF). World Health Organization Classification of Tumours. Lyon: IARC Press. ISBN 92 832 2418 3. Retrieved 27 March 2010. Cite error: The named reference "who2004" was defined multiple times with different content (see the help page).
- ^ Rossi G, Marchioni A, Sartori1 G, Longo L, Piccinini S, Cavazza A (2007). "Histotype in non-small cell lung cancer therapy and staging: The emerging role of an old and underrated factor". Curr Resp Med Rev. 3: 69–77. doi:10.2174/157339807779941820.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ a b Vincent MD (2009). "Optimizing the management of advanced non-small-cell lung cancer: a personal view". Curr Oncol. 16 (4): 9–21. PMC 2722061. PMID 19672420.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Travis WD, Travis LB, Devesa SS (1995). "Lung cancer". Cancer. 75 (1 Suppl): 191–202. PMID 8000996.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Noguchi M, Morikawa A, Kawasaki M; et al. (1995). "Small adenocarcinoma of the lung. Histologic characteristics and prognosis". Cancer. 75 (12): 2844–52. PMID 7773933.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Varlotto JM, Flickinger JC, Recht A, Nikolov MC, DeCamp MM. Comparison of survival and disease-specific survival in surgically resected, lymph node-positive bronchioloalveolar carcinoma versus nonsmall cell lung cancer. Cancer 2008; 112:1547-54.
- ^ World Health Organization. Histological Typing of Lung Tumours. 1st ed. Geneva, Switzerland: World Health Organization; 1967.
- ^ World Health Organization. Histological Typing of Lung Tumours. 2nd ed. Geneva, Switzerland: World Health Organization; 1981.
- ^ a b Travis WD,Colby TV,Corrin B, et al. Histological Typing of Lung and Pleural Tumors, 3rd ed. Berlin: Springer; 1999.
- ^ Raz DJ, He B, Rosell R, Jablons DM (2006). "Bronchioloalveolar carcinoma: a review". Clin Lung Cancer. 7 (5): 313–22. doi:10.3816/CLC.2006.n.012. PMID 16640802.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Zell JA, Ou SH, Ziogas A, Anton-Culver H (2005). "Epidemiology of bronchioloalveolar carcinoma: improvement in survival after release of the 1999 WHO classification of lung tumors". J. Clin. Oncol. 23 (33): 8396–405. doi:10.1200/JCO.2005.03.0312. PMID 16293870.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e Read WL, Page NC, Tierney RM, Piccirillo JF, Govindan R (2004). "The epidemiology of bronchioloalveolar carcinoma over the past two decades: analysis of the SEER database". Lung Cancer. 45 (2): 137–42. doi:10.1016/j.lungcan.2004.01.019. PMID 15246183.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) Cite error: The named reference "ReadPage" was defined multiple times with different content (see the help page). - ^ a b c d e Yousem SA, Beasley MB (2007). "Bronchioloalveolar carcinoma: a review of current concepts and evolving issues". Arch. Pathol. Lab. Med. 131 (7): 1027–32. doi:10.1043/1543-2165(2007)131[1027:BCAROC]2.0.CO;2. PMID 17616987.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Raz DJ, He B, Rosell R, Jablons DM (2006). "Current concepts in bronchioloalveolar carcinoma biology". Clin. Cancer Res. 12 (12): 3698–704. doi:10.1158/1078-0432.CCR-06-0457. PMID 16778095.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL (1 November 1997). "Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings". Radiographics. 17 (6): 1345–57. PMID 9397450.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chilosi M, Murer B (2010). "Mixed adenocarcinomas of the lung: place in new proposals in classification, mandatory for target therapy". Arch. Pathol. Lab. Med. 134 (1): 55–65. doi:10.1043/1543-2165-134.1.55. PMID 20073606.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Scialpi M, Cappabianca S, Rotondo A, Scalera GB, Barberini F, Cagini L, Donato S, Brunese L, Piscioli I, Lupattelli L. Pulmonary congenital cystic disease in adults. Spiral computed tomography findings with pathologic correlation and management. Radiol Med 2010 Jan 7. [abstract] [Epub ahead of print]
- ^ Abecasis F, Gomes Ferreira M, Oliveira A, Vaz Velho H (2008). "[Bronchioloalveolar carcinoma associated with congenital pulmonary airway malformation in an asymptomatic adolescent]". Rev Port Pneumol (in Portuguese). 14 (2): 285–90. PMID 18363023.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Song DE, Jang SJ, Black J, Ro JY (2007). "Mucinous bronchioloalveolar carcinoma of lung with a rhabdoid component—report of a case and review of the literature". Histopathology. 51 (3): 427–30. doi:10.1111/j.1365-2559.2007.02784.x. PMID 17727492.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Finberg KE, Sequist LV, Joshi VA; et al. (2007). "Mucinous differentiation correlates with absence of EGFR mutation and presence of KRAS mutation in lung adenocarcinomas with bronchioloalveolar features". J Mol Diagn. 9 (3): 320–6. doi:10.2353/jmoldx.2007.060182. PMC 1899415. PMID 17591931.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sakuma Y, Matsukuma S, Yoshihara M; et al. (2007). "Distinctive evaluation of nonmucinous and mucinous subtypes of bronchioloalveolar carcinomas in EGFR and K-ras gene-mutation analyses for Japanese lung adenocarcinomas: confirmation of the correlations with histologic subtypes and gene mutations". Am. J. Clin. Pathol. 128 (1): 100–8. doi:10.1309/WVXFGAFLAUX48DU6. PMID 17580276.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Breathnach OS, Kwiatkowski DJ, Finkelstein DM; et al. (2001). "Bronchioloalveolar carcinoma of the lung: recurrences and survival in patients with stage I disease". J. Thorac. Cardiovasc. Surg. 121 (1): 42–7. doi:10.1067/mtc.2001.110190. PMID 11135158.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Grover FL, Piantadosi S (1989). "Recurrence and survival following resection of bronchioloalveolar carcinoma of the lung--The Lung Cancer Study Group experience". Ann. Surg. 209 (6): 779–90. PMC 1494125. PMID 2543339.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Barkley, JE (1996 Aug). "Bronchioloalveolar carcinoma". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 14 (8): 2377–86. PMID 8708731.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Garfield DH, Cadranel J, West HL (2008). "Bronchioloalveolar carcinoma: the case for two diseases". Clin Lung Cancer. 9 (1): 24–9. doi:10.3816/CLC.2008.n.004. PMID 18282354.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Furák J, Troján I, Szoke T; et al. (2003). "Bronchioloalveolar lung cancer: occurrence, surgical treatment and survival". Eur J Cardiothorac Surg. 23 (5): 818–23. PMID 12754039.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Scialpi M, Cappabianca S, Rotondo A; et al. (2010). "Pulmonary congenital cystic disease in adults. Spiral computed tomography findings with pathologic correlation and management". Radiol Med. 115 (4): 539–50. doi:10.1007/s11547-010-0467-6. PMID 20058095. {{cite journal}}: Explicit use of et al. in: |author= (help); Unknown parameter |month= ignored (help)CS1 maint: multiple names: authors list (link)