Pulse oximetry: Difference between revisions
DevRockinAZ (talk | contribs) |
No edit summary |
||
| Line 8: | Line 8: | ||
==History== |
==History== |
||
In 1935, Karl Matthes (German physician 1905–1962) developed the first 2-wavelength ear O<sub>2</sub> saturation meter with red and green filters (later switched to red and infrared filters). His meter was the first device to measure O<sub>2</sub> saturation.<ref>{{cite journal |last=Matthes |first=K |title=Untersuchungen über die Sauerstoffsättigung des menschlichen Arterienblutes |language=German |trans-title=Studies on the Oxygen Saturation of Arterial Human Blood |journal=Naunyn-Schmiedeberg's Archives of Pharmacology |volume=179 |issue=6 |pages=698–711 |doi=10.1007/BF01862691 |
In 1935, Karl Matthes (German physician 1905–1962) developed the first 2-wavelength ear O<sub>2</sub> saturation meter with red and green filters (later switched to red and infrared filters). His meter was the first device to measure O<sub>2</sub> saturation.<ref>{{cite journal |last=Matthes |first=K |title=Untersuchungen über die Sauerstoffsättigung des menschlichen Arterienblutes |language=German |trans-title=Studies on the Oxygen Saturation of Arterial Human Blood |journal=Naunyn-Schmiedeberg's Archives of Pharmacology |volume=179 |issue=6 |pages=698–711 |doi=10.1007/BF01862691 |year=1935}}</ref> |
||
The original oximeter was made by [[Glenn Allan Millikan]] in the 1940s.<ref>{{cite journal |author=Millikan G. A. |authorlink=Glenn Allan Millikan |year=1942 |title=The oximeter: an instrument for measuring continuously oxygen saturation of arterial blood in man |url= |journal=[[Review of Scientific Instruments]] |volume=13 |issue=10 |pages=434–444 |doi=10.1063/1.1769941 |bibcode=1942RScI...13..434M }}</ref> In 1949 Wood added a pressure capsule to squeeze blood out of the ear so as to obtain an absolute O<sub>2</sub> saturation value when blood was readmitted. The concept is similar to today's conventional pulse oximetry, but was difficult to implement because of unstable [[photocell]]s and light sources; the method is not now used clinically. In 1964 Shaw assembled the first absolute reading ear oximeter by using eight wavelengths of light. |
The original oximeter was made by [[Glenn Allan Millikan]] in the 1940s.<ref>{{cite journal |author=Millikan G. A. |authorlink=Glenn Allan Millikan |year=1942 |title=The oximeter: an instrument for measuring continuously oxygen saturation of arterial blood in man |url= |journal=[[Review of Scientific Instruments]] |volume=13 |issue=10 |pages=434–444 |doi=10.1063/1.1769941 |bibcode=1942RScI...13..434M }}</ref> In 1949 Wood added a pressure capsule to squeeze blood out of the ear so as to obtain an absolute O<sub>2</sub> saturation value when blood was readmitted. The concept is similar to today's conventional pulse oximetry, but was difficult to implement because of unstable [[photocell]]s and light sources; the method is not now used clinically. In 1964 Shaw assembled the first absolute reading ear oximeter by using eight wavelengths of light. |
||
Pulse oximetry was developed in 1972, by [[Takuo Aoyagi]] and Michio Kishi, bioengineers, at [[Nihon Kohden]] using the ratio of red to infrared light absorption of pulsating components at the measuring site. Susumu Nakajima, a surgeon, and his associates first tested the device in patients, reporting it in 1975.<ref>{{cite journal|first=John W. |last=Severinghaus |first2=Yoshiyuki |last2=Honda |title=History of Blood Gas Analysis. VII. Pulse Oximetry |url=http://www.masimo.com/Nellcorfiction/PDF_FF/History%20of%20Pulse%20Oximetry.pdf |journal=Journal of Clinical Monitoring |volume=3 |issue=2 |date=April 1987 |pages=135–138 |pmid=3295125 |doi=10.1007/bf00858362 |deadurl=yes |archiveurl=https://web.archive.org/web/20081116151256/http://www.masimo.com/Nellcorfiction/PDF_FF/History%20of%20Pulse%20Oximetry.pdf |archivedate=2008-11-16 |df= }}</ref> It was commercialized by [[Biox]] in 1980. <ref>{{Cite web|url=http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=46970|title=510(k) Premarket Notification|website=www.accessdata.fda.gov|access-date=2017-02-23}}</ref><ref>{{cite journal |
Pulse oximetry was developed in 1972, by [[Takuo Aoyagi]] and Michio Kishi, bioengineers, at [[Nihon Kohden]] using the ratio of red to infrared light absorption of pulsating components at the measuring site. Susumu Nakajima, a surgeon, and his associates first tested the device in patients, reporting it in 1975.<ref>{{cite journal|first=John W. |last=Severinghaus |first2=Yoshiyuki |last2=Honda |title=History of Blood Gas Analysis. VII. Pulse Oximetry |url=http://www.masimo.com/Nellcorfiction/PDF_FF/History%20of%20Pulse%20Oximetry.pdf |journal=Journal of Clinical Monitoring |volume=3 |issue=2 |date=April 1987 |pages=135–138 |pmid=3295125 |doi=10.1007/bf00858362 |deadurl=yes |archiveurl=https://web.archive.org/web/20081116151256/http://www.masimo.com/Nellcorfiction/PDF_FF/History%20of%20Pulse%20Oximetry.pdf |archivedate=2008-11-16 |df= }}</ref> It was commercialized by [[Biox]] in 1980. <ref>{{Cite web|url=http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=46970|title=510(k) Premarket Notification|website=www.accessdata.fda.gov|access-date=2017-02-23}}</ref><ref>{{cite journal |doi=10.1007/bf00858362 }}</ref><ref>http://www.masimo.co.uk/nellcorfiction/index.htm{{full}}</ref> |
||
By 1987, the standard of care for the administration of a general anesthetic in the U.S. included pulse oximetry. From the operating room, the use of pulse oximetry rapidly spread throughout the hospital, first to the [[recovery room]], and then into the various [[intensive care unit]]s. Pulse oximetry was of particular value in the neonatal unit where the patients do not thrive with inadequate oxygenation, but too much oxygen and fluctuations in oxygen concentration can lead to vision impairment or blindness from retinopathy of prematurity (ROP). Furthermore, obtaining an arterial blood gas from a neonatal patient is painful to the patient and a major cause of neonatal anemia.<ref>Lin JC, Strauss RG, Kulhavy JC, et al. Phlebotomy overdraw in the neonatal intensive care nursery. ''Pediatrics'' Aug 2000;106(2):E19.</ref> Motion artifact can be a significant limitation to pulse oximetry monitoring resulting in frequent false alarms and loss of data. The reason for this is that during motion and low peripheral perfusion, many pulse oximeters cannot distinguish between pulsating arterial blood and moving venous blood, leading to underestimation of oxygen saturation. Early studies of pulse oximetry performance during subject motion made clear the vulnerabilities of conventional pulse oximetry technologies to motion artifact.<ref>{{cite journal | author = Barker SJ | year = 2002 | title = "Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = 4| pages = 967–972 | doi=10.1213/00000539-200210000-00033}}</ref><ref>{{cite journal |vauthors=Barker SJ, Shah NK | year = 1997 | title = The effects of motion on the performance of pulse oximeters in volunteers (revised publication) | url = | journal = Anesthesiology | volume = 86 | issue = 1| pages = 101–108 | doi=10.1097/00000542-199701000-00014}}</ref> |
By 1987, the standard of care for the administration of a general anesthetic in the U.S. included pulse oximetry. From the operating room, the use of pulse oximetry rapidly spread throughout the hospital, first to the [[recovery room]], and then into the various [[intensive care unit]]s. Pulse oximetry was of particular value in the neonatal unit where the patients do not thrive with inadequate oxygenation, but too much oxygen and fluctuations in oxygen concentration can lead to vision impairment or blindness from retinopathy of prematurity (ROP). Furthermore, obtaining an arterial blood gas from a neonatal patient is painful to the patient and a major cause of neonatal anemia.<ref>Lin JC, Strauss RG, Kulhavy JC, et al. Phlebotomy overdraw in the neonatal intensive care nursery. ''Pediatrics'' Aug 2000;106(2):E19.</ref> Motion artifact can be a significant limitation to pulse oximetry monitoring resulting in frequent false alarms and loss of data. The reason for this is that during motion and low peripheral perfusion, many pulse oximeters cannot distinguish between pulsating arterial blood and moving venous blood, leading to underestimation of oxygen saturation. Early studies of pulse oximetry performance during subject motion made clear the vulnerabilities of conventional pulse oximetry technologies to motion artifact.<ref>{{cite journal | author = Barker SJ | year = 2002 | title = "Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = 4| pages = 967–972 | doi=10.1213/00000539-200210000-00033}}</ref><ref>{{cite journal |vauthors=Barker SJ, Shah NK | year = 1997 | title = The effects of motion on the performance of pulse oximeters in volunteers (revised publication) | url = | journal = Anesthesiology | volume = 86 | issue = 1| pages = 101–108 | doi=10.1097/00000542-199701000-00014}}</ref> |
||
In 1995, [[Masimo]] introduced Signal Extraction Technology (SET) that could measure accurately during patient motion and low perfusion by separating the arterial signal from the venous and other signals. Since then, pulse oximetry manufacturers have developed new algorithms to reduce some false alarms during motion<ref>{{cite journal |vauthors=Jopling MW, Mannheimer PD, Bebout DE | year = 2002 | title = Issues in the laboratory evaluation of pulse oximeter performance | pmid = 11900041 | journal = Anesth Analg | volume = 94 | issue = | pages = S62–68 }}</ref> such as extending averaging times or freezing values on the screen, but they do not claim to measure changing conditions during motion and low perfusion. So, there are still important differences in performance of pulse oximeters during challenging conditions.<ref>{{cite journal | author = Shah N, Ragaswamy HB, Govindugari K, Estanol L | year = | title = Performance of three new-generation pulse oximeters during motion and low perfusion in volunteers | url = | journal = J Clin Anesth | volume = 24 | issue = | pages = 385–391 | doi = 10.1016/j.jclinane.2011.10.012 }}</ref> |
In 1995, [[Masimo]] introduced Signal Extraction Technology (SET) that could measure accurately during patient motion and low perfusion by separating the arterial signal from the venous and other signals. Since then, pulse oximetry manufacturers have developed new algorithms to reduce some false alarms during motion<ref>{{cite journal |vauthors=Jopling MW, Mannheimer PD, Bebout DE | year = 2002 | title = Issues in the laboratory evaluation of pulse oximeter performance | pmid = 11900041 | journal = Anesth Analg | volume = 94 | issue = | pages = S62–68 }}</ref> such as extending averaging times or freezing values on the screen, but they do not claim to measure changing conditions during motion and low perfusion. So, there are still important differences in performance of pulse oximeters during challenging conditions.<ref>{{cite journal | author = Shah N, Ragaswamy HB, Govindugari K, Estanol L | year = | title = Performance of three new-generation pulse oximeters during motion and low perfusion in volunteers | url = | journal = J Clin Anesth | volume = 24 | issue = | pages = 385–391 | doi = 10.1016/j.jclinane.2011.10.012 }}</ref> |
||
Published papers have compared signal extraction technology to other pulse oximetry technologies and have demonstrated consistently favorable results for signal extraction technology.<ref>{{cite journal |author = Barker SJ | year = 2002 | title = Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = | pages = 967–72 | doi=10.1213/00000539-200210000-00033}}</ref><ref name="Shah"> |
Published papers have compared signal extraction technology to other pulse oximetry technologies and have demonstrated consistently favorable results for signal extraction technology.<ref>{{cite journal |author = Barker SJ | year = 2002 | title = Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = | pages = 967–72 | doi=10.1213/00000539-200210000-00033}}</ref><ref name="Shah">{{cite journal |doi=10.1016/j.jclinane.2011.10.012 }}</ref><ref>{{cite journal |vauthors=Hay WW Jr, Rodden DJ, Collins SM, Melara DL, Hale KA, Fashaw LM | year = 2002 | title = Reliability of conventional and new pulse oximetry in neonatal patients | url = | journal = J Perinatol | volume = 22 | issue = | pages = 360–6 | doi=10.1038/sj.jp.7210740}}</ref> Signal extraction technology pulse oximetry performance has also been shown to translate into helping clinicians improve patient outcomes. In one study, retinopathy of prematurity (eye damage) was reduced by 58% in very low birth weight neonates at a center using signal extraction technology, while there was no decrease in retinopathy of prematurity at another center with the same clinicians using the same protocol but with non-signal extraction technology.<ref>{{cite journal |vauthors=Castillo A, Deulofeut R, Critz A, Sola A | year = 2010 | title = Prevention of retinopathy of prematurity in preterm infants through changes in clinical practice and SpO(2)technology | journal = Acta Paediatr | volume = 100 | issue = | pages = 188–92 | doi=10.1111/j.1651-2227.2010.02001.x | pmid=20825604 | pmc=3040295}}</ref> Other studies have shown that signal extraction technology pulse oximetry results in fewer arterial blood gas measurements, faster oxygen weaning time, lower sensor utilization, and lower length of stay.<ref>{{cite journal |vauthors=Durbin CG, Rostow SK | year = 2002 | title = More reliable oximetry reduces the frequency of arterial blood gas analyses and hastens oxygen weaning after cardiac surgery: A prospective, randomized trial of the clinical impact of a new technology | url = | journal = Crit Care Med | volume = 30 | issue = | pages = 1735–40 | doi=10.1097/00003246-200208000-00010}}</ref> The measure-through motion and low perfusion capabilities it has also allow it to be used in previously unmonitored areas such as the general floor, where false alarms have plagued conventional pulse oximetry. As evidence of this, a landmark study was published in 2010 showing clinicians using signal extraction technology pulse oximetry on the general floor were able to decrease rapid response team activations, ICU transfers, and ICU days.<ref>{{cite journal |vauthors=Taenzer AH, Pyke JB, McGrath SP, Blike GT | year = 2010 | title = The impact of pulse oximetry surveillance on rescue events and intensive care unit transfers a before-and-after concurrence study | url = | journal = Anesthesiology | volume = 112 | issue = | pages = 282–7 | doi=10.1097/aln.0b013e3181ca7a9b | pmid=20098128}}</ref> |
||
In 2011, an expert workgroup recommended newborn screening with pulse oximetry to increase the detection of critical congenital heart disease (CCHD).<ref>{{cite |
In 2011, an expert workgroup recommended newborn screening with pulse oximetry to increase the detection of critical congenital heart disease (CCHD).<ref>{{cite journal |doi=10.1542/peds.2011-1317 }}</ref> The CCHD workgroup cited the results of two large, prospective studies of 59,876 subjects that exclusively used signal extraction technology to increase the identification of CCHD with minimal false positives.<ref>{{cite journal |doi=10.1136/bmj.a3037 }}</ref><ref>{{cite journal |doi=10.1016/S0140-6736(11)60753-8 }}</ref> The CCHD workgroup recommended newborn screening be performed with motion tolerant pulse oximetry that has also been validated in low perfusion conditions. In 2011, the US Secretary of Health and Human Services added pulse oximetry to the recommended uniform screening panel.<ref>{{cite journal|title=Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease. |date=2014-11-12 |pmid=22201143 | doi=10.1542/peds.2011-3211 |volume=129 |author=Mahle WT, Martin GR, Beekman RH 3rd, Morrow WR |journal=Pediatrics |pages=190–2}}</ref> Before the evidence for screening using signal extraction technology, less than 1% of newborns in the United States were screened. Today, [[The Newborn Foundation]] has documented near universal screening in the United States and international screening is rapidly expanding.<ref>{{cite web|url=http://cchdscreeningmap.org/ |title=Newborn CCHD Screening Progress Map | Updated 7/7/2014 |publisher=Cchdscreeningmap.org |date= |accessdate=2015-04-02}}</ref> In 2014, a third large study of 122, 738 newborns that also exclusively used signal extraction technology showed similar, positive results as the first two large studies.<ref>{{cite journal |doi=10.1016/S0140-6736(14)60198-7 }}</ref> |
||
High-resolution pulse oximetry (HRPO) has been developed for in-home sleep apnea screening and testing in patients for whom it is impractical to perform [[polysomnography]].<ref name="sleepreviewmag.com">[http://www.sleepreviewmag.com/issues/articles/2008-04_10.asp ] {{webarchive |url=https://web.archive.org/web/20120210190044/http://www.sleepreviewmag.com/issues/articles/2008-04_10.asp |date=February 10, 2012 }}</ref><ref>[http://www.maxtecinc.com/assets/docs/pulsox/ml187.p300iDataSheet.pdf ] {{webarchive |url=https://web.archive.org/web/20090107051157/http://www.maxtecinc.com/assets/docs/pulsox/ml187.p300iDataSheet.pdf |date=January 7, 2009 }}</ref><ref>{{cite web|url=http://www.anesthesiology.org/pt/re/anes/fulltext.00000542-200809000-00004.htm |title=Home |publisher=Anesthesiology.org |date= |accessdate=2015-04-02}}</ref> It stores and records both [[pulse rate]] and SpO2 in 1 second intervals and has been shown in one study to help to detect sleep disordered breathing in surgical patients.<ref>{{cite journal |vauthors=Chung F, Liao P, Elsaid H, Islam S, Shapiro CM, Sun Y | year = | title = Oxygen desaturation index from nocturnal oximetry: a sensitive and specific tool to detect sleep-disordered breathing in surgical patients | url = | journal = Anesth Analg | volume = 114 | issue = | pages = 993–1000 | doi=10.1213/ane.0b013e318248f4f5}}</ref> |
High-resolution pulse oximetry (HRPO) has been developed for in-home sleep apnea screening and testing in patients for whom it is impractical to perform [[polysomnography]].<ref name="sleepreviewmag.com">[http://www.sleepreviewmag.com/issues/articles/2008-04_10.asp ] {{webarchive |url=https://web.archive.org/web/20120210190044/http://www.sleepreviewmag.com/issues/articles/2008-04_10.asp |date=February 10, 2012 }}</ref><ref>[http://www.maxtecinc.com/assets/docs/pulsox/ml187.p300iDataSheet.pdf ] {{webarchive |url=https://web.archive.org/web/20090107051157/http://www.maxtecinc.com/assets/docs/pulsox/ml187.p300iDataSheet.pdf |date=January 7, 2009 }}</ref><ref>{{cite web|url=http://www.anesthesiology.org/pt/re/anes/fulltext.00000542-200809000-00004.htm |title=Home |publisher=Anesthesiology.org |date= |accessdate=2015-04-02}}</ref> It stores and records both [[pulse rate]] and SpO2 in 1 second intervals and has been shown in one study to help to detect sleep disordered breathing in surgical patients.<ref>{{cite journal |vauthors=Chung F, Liao P, Elsaid H, Islam S, Shapiro CM, Sun Y | year = | title = Oxygen desaturation index from nocturnal oximetry: a sensitive and specific tool to detect sleep-disordered breathing in surgical patients | url = | journal = Anesth Analg | volume = 114 | issue = | pages = 993–1000 | doi=10.1213/ane.0b013e318248f4f5}}</ref> |
||
| Line 25: | Line 26: | ||
In 1995 Masimo introduced perfusion index, quantifying the amplitude of the peripheral [[plethysmograph]] waveform. Perfusion index has been shown to help clinicians predict illness severity and early adverse respiratory outcomes in neonates,<ref>{{cite journal |vauthors=De Felice C, Leoni L, Tommasini E, Tonni G, Toti P, Del Vecchio A, Ladisa G, Latini G | year = 2008 | title = Maternal pulse oximetry perfusion index as a predictor of early adverse respiratory neonatal outcome after elective cesarean delivery | url = | journal = [[Pediatric Critical Care Medicine]] | volume = 9 | issue = | pages = 203–8 | doi=10.1097/pcc.0b013e3181670021}}</ref><ref>{{cite journal |vauthors=De Felice C, Latini G, Vacca P, Kopotic RJ | year = 2002 | title = The pulse oximeter perfusion index as a predictor for high illness severity in neonates | url = | journal = Eur J Pediatr | volume = 161 | issue = | pages = 561–2 | doi=10.1007/s00431-002-1042-5}}</ref><ref>De Felice C, Goldstein MR, Parrini S, Verrotti A, Criscuolo M, Latini G. Early dynamic changes in pulse oximetry signals in preterm newborns with histologic chorioamnionitis. ''[[Pediatric Critical Care Medicine]]'' 2006;7:138–42.</ref> predict low superior vena cava flow in very low birth weight infants,<ref>{{cite journal |vauthors=Takahashi S, Kakiuchi S, Nanba Y, Tsukamoto K, Nakamura T, Ito Y | year = | title = The perfusion index derived from a pulse oximeter for predicting low superior vena cava flow in very low birth weight infants | url = | journal = J Perinatol | volume = 30 | issue = | pages = 265–9 | doi=10.1038/jp.2009.159| pmc = 2834357}}</ref> provide an early indicator of sympathectomy after epidural anesthesia,<ref>{{cite journal |vauthors=Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM | year = 2009 | title = Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia | url = | journal = Acta Anaesthesiol Scand | volume = 53 | issue = | pages = 1018–26 | doi=10.1111/j.1399-6576.2009.01968.x}}</ref> and improve detection of critical congenital heart disease in newborns.<ref>{{cite journal |vauthors=Granelli AW, Ostman-Smith I | year = 2007 | title = Noninvasive peripheral perfusion index as a possible tool for screening for critical left heart obstruction | url = | journal = Acta Paediatr | volume = 96 | issue = | pages = 1455–9 | doi=10.1111/j.1651-2227.2007.00439.x}}</ref> |
In 1995 Masimo introduced perfusion index, quantifying the amplitude of the peripheral [[plethysmograph]] waveform. Perfusion index has been shown to help clinicians predict illness severity and early adverse respiratory outcomes in neonates,<ref>{{cite journal |vauthors=De Felice C, Leoni L, Tommasini E, Tonni G, Toti P, Del Vecchio A, Ladisa G, Latini G | year = 2008 | title = Maternal pulse oximetry perfusion index as a predictor of early adverse respiratory neonatal outcome after elective cesarean delivery | url = | journal = [[Pediatric Critical Care Medicine]] | volume = 9 | issue = | pages = 203–8 | doi=10.1097/pcc.0b013e3181670021}}</ref><ref>{{cite journal |vauthors=De Felice C, Latini G, Vacca P, Kopotic RJ | year = 2002 | title = The pulse oximeter perfusion index as a predictor for high illness severity in neonates | url = | journal = Eur J Pediatr | volume = 161 | issue = | pages = 561–2 | doi=10.1007/s00431-002-1042-5}}</ref><ref>De Felice C, Goldstein MR, Parrini S, Verrotti A, Criscuolo M, Latini G. Early dynamic changes in pulse oximetry signals in preterm newborns with histologic chorioamnionitis. ''[[Pediatric Critical Care Medicine]]'' 2006;7:138–42.</ref> predict low superior vena cava flow in very low birth weight infants,<ref>{{cite journal |vauthors=Takahashi S, Kakiuchi S, Nanba Y, Tsukamoto K, Nakamura T, Ito Y | year = | title = The perfusion index derived from a pulse oximeter for predicting low superior vena cava flow in very low birth weight infants | url = | journal = J Perinatol | volume = 30 | issue = | pages = 265–9 | doi=10.1038/jp.2009.159| pmc = 2834357}}</ref> provide an early indicator of sympathectomy after epidural anesthesia,<ref>{{cite journal |vauthors=Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM | year = 2009 | title = Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia | url = | journal = Acta Anaesthesiol Scand | volume = 53 | issue = | pages = 1018–26 | doi=10.1111/j.1399-6576.2009.01968.x}}</ref> and improve detection of critical congenital heart disease in newborns.<ref>{{cite journal |vauthors=Granelli AW, Ostman-Smith I | year = 2007 | title = Noninvasive peripheral perfusion index as a possible tool for screening for critical left heart obstruction | url = | journal = Acta Paediatr | volume = 96 | issue = | pages = 1455–9 | doi=10.1111/j.1651-2227.2007.00439.x}}</ref> |
||
In 2007, Masimo introduced the first measurement of the pleth variability index (PVI), which multiple clinical studies have shown provides a new method for automatic, noninvasive assessment of a patient's ability to respond to fluid administration.<ref>{{cite journal | |
In 2007, Masimo introduced the first measurement of the pleth variability index (PVI), which multiple clinical studies have shown provides a new method for automatic, noninvasive assessment of a patient's ability to respond to fluid administration.<ref>{{cite journal |doi=10.1097/EJA.0b013e328335fbd1 }}</ref><ref>{{cite journal |vauthors=Cannesson M, Desebbe O, Rosamel P, Delannoy B, Robin J, Bastien O, Lehot JJ | date = Aug 2008 | title = Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theater | url = | journal = Br J Anaesth | volume = 101 | issue = 2| pages = 200–6 | doi=10.1093/bja/aen133}}</ref><ref>Forget P, Lois F, de Kock M. Goal-Directed Fluid Management Based on the Pulse Oximeter-Derived Pleth Variability Index Reduces Lactate Levels and Improves Fluid Management. Anesth Analg 2010.</ref> Appropriate fluid levels are vital to reducing postoperative risks and improving patient outcomes: fluid volumes that are too low (under-hydration) or too high (over-hydration) have been shown to decrease wound healing and increase the risk of infection or cardiac complications.<ref>{{cite journal | author = Ishii M, Ohno K | year = 1977 | title = Comparisons of body fluid volumes, plasma renin activity, hemodynamics and pressor responsiveness between juvenile and aged patients with essential hypertension | url = | journal = Jpn. Circ. J. | volume = 41 | issue = 3| pages = 237–46 | doi = 10.1253/jcj.41.237 | pmid = 870721 | last2 = Ohno }}</ref> Recently, the National Health Service in the United Kingdom and the French Anesthesia and Critical Care Society listed PVI monitoring as part of their suggested strategies for intra-operative fluid management.<ref>{{cite web|url=http://www.ntac.nhs.uk/NewsAndEvents/NewsEvents3420.aspx |title=[ARCHIVED CONTENT] NHS Technology Adoption Centre |publisher=Ntac.nhs.uk |date= |accessdate=2015-04-02}}</ref><ref>[http://www.aidara.fr/docs/confconsensus/RFEremplissage-SFAR2012.pdf ] {{webarchive |url=https://web.archive.org/web/20141012112938/http://www.aidara.fr/docs/confconsensus/RFEremplissage-SFAR2012.pdf |date=October 12, 2014 }}</ref> |
||
==Function== |
==Function== |
||
| Line 45: | Line 46: | ||
==Indication== |
==Indication== |
||
[[File:Saturometre 2.jpg|thumb|A pulse oximeter probe applied to a person's finger]] |
[[File:Saturometre 2.jpg|thumb|A pulse oximeter probe applied to a person's finger]] |
||
A pulse oximeter is a [[medical device]] that indirectly monitors the oxygen saturation of a patient's [[blood]] (as opposed to measuring oxygen saturation directly through a blood sample) and changes in blood volume in the skin, producing a [[photoplethysmogram]]. The pulse oximeter may be incorporated into a multiparameter patient monitor. Most monitors also display the pulse rate. Portable, battery-operated pulse oximeters are also available for transport or home blood-oxygen monitoring. |
A pulse oximeter is a [[medical device]] that indirectly monitors the oxygen saturation of a patient's [[blood]] (as opposed to measuring oxygen saturation directly through a blood sample) and changes in blood volume in the skin, producing a [[photoplethysmogram]]. The pulse oximeter may be incorporated into a multiparameter patient monitor. Most monitors also display the pulse rate. Portable, battery-operated pulse oximeters are also available for transport or home blood-oxygen monitoring.{{fact}} |
||
===Advantages=== |
===Advantages=== |
||
Pulse oximetry is particularly convenient for [[noninvasive]] continuous measurement of blood oxygen saturation. In contrast, blood gas levels must otherwise be determined in a laboratory on a drawn blood sample. Pulse oximetry is useful in any setting where a patient's [[Oxygenation (medical)|oxygenation]] is unstable, including [[intensive care]], operating, recovery, emergency and hospital ward settings, [[aircraft pilot|pilots]] in unpressurized aircraft, for assessment of any patient's oxygenation, and determining the effectiveness of or need for supplemental [[oxygen]]. Although a pulse oximeter is used to monitor oxygenation, it cannot determine the metabolism of oxygen, or the amount of oxygen being used by a patient. For this purpose, it is necessary to also measure [[carbon dioxide]] (CO<sub>2</sub>) levels. It is possible that it can also be used to detect abnormalities in ventilation. However, the use of a pulse oximeter to detect [[hypoventilation]] is impaired with the use of supplemental oxygen, as it is only when patients breathe room air that abnormalities in respiratory function can be detected reliably with its use. Therefore, the routine administration of supplemental oxygen may be unwarranted if the patient is able to maintain adequate oxygenation in room air, since it can result in hypoventilation going undetected.<ref> |
Pulse oximetry is particularly convenient for [[noninvasive]] continuous measurement of blood oxygen saturation. In contrast, blood gas levels must otherwise be determined in a laboratory on a drawn blood sample. Pulse oximetry is useful in any setting where a patient's [[Oxygenation (medical)|oxygenation]] is unstable, including [[intensive care]], operating, recovery, emergency and hospital ward settings, [[aircraft pilot|pilots]] in unpressurized aircraft, for assessment of any patient's oxygenation, and determining the effectiveness of or need for supplemental [[oxygen]]. Although a pulse oximeter is used to monitor oxygenation, it cannot determine the metabolism of oxygen, or the amount of oxygen being used by a patient. For this purpose, it is necessary to also measure [[carbon dioxide]] (CO<sub>2</sub>) levels. It is possible that it can also be used to detect abnormalities in ventilation. However, the use of a pulse oximeter to detect [[hypoventilation]] is impaired with the use of supplemental oxygen, as it is only when patients breathe room air that abnormalities in respiratory function can be detected reliably with its use. Therefore, the routine administration of supplemental oxygen may be unwarranted if the patient is able to maintain adequate oxygenation in room air, since it can result in hypoventilation going undetected.<ref>{{cite journal |doi=10.1378/chest.126.5.1552 }}</ref> |
||
Because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation values, pulse oximeters are of critical importance in [[emergency medicine]] and are also very useful for patients with respiratory or cardiac problems, especially [[Chronic obstructive pulmonary disease|COPD]], or for diagnosis of some [[sleep disorders]] such as [[apnea]] and [[hypopnea]].<ref>{{cite journal |
Because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation values, pulse oximeters are of critical importance in [[emergency medicine]] and are also very useful for patients with respiratory or cardiac problems, especially [[Chronic obstructive pulmonary disease|COPD]], or for diagnosis of some [[sleep disorders]] such as [[apnea]] and [[hypopnea]].<ref>{{cite journal |title=Sleep 3: Clinical presentation and diagnosis of the obstructive sleep apnoea hypopnoea syndrome |first1=D |last1=Schlosshan |first2=M W |last2=Elliott |volume=59 |pages=347–352 |journal=Thorax |date=2004 |doi=10.1136/thx.2003.007179|pmc=1763828 }}</ref> Portable battery-operated pulse oximeters are useful for pilots operating in a non-pressurized aircraft above 10,000 feet (12,500 feet in the U.S.)<ref>{{cite web|url=http://www.airweb.faa.gov/Regulatory_and_Guidance_Library/rgFAR.nsf/0/BA9AFBF96DBC56F0852566CF006798F9?OpenDocument&Highlight=oxygen |title=FAR Part 91 Sec. 91.211 effective as of 09/30/1963 |publisher=Airweb.faa.gov |date= |accessdate=2015-04-02}}</ref> where supplemental oxygen is required. Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at high [[altitudes]] or with exercise. Some portable pulse oximeters employ software that charts a patient's blood oxygen and pulse, serving as a reminder to check blood oxygen levels. |
||
===Limitations=== |
===Limitations=== |
||
Pulse oximetry measures solely hemoglobin saturation, not [[Ventilation (physiology)|ventilation]] and is not a complete measure of respiratory sufficiency. It is not a substitute for [[blood gases]] checked in a laboratory, because it gives no indication of base deficit, carbon dioxide levels, blood [[pH]], or [[bicarbonate]] (HCO<sub>3</sub><sup>−</sup>) concentration. The metabolism of oxygen can be readily measured by monitoring expired CO<sub>2</sub>, but saturation figures give no information about blood oxygen content. Most of the oxygen in the blood is carried by hemoglobin; in severe anemia, the blood will carry less total oxygen, despite the hemoglobin being 100% saturated. |
Pulse oximetry measures solely hemoglobin saturation, not [[Ventilation (physiology)|ventilation]] and is not a complete measure of respiratory sufficiency. It is not a substitute for [[blood gases]] checked in a laboratory, because it gives no indication of base deficit, carbon dioxide levels, blood [[pH]], or [[bicarbonate]] (HCO<sub>3</sub><sup>−</sup>) concentration. The metabolism of oxygen can be readily measured by monitoring expired CO<sub>2</sub>, but saturation figures give no information about blood oxygen content. Most of the oxygen in the blood is carried by hemoglobin; in severe anemia, the blood will carry less total oxygen, despite the hemoglobin being 100% saturated.{{fact}} |
||
Erroneously low readings may be caused by [[hypoperfusion]] of the extremity being used for monitoring (often due to a limb being cold, or from [[vasoconstriction]] secondary to the use of [[vasopressor]] agents); incorrect sensor application; highly [[Callus|calloused]] skin; or movement (such as shivering), especially during hypoperfusion. To ensure accuracy, the sensor should return a steady pulse and/or pulse waveform. Pulse oximetry technologies differ in their abilities to provide accurate data during conditions of motion and low perfusion.<ref name="Shah" /><ref>{{cite journal | author = Barker SJ | year = 2002 | title = "Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = | pages = 967–72 | doi=10.1213/00000539-200210000-00033}}</ref> |
Erroneously low readings may be caused by [[hypoperfusion]] of the extremity being used for monitoring (often due to a limb being cold, or from [[vasoconstriction]] secondary to the use of [[vasopressor]] agents); incorrect sensor application; highly [[Callus|calloused]] skin; or movement (such as shivering), especially during hypoperfusion. To ensure accuracy, the sensor should return a steady pulse and/or pulse waveform. Pulse oximetry technologies differ in their abilities to provide accurate data during conditions of motion and low perfusion.<ref name="Shah" /><ref>{{cite journal | author = Barker SJ | year = 2002 | title = "Motion-resistant" pulse oximetry: a comparison of new and old models | url = | journal = Anesth Analg | volume = 95 | issue = | pages = 967–72 | doi=10.1213/00000539-200210000-00033}}</ref> |
||
Pulse oximetry also is not a complete measure of circulatory sufficiency. If there is insufficient [[Circulatory system|bloodflow]] or insufficient hemoglobin in the blood ([[anemia]]), tissues can suffer [[Hypoxia (medical)|hypoxia]] despite high [[oxygen saturation]] in the blood that does arrive. In 2008, a pulse oximeter that can measure hemoglobin levels in addition to oxygen saturation was introduced by Masimo. To quantify hemoglobin, the device uses additional wavelengths of light beyond the two standard ones. |
Pulse oximetry also is not a complete measure of circulatory sufficiency. If there is insufficient [[Circulatory system|bloodflow]] or insufficient hemoglobin in the blood ([[anemia]]), tissues can suffer [[Hypoxia (medical)|hypoxia]] despite high [[oxygen saturation]] in the blood that does arrive. In 2008, a pulse oximeter that can measure hemoglobin levels in addition to oxygen saturation was introduced by Masimo. To quantify hemoglobin, the device uses additional wavelengths of light beyond the two standard ones.{{fact}} |
||
Since pulse oximetry measures only the percentage of bound hemoglobin, a falsely high or falsely low reading will occur when hemoglobin binds to something other than oxygen: |
Since pulse oximetry measures only the percentage of bound hemoglobin, a falsely high or falsely low reading will occur when hemoglobin binds to something other than oxygen: |
||
| Line 63: | Line 64: | ||
* [[Cyanide poisoning]] gives a high reading because it reduces oxygen extraction from arterial blood. In this case, the reading is not false, as arterial blood oxygen is indeed high in early cyanide poisoning. |
* [[Cyanide poisoning]] gives a high reading because it reduces oxygen extraction from arterial blood. In this case, the reading is not false, as arterial blood oxygen is indeed high in early cyanide poisoning. |
||
* [[Methemoglobinemia]] characteristically causes pulse oximetry readings in the mid-80s. |
* [[Methemoglobinemia]] characteristically causes pulse oximetry readings in the mid-80s. |
||
* COPD [especially chronic bronchitis] may cause false readings.<ref>{{ |
* COPD [especially chronic bronchitis] may cause false readings.<ref name=pmid26715772>{{cite journal |doi=10.4187/respcare.04435 }}</ref> |
||
A noninvasive method that allows continuous measurement of the dyshemoglobins is the pulse [[CO-oximeter]], which was invented in 2005 by Masimo. It provides clinicians a way to measure the dyshemoglobins, carboxyhemoglobin, and methemoglobin along with total hemoglobin. |
A noninvasive method that allows continuous measurement of the dyshemoglobins is the pulse [[CO-oximeter]], which was invented in 2005 by Masimo. It provides clinicians a way to measure the dyshemoglobins, carboxyhemoglobin, and methemoglobin along with total hemoglobin. |
||
| Line 76: | Line 77: | ||
| date = December 2008}}</ref> |
| date = December 2008}}</ref> |
||
The [[Apple Watch]] uses this technology for its heart rate monitor.<ref>http://9to5mac.com/2015/04/24/apple-watch-blood-oxygen/</ref><ref>https://support.apple.com/en-us/HT204666</ref> The accuracy of the heart rate monitor has been debated, as different tests have shown it to be 91% as accurate as chest strap monitors. <ref>https://www.npr.org/sections/health-shots/2016/10/15/497828894/you-can-monitor-your-heart-with-a-smartphone-but-should-you</ref> |
The [[Apple Watch]] uses this technology for its heart rate monitor.<ref>http://9to5mac.com/2015/04/24/apple-watch-blood-oxygen/</ref><ref>https://support.apple.com/en-us/HT204666{{full}}</ref> The accuracy of the heart rate monitor has been debated, as different tests have shown it to be 91% as accurate as chest strap monitors. <ref>https://www.npr.org/sections/health-shots/2016/10/15/497828894/you-can-monitor-your-heart-with-a-smartphone-but-should-you{{full}}</ref><ref>https://breakingmuscle.com/fitness/chest-strap-vs-wristband-heart-rate-monitors{{full}}</ref> |
||
==Pleth variability index== |
==Pleth variability index== |
||
Pleth variability index (PVI) is a measure of the variability of the plethysmographic waveform amplitude.<ref name="CannessonDesebbe2008">{{cite journal |
Pleth variability index (PVI) is a measure of the variability of the plethysmographic waveform amplitude.<ref name="CannessonDesebbe2008">{{cite journal |doi=10.1093/bja/aen133 }}</ref> |
||
==See also== |
==See also== |
||
Revision as of 22:44, 18 June 2018

Pulse oximetry is a noninvasive method for monitoring a person's oxygen saturation (SO2). Though its reading of SpO2 (peripheral oxygen saturation) is not always identical to the more desirable reading of SaO2 (arterial oxygen saturation) from arterial blood gas analysis, the two are correlated well enough that the safe, convenient, noninvasive, inexpensive pulse oximetry method is valuable for measuring oxygen saturation in clinical use.
In its most common (transmissive) application mode, a sensor device is placed on a thin part of the patient's body, usually a fingertip or earlobe, or in the case of an infant, across a foot. The device passes two wavelengths of light through the body part to a photodetector. It measures the changing absorbance at each of the wavelengths, allowing it to determine the absorbances due to the pulsing arterial blood alone, excluding venous blood, skin, bone, muscle, fat, and (in most cases) nail polish.[1]
Less commonly, reflectance pulse oximetry is used as an alternative to transmissive pulse oximetery described above. This method does not require a thin section of the person's body and is therefore well suited to a universal application such as the feet, forehead, and chest, but it also has some limitations. Vasodilation and pooling of venous blood in the head due to compromised venous return to the heart can cause a combination of arterial and venous pulsations in the forehead region and lead to spurious SpO2 results. Such conditions occur while undergoing anesthesia with endotracheal intubation and mechanical ventilation or in patients in the Trendelenburg position.[2]
History
In 1935, Karl Matthes (German physician 1905–1962) developed the first 2-wavelength ear O2 saturation meter with red and green filters (later switched to red and infrared filters). His meter was the first device to measure O2 saturation.[3]
The original oximeter was made by Glenn Allan Millikan in the 1940s.[4] In 1949 Wood added a pressure capsule to squeeze blood out of the ear so as to obtain an absolute O2 saturation value when blood was readmitted. The concept is similar to today's conventional pulse oximetry, but was difficult to implement because of unstable photocells and light sources; the method is not now used clinically. In 1964 Shaw assembled the first absolute reading ear oximeter by using eight wavelengths of light.
Pulse oximetry was developed in 1972, by Takuo Aoyagi and Michio Kishi, bioengineers, at Nihon Kohden using the ratio of red to infrared light absorption of pulsating components at the measuring site. Susumu Nakajima, a surgeon, and his associates first tested the device in patients, reporting it in 1975.[5] It was commercialized by Biox in 1980. [6][7][8]
By 1987, the standard of care for the administration of a general anesthetic in the U.S. included pulse oximetry. From the operating room, the use of pulse oximetry rapidly spread throughout the hospital, first to the recovery room, and then into the various intensive care units. Pulse oximetry was of particular value in the neonatal unit where the patients do not thrive with inadequate oxygenation, but too much oxygen and fluctuations in oxygen concentration can lead to vision impairment or blindness from retinopathy of prematurity (ROP). Furthermore, obtaining an arterial blood gas from a neonatal patient is painful to the patient and a major cause of neonatal anemia.[9] Motion artifact can be a significant limitation to pulse oximetry monitoring resulting in frequent false alarms and loss of data. The reason for this is that during motion and low peripheral perfusion, many pulse oximeters cannot distinguish between pulsating arterial blood and moving venous blood, leading to underestimation of oxygen saturation. Early studies of pulse oximetry performance during subject motion made clear the vulnerabilities of conventional pulse oximetry technologies to motion artifact.[10][11]
In 1995, Masimo introduced Signal Extraction Technology (SET) that could measure accurately during patient motion and low perfusion by separating the arterial signal from the venous and other signals. Since then, pulse oximetry manufacturers have developed new algorithms to reduce some false alarms during motion[12] such as extending averaging times or freezing values on the screen, but they do not claim to measure changing conditions during motion and low perfusion. So, there are still important differences in performance of pulse oximeters during challenging conditions.[13]
Published papers have compared signal extraction technology to other pulse oximetry technologies and have demonstrated consistently favorable results for signal extraction technology.[14][15][16] Signal extraction technology pulse oximetry performance has also been shown to translate into helping clinicians improve patient outcomes. In one study, retinopathy of prematurity (eye damage) was reduced by 58% in very low birth weight neonates at a center using signal extraction technology, while there was no decrease in retinopathy of prematurity at another center with the same clinicians using the same protocol but with non-signal extraction technology.[17] Other studies have shown that signal extraction technology pulse oximetry results in fewer arterial blood gas measurements, faster oxygen weaning time, lower sensor utilization, and lower length of stay.[18] The measure-through motion and low perfusion capabilities it has also allow it to be used in previously unmonitored areas such as the general floor, where false alarms have plagued conventional pulse oximetry. As evidence of this, a landmark study was published in 2010 showing clinicians using signal extraction technology pulse oximetry on the general floor were able to decrease rapid response team activations, ICU transfers, and ICU days.[19]
In 2011, an expert workgroup recommended newborn screening with pulse oximetry to increase the detection of critical congenital heart disease (CCHD).[20] The CCHD workgroup cited the results of two large, prospective studies of 59,876 subjects that exclusively used signal extraction technology to increase the identification of CCHD with minimal false positives.[21][22] The CCHD workgroup recommended newborn screening be performed with motion tolerant pulse oximetry that has also been validated in low perfusion conditions. In 2011, the US Secretary of Health and Human Services added pulse oximetry to the recommended uniform screening panel.[23] Before the evidence for screening using signal extraction technology, less than 1% of newborns in the United States were screened. Today, The Newborn Foundation has documented near universal screening in the United States and international screening is rapidly expanding.[24] In 2014, a third large study of 122, 738 newborns that also exclusively used signal extraction technology showed similar, positive results as the first two large studies.[25]
High-resolution pulse oximetry (HRPO) has been developed for in-home sleep apnea screening and testing in patients for whom it is impractical to perform polysomnography.[26][27][28] It stores and records both pulse rate and SpO2 in 1 second intervals and has been shown in one study to help to detect sleep disordered breathing in surgical patients.[29]
In 1995 Masimo introduced perfusion index, quantifying the amplitude of the peripheral plethysmograph waveform. Perfusion index has been shown to help clinicians predict illness severity and early adverse respiratory outcomes in neonates,[30][31][32] predict low superior vena cava flow in very low birth weight infants,[33] provide an early indicator of sympathectomy after epidural anesthesia,[34] and improve detection of critical congenital heart disease in newborns.[35]
In 2007, Masimo introduced the first measurement of the pleth variability index (PVI), which multiple clinical studies have shown provides a new method for automatic, noninvasive assessment of a patient's ability to respond to fluid administration.[36][37][38] Appropriate fluid levels are vital to reducing postoperative risks and improving patient outcomes: fluid volumes that are too low (under-hydration) or too high (over-hydration) have been shown to decrease wound healing and increase the risk of infection or cardiac complications.[39] Recently, the National Health Service in the United Kingdom and the French Anesthesia and Critical Care Society listed PVI monitoring as part of their suggested strategies for intra-operative fluid management.[40][41]
Function
A blood-oxygen monitor displays the percentage of blood that is loaded with oxygen. More specifically, it measures what percentage of hemoglobin, the protein in blood that carries oxygen, is loaded. Acceptable normal ranges for patients without pulmonary pathology are from 95 to 99 percent. For a patient breathing room air at or near sea level, an estimate of arterial pO2 can be made from the blood-oxygen monitor "saturation of peripheral oxygen" (SpO2) reading.
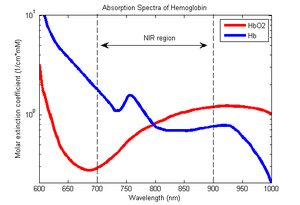
A typical pulse oximeter uses an electronic processor and a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient's body, usually a fingertip or an earlobe. One LED is red, with wavelength of 660 nm, and the other is infrared with a wavelength of 940 nm. Absorption of light at these wavelengths differs significantly between blood loaded with oxygen and blood lacking oxygen. Oxygenated hemoglobin absorbs more infrared light and allows more red light to pass through. Deoxygenated hemoglobin allows more infrared light to pass through and absorbs more red light. The LEDs sequence through their cycle of one on, then the other, then both off about thirty times per second which allows the photodiode to respond to the red and infrared light separately and also adjust for the ambient light baseline.[42] The amount of light that is transmitted (in other words, that is not absorbed) is measured, and separate normalized signals are produced for each wavelength. These signals fluctuate in time because the amount of arterial blood that is present increases (literally pulses) with each heartbeat. By subtracting the minimum transmitted light from the peak transmitted light in each wavelength, the effects of other tissues are corrected for.[43] The ratio of the red light measurement to the infrared light measurement is then calculated by the processor (which represents the ratio of oxygenated hemoglobin to deoxygenated hemoglobin), and this ratio is then converted to SpO2 by the processor via a lookup table[43] based on the Beer–Lambert law.[42]
Indication

A pulse oximeter is a medical device that indirectly monitors the oxygen saturation of a patient's blood (as opposed to measuring oxygen saturation directly through a blood sample) and changes in blood volume in the skin, producing a photoplethysmogram. The pulse oximeter may be incorporated into a multiparameter patient monitor. Most monitors also display the pulse rate. Portable, battery-operated pulse oximeters are also available for transport or home blood-oxygen monitoring.[citation needed]
Advantages
Pulse oximetry is particularly convenient for noninvasive continuous measurement of blood oxygen saturation. In contrast, blood gas levels must otherwise be determined in a laboratory on a drawn blood sample. Pulse oximetry is useful in any setting where a patient's oxygenation is unstable, including intensive care, operating, recovery, emergency and hospital ward settings, pilots in unpressurized aircraft, for assessment of any patient's oxygenation, and determining the effectiveness of or need for supplemental oxygen. Although a pulse oximeter is used to monitor oxygenation, it cannot determine the metabolism of oxygen, or the amount of oxygen being used by a patient. For this purpose, it is necessary to also measure carbon dioxide (CO2) levels. It is possible that it can also be used to detect abnormalities in ventilation. However, the use of a pulse oximeter to detect hypoventilation is impaired with the use of supplemental oxygen, as it is only when patients breathe room air that abnormalities in respiratory function can be detected reliably with its use. Therefore, the routine administration of supplemental oxygen may be unwarranted if the patient is able to maintain adequate oxygenation in room air, since it can result in hypoventilation going undetected.[44]
Because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation values, pulse oximeters are of critical importance in emergency medicine and are also very useful for patients with respiratory or cardiac problems, especially COPD, or for diagnosis of some sleep disorders such as apnea and hypopnea.[45] Portable battery-operated pulse oximeters are useful for pilots operating in a non-pressurized aircraft above 10,000 feet (12,500 feet in the U.S.)[46] where supplemental oxygen is required. Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at high altitudes or with exercise. Some portable pulse oximeters employ software that charts a patient's blood oxygen and pulse, serving as a reminder to check blood oxygen levels.
Limitations
Pulse oximetry measures solely hemoglobin saturation, not ventilation and is not a complete measure of respiratory sufficiency. It is not a substitute for blood gases checked in a laboratory, because it gives no indication of base deficit, carbon dioxide levels, blood pH, or bicarbonate (HCO3−) concentration. The metabolism of oxygen can be readily measured by monitoring expired CO2, but saturation figures give no information about blood oxygen content. Most of the oxygen in the blood is carried by hemoglobin; in severe anemia, the blood will carry less total oxygen, despite the hemoglobin being 100% saturated.[citation needed]
Erroneously low readings may be caused by hypoperfusion of the extremity being used for monitoring (often due to a limb being cold, or from vasoconstriction secondary to the use of vasopressor agents); incorrect sensor application; highly calloused skin; or movement (such as shivering), especially during hypoperfusion. To ensure accuracy, the sensor should return a steady pulse and/or pulse waveform. Pulse oximetry technologies differ in their abilities to provide accurate data during conditions of motion and low perfusion.[15][47]
Pulse oximetry also is not a complete measure of circulatory sufficiency. If there is insufficient bloodflow or insufficient hemoglobin in the blood (anemia), tissues can suffer hypoxia despite high oxygen saturation in the blood that does arrive. In 2008, a pulse oximeter that can measure hemoglobin levels in addition to oxygen saturation was introduced by Masimo. To quantify hemoglobin, the device uses additional wavelengths of light beyond the two standard ones.[citation needed]
Since pulse oximetry measures only the percentage of bound hemoglobin, a falsely high or falsely low reading will occur when hemoglobin binds to something other than oxygen:
- Hemoglobin has a higher affinity to carbon monoxide than it does to oxygen, and a high reading may occur despite the patient's actually being hypoxemic. In cases of carbon monoxide poisoning, this inaccuracy may delay the recognition of hypoxia (low cellular oxygen level).
- Cyanide poisoning gives a high reading because it reduces oxygen extraction from arterial blood. In this case, the reading is not false, as arterial blood oxygen is indeed high in early cyanide poisoning.
- Methemoglobinemia characteristically causes pulse oximetry readings in the mid-80s.
- COPD [especially chronic bronchitis] may cause false readings.[48]
A noninvasive method that allows continuous measurement of the dyshemoglobins is the pulse CO-oximeter, which was invented in 2005 by Masimo. It provides clinicians a way to measure the dyshemoglobins, carboxyhemoglobin, and methemoglobin along with total hemoglobin.
Increasing usage
According to a report by iData Research the U.S. pulse oximetry monitoring market for equipment and sensors was over 700 million USD in 2011.[49]
In 2008, more than half of the major internationally exporting medical equipment manufacturers in China were producers of pulse oximeters.[50]
The Apple Watch uses this technology for its heart rate monitor.[51][52] The accuracy of the heart rate monitor has been debated, as different tests have shown it to be 91% as accurate as chest strap monitors. [53][54]
Pleth variability index
Pleth variability index (PVI) is a measure of the variability of the plethysmographic waveform amplitude.[55]
See also
- Arterial blood gas
- Capnography
- Integrated Pulmonary Index
- Respiratory monitoring
- Medical equipment
- Mechanical ventilation
- Oxygen sensor
- Oxygen saturation
- Photoplethysmogram, measuring of carbon dioxide (CO2) in the respiratory gases
- Sleep apnea
References
- ^ Brand TM, Brand ME, Jay GD (February 2002). "Enamel nail polish does not interfere with pulse oximetry among normoxic volunteers". J Clin Monit Comput. 17 (2): 93–6. doi:10.1023/A:1016385222568. PMID 12212998.
- ^ Jorgensen JS, Schmid ER, Konig V, Faisst K, Huch A, Huch R (1995). "Limitations of forehead pulse oximetry". J Clin Monit. 11 (4): 253–256. doi:10.1007/bf01617520.
- ^ Matthes, K (1935). "Untersuchungen über die Sauerstoffsättigung des menschlichen Arterienblutes" [Studies on the Oxygen Saturation of Arterial Human Blood]. Naunyn-Schmiedeberg's Archives of Pharmacology (in German). 179 (6): 698–711. doi:10.1007/BF01862691.
- ^ Millikan G. A. (1942). "The oximeter: an instrument for measuring continuously oxygen saturation of arterial blood in man". Review of Scientific Instruments. 13 (10): 434–444. Bibcode:1942RScI...13..434M. doi:10.1063/1.1769941.
- ^ Severinghaus, John W.; Honda, Yoshiyuki (April 1987). "History of Blood Gas Analysis. VII. Pulse Oximetry" (PDF). Journal of Clinical Monitoring. 3 (2): 135–138. doi:10.1007/bf00858362. PMID 3295125. Archived from the original (PDF) on 2008-11-16.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "510(k) Premarket Notification". www.accessdata.fda.gov. Retrieved 2017-02-23.
- ^ . doi:10.1007/bf00858362.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ http://www.masimo.co.uk/nellcorfiction/index.htm[full citation needed]
- ^ Lin JC, Strauss RG, Kulhavy JC, et al. Phlebotomy overdraw in the neonatal intensive care nursery. Pediatrics Aug 2000;106(2):E19.
- ^ Barker SJ (2002). ""Motion-resistant" pulse oximetry: a comparison of new and old models". Anesth Analg. 95 (4): 967–972. doi:10.1213/00000539-200210000-00033.
- ^ Barker SJ, Shah NK (1997). "The effects of motion on the performance of pulse oximeters in volunteers (revised publication)". Anesthesiology. 86 (1): 101–108. doi:10.1097/00000542-199701000-00014.
- ^ Jopling MW, Mannheimer PD, Bebout DE (2002). "Issues in the laboratory evaluation of pulse oximeter performance". Anesth Analg. 94: S62–68. PMID 11900041.
- ^ Shah N, Ragaswamy HB, Govindugari K, Estanol L. "Performance of three new-generation pulse oximeters during motion and low perfusion in volunteers". J Clin Anesth. 24: 385–391. doi:10.1016/j.jclinane.2011.10.012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Barker SJ (2002). "Motion-resistant" pulse oximetry: a comparison of new and old models". Anesth Analg. 95: 967–72. doi:10.1213/00000539-200210000-00033.
- ^ a b . doi:10.1016/j.jclinane.2011.10.012.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ Hay WW Jr, Rodden DJ, Collins SM, Melara DL, Hale KA, Fashaw LM (2002). "Reliability of conventional and new pulse oximetry in neonatal patients". J Perinatol. 22: 360–6. doi:10.1038/sj.jp.7210740.
- ^ Castillo A, Deulofeut R, Critz A, Sola A (2010). "Prevention of retinopathy of prematurity in preterm infants through changes in clinical practice and SpO(2)technology". Acta Paediatr. 100: 188–92. doi:10.1111/j.1651-2227.2010.02001.x. PMC 3040295. PMID 20825604.
- ^ Durbin CG, Rostow SK (2002). "More reliable oximetry reduces the frequency of arterial blood gas analyses and hastens oxygen weaning after cardiac surgery: A prospective, randomized trial of the clinical impact of a new technology". Crit Care Med. 30: 1735–40. doi:10.1097/00003246-200208000-00010.
- ^ Taenzer AH, Pyke JB, McGrath SP, Blike GT (2010). "The impact of pulse oximetry surveillance on rescue events and intensive care unit transfers a before-and-after concurrence study". Anesthesiology. 112: 282–7. doi:10.1097/aln.0b013e3181ca7a9b. PMID 20098128.
- ^ . doi:10.1542/peds.2011-1317.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ . doi:10.1136/bmj.a3037.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ . doi:10.1016/S0140-6736(11)60753-8.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ Mahle WT, Martin GR, Beekman RH 3rd, Morrow WR (2014-11-12). "Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease". Pediatrics. 129: 190–2. doi:10.1542/peds.2011-3211. PMID 22201143.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ "Newborn CCHD Screening Progress Map | Updated 7/7/2014". Cchdscreeningmap.org. Retrieved 2015-04-02.
- ^ . doi:10.1016/S0140-6736(14)60198-7.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ [1] Archived February 10, 2012, at the Wayback Machine
- ^ [2] Archived January 7, 2009, at the Wayback Machine
- ^ "Home". Anesthesiology.org. Retrieved 2015-04-02.
- ^ Chung F, Liao P, Elsaid H, Islam S, Shapiro CM, Sun Y. "Oxygen desaturation index from nocturnal oximetry: a sensitive and specific tool to detect sleep-disordered breathing in surgical patients". Anesth Analg. 114: 993–1000. doi:10.1213/ane.0b013e318248f4f5.
- ^ De Felice C, Leoni L, Tommasini E, Tonni G, Toti P, Del Vecchio A, Ladisa G, Latini G (2008). "Maternal pulse oximetry perfusion index as a predictor of early adverse respiratory neonatal outcome after elective cesarean delivery". Pediatric Critical Care Medicine. 9: 203–8. doi:10.1097/pcc.0b013e3181670021.
- ^ De Felice C, Latini G, Vacca P, Kopotic RJ (2002). "The pulse oximeter perfusion index as a predictor for high illness severity in neonates". Eur J Pediatr. 161: 561–2. doi:10.1007/s00431-002-1042-5.
- ^ De Felice C, Goldstein MR, Parrini S, Verrotti A, Criscuolo M, Latini G. Early dynamic changes in pulse oximetry signals in preterm newborns with histologic chorioamnionitis. Pediatric Critical Care Medicine 2006;7:138–42.
- ^ Takahashi S, Kakiuchi S, Nanba Y, Tsukamoto K, Nakamura T, Ito Y. "The perfusion index derived from a pulse oximeter for predicting low superior vena cava flow in very low birth weight infants". J Perinatol. 30: 265–9. doi:10.1038/jp.2009.159. PMC 2834357.
- ^ Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM (2009). "Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia". Acta Anaesthesiol Scand. 53: 1018–26. doi:10.1111/j.1399-6576.2009.01968.x.
- ^ Granelli AW, Ostman-Smith I (2007). "Noninvasive peripheral perfusion index as a possible tool for screening for critical left heart obstruction". Acta Paediatr. 96: 1455–9. doi:10.1111/j.1651-2227.2007.00439.x.
- ^ . doi:10.1097/EJA.0b013e328335fbd1.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ Cannesson M, Desebbe O, Rosamel P, Delannoy B, Robin J, Bastien O, Lehot JJ (Aug 2008). "Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theater". Br J Anaesth. 101 (2): 200–6. doi:10.1093/bja/aen133.
- ^ Forget P, Lois F, de Kock M. Goal-Directed Fluid Management Based on the Pulse Oximeter-Derived Pleth Variability Index Reduces Lactate Levels and Improves Fluid Management. Anesth Analg 2010.
- ^ Ishii M, Ohno K; Ohno (1977). "Comparisons of body fluid volumes, plasma renin activity, hemodynamics and pressor responsiveness between juvenile and aged patients with essential hypertension". Jpn. Circ. J. 41 (3): 237–46. doi:10.1253/jcj.41.237. PMID 870721.
- ^ "[ARCHIVED CONTENT] NHS Technology Adoption Centre". Ntac.nhs.uk. Retrieved 2015-04-02.
- ^ [3] Archived October 12, 2014, at the Wayback Machine
- ^ a b "Principles of pulse oximetry". Anaesthesia UK. 11 Sep 2004. Archived from the original on 2015-02-24. Retrieved 2015-02-24.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b "Pulse Oximetry". Oximetry.org. 2002-09-10. Archived from the original on 2015-03-18. Retrieved 2015-04-02.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ . doi:10.1378/chest.126.5.1552.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ Schlosshan, D; Elliott, M W (2004). "Sleep 3: Clinical presentation and diagnosis of the obstructive sleep apnoea hypopnoea syndrome". Thorax. 59: 347–352. doi:10.1136/thx.2003.007179. PMC 1763828.
- ^ "FAR Part 91 Sec. 91.211 effective as of 09/30/1963". Airweb.faa.gov. Retrieved 2015-04-02.
- ^ Barker SJ (2002). ""Motion-resistant" pulse oximetry: a comparison of new and old models". Anesth Analg. 95: 967–72. doi:10.1213/00000539-200210000-00033.
- ^ . doi:10.4187/respcare.04435.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ^ U.S. Market for Patient Monitoring Equipment. iData Research. May 2012
- ^ "Key Portable Medical Device Vendors Worldwide". China Portable Medical Devices Report. ResearchInChina. December 2008.
- ^ http://9to5mac.com/2015/04/24/apple-watch-blood-oxygen/
- ^ https://support.apple.com/en-us/HT204666[full citation needed]
- ^ https://www.npr.org/sections/health-shots/2016/10/15/497828894/you-can-monitor-your-heart-with-a-smartphone-but-should-you[full citation needed]
- ^ https://breakingmuscle.com/fitness/chest-strap-vs-wristband-heart-rate-monitors[full citation needed]
- ^ . doi:10.1093/bja/aen133.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help)
