Behçet's disease of the optic nerve: Difference between revisions
No edit summary |
No edit summary |
||
| Line 34: | Line 34: | ||
== Pathophysiology == |
== Pathophysiology == |
||
[[Image:HLA-B*5101.png|thumb|right|[[HLA-B51]] |
|||
[[Vasculitis]] resulting in occlusion of the vessels supplying the optic nerve may be the cause of acute optic neuropathy and progressive optic atrophy in Behcet’s disease. Histological evaluation in a reported case of acute optic neuropathy demonstrated substitution of the axonal portion of the optic nerve with fibrous astrocytes without retinal changes.[3] CNS involvement in Behcet’s may lead to intracranial hypertension most commonly due to dural venous sinus thrombosis[2, 8-10] and subsequent secondary optic atrophy. |
[[Vasculitis]] resulting in occlusion of the vessels supplying the optic nerve may be the cause of acute optic neuropathy and progressive optic atrophy in Behcet’s disease. Histological evaluation in a reported case of acute optic neuropathy demonstrated substitution of the axonal portion of the optic nerve with fibrous astrocytes without retinal changes.[3] CNS involvement in Behcet’s may lead to intracranial hypertension most commonly due to dural venous sinus thrombosis[2, 8-10] and subsequent secondary optic atrophy. |
||
Revision as of 00:18, 20 September 2009
| Behçet's disease of the optic nerve |
|---|
Optic nerve involvement in Behcet’s disease is rare. However, progressive optic atrophy and visual loss does occur. Acute optic atrophy and Anterior ischemic optic neuropathy (AION) have been reported in Behcet’s disease.
Background

Behçet's disease is a systemic immune-mediated vasculitis with major symptoms including oral and genital ulcers, skin lesions and ocular inflammation. Ocular Behcet’s occurs in 60-80% of patients with Behcet’s disease and can affect both the anterior and posterior chambers of the eye. Common ocular manifestations include anterior and/or posterior uveitis, retinal vasculitis and occlusion, macular edema, optic disk hyperemia, iridocyclitis, hypopyon and vitreitis.
Behcet’s disease may result in primary or secondary optic nerve involvement. Optic nerve atrophy has been identified as the most common cause of visual impairment in ocular Behcet’s disease.[1] Papilledema as a result of dural sinus thrombosis[2] and atrophy consecutive to retinal disease, have been characterized as secondary causes of optic nerve atrophy in Behcet’s disease.[1, 3]
Acute optic neuropathy in Behcet’s disease has been reported.[4-6] In cases of acute optic neuropathy, symptoms were often associated with exacerbations or relapse of systemic disease. Moreover, visual symptoms may herald the onset of CNS manifestations of the disease. Acute optic neuropathy may be unilateral or bilateral at its onset and may recur or come to involve the contralateral eye. [4-6]
Epidemiology
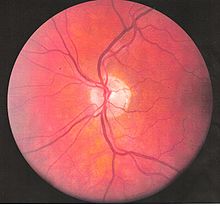
In an epidemiologic study by Krause et al., 56% of patient’s with Behcet’s Disease developed ocular involvement at a mean age of 30. Ocular involvement was the first manifestation of Behcet’s disease in 8.6% of patients.[7] Ocular Behcet’s with involvement of the optic nerve is rarely reported. Among patients with ocular Behcet’s disease fundoscopic findings of optic atrophy, and optic disc paleness have been identified with a frequency of 17.9% and 7.4%, respectively. Other fundoscopic findings include vascular sheathing(23.7%), retinal hemorrhage(9%), macular edema(11.3%), branch retinal vein occlusion(5.8%), and retinal edema(6.6%). However, optic atrophy was the most significant cause of visual impairment identified in 54% of patients with Ocular Behcet’s disease and permanent visual impairment.[1]
Pathophysiology
[[Image:HLA-B*5101.png|thumb|right|HLA-B51 Vasculitis resulting in occlusion of the vessels supplying the optic nerve may be the cause of acute optic neuropathy and progressive optic atrophy in Behcet’s disease. Histological evaluation in a reported case of acute optic neuropathy demonstrated substitution of the axonal portion of the optic nerve with fibrous astrocytes without retinal changes.[3] CNS involvement in Behcet’s may lead to intracranial hypertension most commonly due to dural venous sinus thrombosis[2, 8-10] and subsequent secondary optic atrophy.
Signs and Symptoms
[[Image:eye_dilate.gif|thumb|left|alt=A Animation that illustrates the pupillary light reflex. When the light is turned on, the pupil reacts by constricting.|The Wikipede edits Pupillary light reaction.]] Signs and symptoms of acute optic neuropathy include painless loss of vision which may affect either one or both eyes, reduced visual acuity, reduced color vision, Relative Afferent Pupillary Defect, central scotoma, swollen optic disc, macular edema, or retrobulbar pain. When these symptoms occur with concurrent mucocutaneous ulcerations, they raise suspicion of acute optic neuropathy in Behcet’s Disease. Progressive optic atrophy may result in decreased visual acuity or color vision. Intracranial hypertension with papilledema may be present.
Diagnosis
Vision, or color vision loss with concurrent mucocutaneous lesions and/or systemic Behcet’s symptoms should raise suspicion of optic nerve involvement in Behcet’s disease and prompt a work-up for Behcet’s disease if not previously diagnosed in addition to an ocular work-up. Diagnosis of Behcet’s disease is based on clinical findings including oral and genital ulcers, skin lesions such as erythema nodosum, acne, or folliculitis, ocular inflammatory findings and a pathergy reaction. Inflammatory markers such ESR, and CRP may be elevated. A complete ophthalmic examination may include a slit lamp examination, optical coherence tomography to detect nerve loss, visual field examinations, fundoscopic examination to assess optic disc pallor and retinal disease, fundoscopic angiography, and visual evoked potentials, which may demonstrate increased latency. Optic nerve enhancement may be identified on Magnetic Resonance Imaging in some patients with acute optic neuropathy. However, a normal study does not rule out optic neuropathy. Cerebrospinal fluid (CSF) analysis may demonstrate elevated protein level with or without pleocytosis. Imaging including angiography may be indicated to identify dural venous sinus thrombosis as a cause of intracranial hypertension and optic atrophy.
Differential Diagnosis
Leber's hereditary optic neuropathy
Anterior Ischemic Optic Neuropathy (AION)
Temporal Arteritis (Non-arteritic AION)
Posterior Ischemic Optic Neuropathy
Cerebral venous sinus thrombosis
Treatment/Prognosis
The optimal treatment for acute optic neuropathy in Behçet's disease has not been established given its rarity. Early identification and treatment is essential. Response to cyclosporine A, periocular triamcinolone, and IV methylprednisone followed by oral prednisone has been reported although relapses leading to irreversible visual loss may occur with treatment.[5] Immunosuppresants such as interferon alphan and tumour necorsis factor antagonists may improve though not reverse symptoms of Ocular Behcet’s, which may progress over time despite treatment. When symptoms are limited to the anterior chamber of the eye prognosis is improved. Posterior involvement, particularly optic nerve involvement is a poor prognostic indicator. Secondary optic nerve atrophy is frequently irreversible. Lumbar puncture or surgical treatment may be required to prevent optic atrophy in cases of intracranial hypertension refractory to treatment with immunomodulators and steroids.
External links
http://www.behcet.org.il/ohnotalkE.htm
References
1. Ozdal, P.C., et al., Posterior segment involvement in ocular Behcet's disease. Eur J Ophthalmol, 2002. 12(5): p. 424-31.
2. Bank, I. and C. Weart, Dural sinus thrombosis in Behcet's disease. Arthritis Rheum, 1984. 27(7): p. 816-8.
3. Kansu, T., et al., Optic neuropathy in Behcet's disease. J Clin Neuroophthalmol, 1989. 9(4): p. 277-80.
4. Salvi, F., et al., Optic neuropathy in Behcet's disease. Report of two cases. Ital J Neurol Sci, 1999. 20(3): p. 183-6.
5. Voros, G.M., S.S. Sandhu, and R. Pandit, Acute optic neuropathy in patients with Behcet's disease. Report of two cases. Ophthalmologica, 2006. 220(6): p. 400-5.
6. Yamauchi, Y., et al., Suspected simultaneous bilateral anterior ischemic optic neuropathy in a patient with Behcet's disease. Ocul Immunol Inflamm, 2005. 13(4): p. 317-25.
7. Krause, L., et al., Ocular involvement in Adamantiades-Behcet's disease in Berlin, Germany. Graefes Arch Clin Exp Ophthalmol, 2009. 247(5): p. 661-6.
8. Brissaud, P., et al., Digital angiography for the diagnosis of dural sinus thrombosis in Behcet's disease. Arthritis Rheum, 1985. 28(3): p. 359-60.
9. el-Ramahi, K.M. and M.Z. al-Kawi, Papilloedema in Behcet's disease: value of MRI in diagnosis of dural sinus thrombosis. J Neurol Neurosurg Psychiatry, 1991. 54(9): p. 826-9.
10. Fujikado, T. and K. Imagawa, Dural sinus thrombosis in Behcet's disease--a case report. Jpn J Ophthalmol, 1994. 38(4): p. 411-6.
