Urorectal septum
| Urorectal septum | |
|---|---|
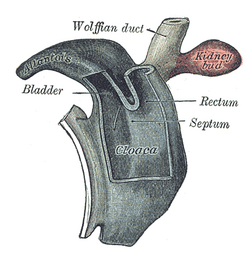 Cloaca of human embryo from twenty-five to twenty-seven days old. | |
| Details | |
| Days | 32 |
| Precursor | Cloaca |
| System | Genitourinary system |
| Identifiers | |
| Latin | septum urorectale |
| TE | septum_by_E5.4.9.0.2.0.14 E5.4.9.0.2.0.14 |
| Anatomical terminology | |
The urorectal septum is an invagination of the cloaca. It divides it into a dorsal part (the hindgut) and a ventral part (the urogenital sinus). It invaginates from cranial to caudal, formed from the endodermal cloaca, and fuses with the cloacal membrane. Malformations can cause fistulas.
Structure
[edit]The urorectal septum is an embryonic structure formed from an invagination of the cloaca. The urorectal septum divides the cloaca into two parts:
- a dorsal part, forming part of the hindgut, which forms the rectum and the anus.[1]
- a ventral part, forming the urogenital sinus, which forms the allantois, which becomes the urinary bladder.[1]
The urorectal septum becomes part of the perineal body, helping to form the perineum.[1]
Development
[edit]The urorectal septum develops from cranial to caudal, and is flat in the coronal plane.[1] It is formed from endoderm, the same germ layer as the cloaca. It fuses with the cloacal membrane.
Clinical significance
[edit]Urorectal septum malformation
[edit]Malformation of the urorectal septum can lead to several different types of fistulas.[2][3]
Classification
[edit]In women, at least five different types of fistula are possible.[3] All of these involve the fusion of the urogenital sinus and the end of the hindgut, causing the rectum to end in the vagina.[3] This may be associated with the uterus in the normal position, posterior to the hindgut, or bicornuate.[3]
In men, at least three different types of fistula are possible.[3] The hindgut may enter and preserve the urogenital sinus after birth.[3] The hindgut may replace the urogenital sinus completely, in which case it may also replace the urinary bladder and cause the ureters to drain into it.[3]
Prognosis
[edit]Urorectal septum malformation is associated with a number of other birth defects, including spina bifida, deafness, sacral hypoplasia, atrial septal defect, ventricular septal defect, tetralogy of Fallot, and limb musculoskeletal disorders.[3] Mainly because of these associations, up to 20% of children born with urorectal septum malformation may not survive long-term.[3] Outcomes from corrective surgery on a urorectal septum fistula are very good.[3]
References
[edit]![]() This article incorporates text in the public domain from page 1109 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 1109 of the 20th edition of Gray's Anatomy (1918)
- ^ a b c d Hynes, Pat J.; Fraher, John P. (January 2004). "The development of the male genitourinary system. I. The origin of the urorectal septum and the formation of the perineum". British Journal of Plastic Surgery. 57 (1): 27–36. doi:10.1016/j.bjps.2003.08.019. ISSN 0007-1226. PMID 14672675 – via ScienceDirect.
{{cite journal}}: CS1 maint: date and year (link) - ^ Escobar LF, Heiman M, Zimmer D, Careskey H (2007). "Urorectal septum malformation sequence: Prenatal progression, clinical report, and embryology review". Am. J. Med. Genet. A. 143 (22): 2722–6. doi:10.1002/ajmg.a.31925. PMID 17937427. S2CID 19219635.
- ^ a b c d e f g h i j Wheeler, Patricia G.; Weaver, David D. (2001). "Partial urorectal septum malformation sequence: A report of 25 cases". American Journal of Medical Genetics. 103 (2): 99–105. doi:10.1002/ajmg.1510. ISSN 1096-8628. PMID 11568914.
External links
[edit]- Subdividing the cloaca
- Parts of the Digestive System
- http://cancerweb.ncl.ac.uk/cgi-bin/omd?urorectal+septum Archived 2008-12-01 at the Wayback Machine
- http://isc.temple.edu/marino/embryology/parch98/parch_text.htm Archived 2007-09-09 at the Wayback Machine
- http://www.med.mun.ca/anatomyts/renal/akid5.htm Archived 2007-11-14 at the Wayback Machine
- http://isc.temple.edu/marino/embryology/parch98/parch_text.htm Archived 2007-09-09 at the Wayback Machine
