Pulmonary surfactant
Pulmonary surfactant is a surface agent formed by type II aleveolar cells. The proteins and lipids that comprise surfactant have both a hydrophilic region and a hydrophobic region, and so reduce the surface tension of water. It does this by moving to the surface region of the liquid with the hydrophilic tails in the water and hydrophobic heads facing towards the air.
Function
- To increase pulmonary compliance
- To prevent the lung collapsing into one large alveolus
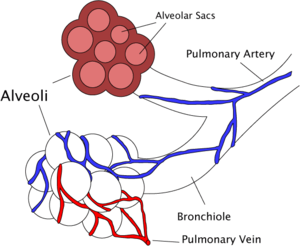
In the lungs you have a situation similar to that of an air bubble in water, as the alveoli are wet and surround a central air space. In this situation, the surface tension serves to try to make the bubble smaller, and this is counteracted by the pressure of the gas. Laplace’s equation expresses this equilibrium:
Compliance
This causes the surface tension part of elastic recoil observed by Neergaard. If the lungs did not secrete surfactant, this surface tension would be much higher and it would not be able to inflate normally. The normal surface tension for water is 70 dynes/cm and in the lungs it is 25 dynes/cm.
Once released into the surface water layer, the surfactant forms a meshwork of tubular myelin. This can be broken down both by macrophages and reabsorbed into lamella structures.
Pulmonary surfactant greatly reduces surface tension, increasing compliance allowing the lung to inflate much more easily. It reduces the pressure difference needed to allow the lung to inflate. The reduction in surface tension also reduces fluid accumulation in the alveolus as the surface tension draws fluid across the alveolar wall and when surfactant is not present, this force is higher.
Alveolar size regulation
As the alveoli increase in size, the surfactant becomes more spread out over the surface of the liquid. This increases surface tension effectively slowing the rate of increase of the alveoli. This also helps all alveoli in the lungs expand at the same rate, as one that increases more quickly will experience a large rise in surface tension slowing its rate of expansion. It also means the rate of shrinking is more regular as if one reduces in size more quickly the surface tension will reduce more so other alveoli can contract more easily than it.
Composition
Lipids
Over 90% of the surfactant is lipids; around half of which is dipalmitoylphosphatidylcholine (DPPC). This is structurally similar to a phospholipid as it has 2 16-carbon saturated chains and a phosphate group with quaternary amine group attached. Phosphatidylcholine molecules form ~35% of the lipid in surfactant and have unsaturated fatty acid chains. Phosphatidylglycerol forms about 11% of the lipids in surfactant, it also has unsaturated fatty acid chains. The components for these lipids diffuse from the blood into type II alveolar cells.
Proteins
The remaining 10% of surfactant is comprised of proteins. Half of this is plasma proteins but the rest is formed by apoproteins. These are SP-A,B,C and D. SP-A and SP-D confer innate immunity as they have carbohydrate recognition domains that allow them to coat bacteria and viruses promoting phagocytosis by macrophages. SP-A is also thought to be involved in a negative feedback mechanism to control the production of surfactant. SP-B and C are hydrophobic and are membrane proteins that increase the rate that surfactant spreads over the surface.
The apoproteins are produced by the secretory pathway in type II cells. They undergo much post-translational modification, ending up in the lamellar bodies. These are concentric rings of lipid and protein, about 1μm in diameter. Pulmonary surfactant in secreted by exocytosis.
Diseases
Infant respiratory distress syndrome (IRDS) is caused by lack of surfactant, commonly suffered by premature babies.
Hyaline membrane disease is also associated with dysfunction of surfactant.

