Holter monitor
 Holter monitor | |
| Inventor | Norman Holter |
|---|---|
In medicine, a Holter monitor (often simply "Holter" or occasionally ambulatory electrocardiography device) is a portable device for continuously monitoring various electrical activity of the central nervous system for at least 24 hours (modern Holters allow up to 11 days of monitoring). The Holter's most common use is for monitoring heart activity (electrocardiography or ECG), but it can also be used for monitoring brain activity (electroencephalography or EEG). Its extended recording period is sometimes useful for observing occasional cardiac arrhythmias or epileptic events which would be difficult to identify in a shorter period of time. For patients having more transient symptoms, a cardiac event monitor which can be worn for a month or more can be used.
The Holter monitor is named for Dr. Norman J. Holter who invented telemetric cardiac monitoring in 1949.[1] Clinical use started in the early 1960s.[1]
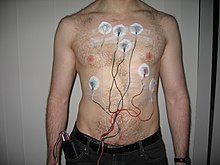
When used for the heart, much like standard electrocardiography the Holter monitor records electrical signals from the heart via a series of electrodes attached to the chest. Electrodes are placed over bones to minimize artifacts from muscular activity. The number and position of electrodes varies by model, but most Holter monitors employ between three and eight. These electrodes are connected to a small piece of equipment that is attached to the patient's belt or hung around the neck, and is responsible for keeping a log of the heart's electrical activity throughout the recording period.
Older devices used reel to reel tapes or a standard C90 or C120 audio cassette and ran at a 1.7mm or 2mm/second speed to record the data. Once a recording was made, it could be played back and analysed at 60x speed so 24 hours of recording could be analysed in 24 minutes. More modern units record onto digital flash memory devices. The data are uploaded into a computer which then automatically analyzes the input, counting ECG complexes, calculating summary statistics such as average heart rate, minimum and maximum heart rate, and finding candidate areas in the recording worthy of further study by the technician.
Recorder
Each Holter system consists of two basic parts – the hardware (called monitor or recorder) for recording the signal and software for review and analysis of the record. Advanced Holter recorders are able to display the signal, which is very useful for checking the signal quality. Very often there is also a “patient button” located on the front site allowing the patient to press it in specific cases such as sickness, going to bed, taking pills…. A special mark will be then placed into the record so that the doctors or technicians can quickly pinpoint these areas when analyzing the signal. More modern devices also have the ability to record a vocal patient diary entry.
Size of recorder differs depending on manufacturer of the device. The average dimensions of today’s Holter monitors are about 110x70x30 mm. Most of the devices operate with two AA batteries. In case the batteries die, some Holters allow their replacement even during monitoring.
Most of the Holters monitor the ECG just in 2 or 3 channels. Depending on the model (manufacturer), different count of leads and lead systems are used. Today’s trend is to minimize such number to insure the patient’s comfort during recording. Although 2/3 channel recording has been used for a long time in the Holter monitoring history, recently 12 channel Holters have appeared. These systems use the classic Mason-Likar lead system, thus producing the signal in the same representation as during the common rest ECG and/or stress test measurement. These Holters then allow to substitute stress test examination in cases the stress test is not possible for the current patient. They are also suitable when analyzing patients after myocardial infarction. Recordings from these 12 lead monitors are of a significantly lower resolution than those from a standard 12 lead ECG and in some cases have been shown to provide misleading ST segment representation.
Analysing software
When the recording of ECG signal is finished (usually after 24 or 48 hours), it is up to the physician to perform the signal analysis. Since it would be extremely time demanding to browse through such a long signal, there is an integrated automatic analysis process in each Holter software which automatically determines different sorts of heart beats, rhythms, etc. However the success of the automatic analysis is very closely associated with the signal quality. The quality itself mainly depends on the attachment of the electrodes to the patient body. If these are not properly attached, the electromagnetic disturbance surrounding us will influence the ECG signal resulting thus in a very noisy record. If the patient moves rapidly, the distortion will be even bigger. Such record is then very difficult to process. Besides the attachment and quality of electrodes, there are other factors affecting the signal quality, such as muscle tremors, sampling rate and resolution of the digitized signal (high quality devices offer 2000Hz and 16 bits or higher).
The automatic analysis commonly provides the physician with information about heart beat morphology, beat interval measurement, heart rate variability, rhythm overview and patient diary (moments when the patient pressed the patient button). Advanced systems also perform spectral analysis, ischemic burden evaluation, graph of patient’s activity or PQ segment analysis. Another requirement is the ability of pacemaker detection and analysis. Such ability is useful when one wants to check the correct pacemaker function.
Wearing the monitor
Although there are many patients having fear of Holter examination, there is nothing to be worry about. There are no contraindications for this examination and it doesn’t interfere with the normal daily life much.
The recording device can be worn on a belt or in a case on a strap worn across the chest. Individuals who want to minimize the visibility of the device can wear layers or bulky clothes so the case is not as obvious. Also, because of the placement of the electrodes, individuals wearing a Holter monitor may wish to wear shirts with a high neck.
Patient wearing the monitor should act as he/she wouldn’t have any device with him/her self and not limit his/her normal daily activities. That’s because it is the intention to do the monitoring in normal life style conditions. Exceptions relate only to activities associated with water such as showering - although removal of the device and connected electrodes can be done occasionally. These situations can also happen during the batteries or electrodes change (both in case of multiple day monitoring).
Gallery
-
A Holter monitor can be worn for many days without causing significant discomfort.
-
Canine Holter Monitor with DogLeggs Vest
-
A Holter monitor with a US quarter dollar coin to show scale
-
Holter monitor can be worn with bra on woman, with no discomfort.
References
- ^ a b
Hilbel, Thomas (01/10/2008). "Telemetry in the clinical setting". Herzschrittmachertherapie & Elektrophysiologie. 19 (3): 146–64. ISSN 0938-7412. Retrieved 2009-Aug-04.
{{cite journal}}: Check date values in:|accessdate=and|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help)
External links
- Information on Holter Monitors for Patients
- Information on Holter Monitors for physicians.
- Holter monitor - MedLine Plus
- Holter monitor - Texas Heart Institute
- Holter Monitor information from Children's Hospital Heart Center, Seattle.
- How is a Holter test performed? - Information on what is the purpose of Holter monitoring and how it is performed.
- - An extensive range of Holter monitors




