Mitral valve
| Mitral valve | |
|---|---|
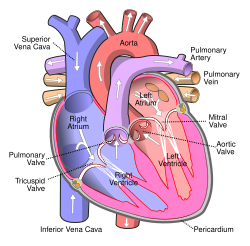 Anterior (frontal) view of the opened heart. White arrows indicate normal blood flow. (Mitral valve labeled at center right.) | |
 Base of ventricles exposed by removal of the atria. (Bicuspid (mitral) valve visible at bottom left.) | |
| Details | |
| Identifiers | |
| Latin | valva atrioventricularis sinistra, valva mitralis |
| MeSH | D008943 |
| TA98 | A12.1.04.003 |
| TA2 | 3987 |
| FMA | 7235 |
| Anatomical terminology | |
The mitral valve (also known as the bicuspid valve or left atrioventricular valve) is a dual-flap (bi- from the Latin, meaning double, and mitral- from the Latin, meaning shaped like a miter) valve in the heart that lies between the left atrium (LA) and the left ventricle (LV). The mitral valve and the tricuspid valve are known collectively as the atrioventricular valves because they lie between the atria and the ventricles of the heart and control the flow of blood.
Overview
A normally-functioning mitral valve opens secondary to increased pressure from the left atrium as it fills with blood. As the pressure increases above that of the left ventricle, the valve opens allowing blood to flow into the left ventricle during diastole (early rapid filling and atrial contraction), and closes at the end of atrial contraction to prevent blood flowing back
Anatomy
The mitral valve is typically 4-6 cm² in area. It has two cusps, or leaflets, (the anteromedial leaflet and the posterolateral leaflet) that guard the opening. The opening is surrounded by a fibrous ring known as the mitral valve annulus. (The orientation of the two leaflets resemble a bishop's miter, whence the valve receives its name.[1]) The anterior cusp protects approximately two-thirds of the valve (imagine a crescent moon within the circle, where the crescent represents the posterior cusp). Note that although the anterior leaflet takes up a larger part of the ring and rises higher, the posterior leaflet has a larger surface area. These valve leaflets are prevented from prolapsing into the left atrium by the action of tendons attached to the posterior surface of the valve, chordae tendineae.
The inelastic chordae tendineae are attached at one end to the papillary muscles and the other to the valve cusps. Papillary muscles are fingerlike projections from the wall of the left ventricle. Chordae tendineae from each muscle are attached to both leaflets of the mitral valve. Thus, when the left ventricle contracts, the intraventricular pressure forces the valve to close, while the tendons keep the leaflets coapting together and prevent the valve from opening in the wrong direction (thus preventing blood to flow back to the left atrium). Each chord has a different thickness. The thinnest ones are attached to the free leaflet margin, whereas thickest ones (strut chords) are attached quite away from the free margin. This disposition has important effects on systolic stress distribution physiology [2].
Normal physiology
During left ventricular diastole, after the pressure drops in the left ventricle due to relaxation of the ventricular myocardium, the mitral valve opens, and blood travels from the left atrium to the left ventricle. About 70-80% of the blood that travels across the mitral valve occurs during the early filling phase of the left ventricle. This early filling phase is due to active relaxation of the ventricular myocardium, causing a pressure gradient that allows a rapid flow of blood from the left atrium, across the mitral valve. This early filling across the mitral valve is seen on doppler echocardiography of the mitral valve as the E wave.
After the E wave, there is a period of slow filling of the ventricle.
Left atrial contraction (left atrial systole) (during left ventricular diastole) causes added blood to flow across the mitral valve immediately before left ventricular systole. This late flow across the open mitral valve is seen on doppler echocardiography of the mitral valve as the A wave. The late filling of the LV contributes about 20% to the volume in the left ventricle prior to ventricular systole, and is known as the atrial kick.
The mitral annulus changes in shape and size during the cardiac cycle. It is smaller at the end of atrial systole due to the contraction of the left atrium around it, like a sphincter. This reduction in annulus size at the end of atrial systole may be important for the proper coapting of the leaflets of the mitral valve when the left ventricle contracts and pumps blood.[3]
Surface anatomy
The closing of the mitral valve and the tricuspid valve constitutes the first heart sound (S1). It is not actually the valve closure which produces a sound but rather the sudden cessation of blood flow caused by the closure of the mitral and tricuspid valves. The mitral valve opening is normally not heard except in Mitral Stenosis (narrowing of the valve) as the Opening Snap. Flow of blood into the heart during rapid filling is not normally heard except in certain pathological states where it constitutes the third heart sound (S3).
Additional images
-
Section of the heart showing the ventricular septum. (Bicuspid valve visible at center.)
-
Apical view of valves
-
Cross-sectional view of mitral valve between left atrium (upper chamber) and left ventricle (lower chamber), which shows parts of walls of left atrium and left ventricle that are next to the mitral valve.
See also
- Anatomy
- Pathophysiology
- Procedures to fix the mitral valve
References
- ^ Template:Stedman's
- ^ Nazari S, Carli F, Salvi S; et al. (2000). "Patterns of systolic stress distribution on mitral valve anterior leaflet chordal apparatus. A structural mechanical theoretical analysis". J Cardiovasc Surg (Torino). 41 (2): 193–202. PMID 10901521.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pai RG, Varadarajan P, Tanimoto M (2003). "Effect of atrial fibrillation on the dynamics of mitral annular area". The Journal of Heart Valve Disease. 12 (1): 31–7. PMID 12578332. Retrieved 2010-03-04.
{{cite journal}}: Unknown parameter|unused_data=ignored (help)CS1 maint: multiple names: authors list (link)
External links
- Anatomy figure: 20:07-03 at Human Anatomy Online, SUNY Downstate Medical Center - "Valves of the heart."
- Mitral Valve Repair at The Mount Sinai Hospital - "Mitral Valve Function"
- Surgical Anatomy of the Mitral Valve at echoincontext.com
- Mitral Valve Repair at Englewood Hospital and Medical Center - Mitral Valve Repair
- Cardiac Valve Animations - Perioperative Interactive Education Group - Cardiac Valve
- Simulation of Blood Flow through the Mitral Valve of the Heart
Animations
♥




