Rasmussen syndrome: Difference between revisions
Marvin 101 (talk | contribs) →Investigations: Image: Brain biopsy in Rasmussen's encephalitis showing lymphocytic infiltrates staining for CD8 on immunohistochemistry]] |
|||
| Line 19: | Line 19: | ||
In Rasmussen’s encephalitis, there is [[chronic inflammation]] of the brain, with infiltration of [[T lymphocyte]]s into the brain tissue. This affects only one [[cerebral hemisphere]], either the left or the right. This inflammation causes permanent damage to the cells of the brain, leading to [[atrophy]] of the hemisphere; the epilepsy that this causes may itself contribute to the brain damage. |
In Rasmussen’s encephalitis, there is [[chronic inflammation]] of the brain, with infiltration of [[T lymphocyte]]s into the brain tissue. This affects only one [[cerebral hemisphere]], either the left or the right. This inflammation causes permanent damage to the cells of the brain, leading to [[atrophy]] of the hemisphere; the epilepsy that this causes may itself contribute to the brain damage. |
||
The cause of the inflammation is not known: infection by a [[virus]] has been suggested, but the evidence for this is inconclusive.<ref name="pmid15689357">{{cite journal |last = Bien |coauthors = Granata, Antozzi |title = Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: a European consensus statement |journal = Brain |volume = 128 |pages = 454–471 |year = 2005 |doi = 10.1093/brain/awh415 |id = 15689357 |pmid = 15689357 |first1 = CG |issue = Pt 3 |display-authors = 1}}</ref> In the 1990s it was suggested that [[auto-antibodies]] against the glutamate receptor [[GluR3]] were important in causing the disease,<ref name="pmid8036512">{{cite journal |author=Rogers SW |title=Autoantibodies to glutamate receptor GluR3 in Rasmussen's encephalitis |journal=Science |volume=265 |issue=5172 |pages=648–51 |year=1994 |pmid=8036512 |doi=10.1126/science.8036512 |author-separator=, |author2=Andrews PI |author3=Gahring LC |display-authors=3 |last4=Whisenand |first4=T |last5=Cauley |first5=K |last6=Crain |first6=B |last7=Hughes |first7=T. |last8=Heinemann |first8=S. |last9=McNamara |first9=J.}}</ref> but this is no longer thought to be the case.<ref name="pmid15249609">{{cite journal |author=Watson R |title=Absence of antibodies to glutamate receptor type 3 (GluR3) in Rasmussen encephalitis |journal=Neurology |volume=63 |issue=1 |pages=43–50 |year=2004 |pmid=15249609 |author-separator=, |author2=Jiang Y |author3=Bermudez I |display-authors=3 |last4=Houlihan |first4=L |last5=Clover |first5=L |last6=McKnight |first6=K |last7=Cross |first7=JH |last8=Hart |first8=IK |last9=Roubertie |first9=A |doi=10.1212/01.WNL.0000132651.66689.0F}}</ref> However, more recent studies report the '''presence of autoantibodies against the NMDA-type glutamate receptor subunit GluRepsilon2 (anti-NR2A antibodies)''' in a subset of patients with Rasmussen's encephalitis.<ref name="pmid15987271">{{cite journal |author=Takahashi Y |title=Autoantibodies and cell-mediated autoimmunity to NMDA-type GluRepsilon2 in patients with Rasmussen's encephalitis and chronic progressive epilepsia partialis continua |journal=Epilepsia |volume=46 |issue=Suppl 5 |pages=152–158 |year=2005 |pmid=15987271 |doi=10.1111/j.1528-1167.2005.01024.x |author-separator=, |author2=Mori H |author3=Mishina M |display-authors=3 |last4=Watanabe |first4=Masahiko |last5=Kondo |first5=Naomi |last6=Shimomura |first6=Jiro |last7=Kubota |first7=Yuko |last8=Matsuda |first8=Kazumi |last9=Fukushima |first9=Katsuyuki}}</ref> |
The cause of the inflammation is not known: infection by a [[virus]] has been suggested, but the evidence for this is inconclusive.<ref name="pmid15689357">{{cite journal |last = Bien |coauthors = Granata, Antozzi |title = Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: a European consensus statement |journal = Brain |volume = 128 |pages = 454–471 |year = 2005 |doi = 10.1093/brain/awh415 |id = 15689357 |pmid = 15689357 |first1 = CG |issue = Pt 3 |display-authors = 1}}</ref> In the 1990s it was suggested that [[auto-antibodies]] against the glutamate receptor [[GluR3]] were important in causing the disease,<ref name="pmid8036512">{{cite journal |author=Rogers SW |title=Autoantibodies to glutamate receptor GluR3 in Rasmussen's encephalitis |journal=Science |volume=265 |issue=5172 |pages=648–51 |year=1994 |pmid=8036512 |doi=10.1126/science.8036512 |author-separator=, |author2=Andrews PI |author3=Gahring LC |display-authors=3 |last4=Whisenand |first4=T |last5=Cauley |first5=K |last6=Crain |first6=B |last7=Hughes |first7=T. |last8=Heinemann |first8=S. |last9=McNamara |first9=J.}}</ref> but this is no longer thought to be the case.<ref name="pmid15249609">{{cite journal |author=Watson R |title=Absence of antibodies to glutamate receptor type 3 (GluR3) in Rasmussen encephalitis |journal=Neurology |volume=63 |issue=1 |pages=43–50 |year=2004 |pmid=15249609 |author-separator=, |author2=Jiang Y |author3=Bermudez I |display-authors=3 |last4=Houlihan |first4=L |last5=Clover |first5=L |last6=McKnight |first6=K |last7=Cross |first7=JH |last8=Hart |first8=IK |last9=Roubertie |first9=A |doi=10.1212/01.WNL.0000132651.66689.0F}}</ref> However, more recent studies report the '''presence of autoantibodies against the NMDA-type glutamate receptor subunit GluRepsilon2 (anti-NR2A antibodies)''' in a subset of patients with Rasmussen's encephalitis.<ref name="pmid15987271">{{cite journal |author=Takahashi Y |title=Autoantibodies and cell-mediated autoimmunity to NMDA-type GluRepsilon2 in patients with Rasmussen's encephalitis (RE) and chronic progressive epilepsia partialis continua |journal=Epilepsia |volume=46 |issue=Suppl 5 |pages=152–158 |year=2005 |pmid=15987271 |doi=10.1111/j.1528-1167.2005.01024.x |author-separator=, |author2=Mori H |author3=Mishina M |display-authors=3 |last4=Watanabe |first4=Masahiko |last5=Kondo |first5=Naomi |last6=Shimomura |first6=Jiro |last7=Kubota |first7=Yuko |last8=Matsuda |first8=Kazumi |last9=Fukushima |first9=Katsuyuki}}</ref> There has also been some evidence that patients suffering from RE express auto-antibodies against alpha 7 subunit of the nicotinic acetylcholine receptor.<ref>{{cite journal|last=Watson|first=R|coauthors=Jepson, JE; Bermudez, I; Alexander, S; Hart, Y; McKnight, K; Roubertie, A; Fecto, F; Valmier, J; Sattelle, DB; Beeson, D; Vincent, A; Lang, B|title=Alpha7-acetylcholine receptor antibodies in two patients with Rasmussen encephalitis.|journal=Neurology|date=2005 Dec 13|volume=65|issue=11|pages=1802-4|pmid=16344526}}</ref> |
||
Rasmussen's encephalitis has been recorded with a [[neurovisceral]] [[porphyria]], [[acute intermittent porphyria]] <ref>Tziperman B, Garty BZ, Schoenfeld N, Hoffer V, Watemberg N, Lev D, Ganor Y, Levite M, Lerman-Sagie T. Acute intermittent porphyria, Rasmussen encephalitis, or both? J Child Neurol. 2007 Jan;22(1):99-105.</ref> and after ADEM (acute disseminated encephalomyelitis){{Citation needed|date=March 2010}}. |
Rasmussen's encephalitis has been recorded with a [[neurovisceral]] [[porphyria]], [[acute intermittent porphyria]] <ref>Tziperman B, Garty BZ, Schoenfeld N, Hoffer V, Watemberg N, Lev D, Ganor Y, Levite M, Lerman-Sagie T. Acute intermittent porphyria, Rasmussen encephalitis, or both? J Child Neurol. 2007 Jan;22(1):99-105.</ref> and after ADEM (acute disseminated encephalomyelitis){{Citation needed|date=March 2010}}. |
||
Revision as of 14:36, 9 December 2012
| Rasmussen syndrome | |
|---|---|
| Specialty | Neurology |
Rasmussen's encephalitis, also known as chronic focal encephalitis (CFE), is a rare inflammatory neurological disorder, characterized by frequent and severe seizures, loss of motor skills and speech, hemiparesis (paralysis on one side of the body), encephalitis (inflammation of the brain), and dementia. The disorder, which affects a single cerebral hemisphere, generally occurs in children under the age of 15.
Causes and pathophysiology
In Rasmussen’s encephalitis, there is chronic inflammation of the brain, with infiltration of T lymphocytes into the brain tissue. This affects only one cerebral hemisphere, either the left or the right. This inflammation causes permanent damage to the cells of the brain, leading to atrophy of the hemisphere; the epilepsy that this causes may itself contribute to the brain damage.
The cause of the inflammation is not known: infection by a virus has been suggested, but the evidence for this is inconclusive.[1] In the 1990s it was suggested that auto-antibodies against the glutamate receptor GluR3 were important in causing the disease,[2] but this is no longer thought to be the case.[3] However, more recent studies report the presence of autoantibodies against the NMDA-type glutamate receptor subunit GluRepsilon2 (anti-NR2A antibodies) in a subset of patients with Rasmussen's encephalitis.[4] There has also been some evidence that patients suffering from RE express auto-antibodies against alpha 7 subunit of the nicotinic acetylcholine receptor.[5]
Rasmussen's encephalitis has been recorded with a neurovisceral porphyria, acute intermittent porphyria [6] and after ADEM (acute disseminated encephalomyelitis)[citation needed].
Clinical features
The condition mostly affects children, with an average age of 6 years. However, one in ten people with the condition develops it in adulthood.
There are two main stages, sometimes preceded by a 'prodromal stage' of a few months. In the acute stage, lasting four to eight months, the inflammation is active and the symptoms become progressively worse. These include weakness of one side of the body (hemiparesis), loss of vision for one side of the visual field (hemianopia), and cognitive difficulties (affecting learning, memory or language, for example). Epileptic seizures are also a major part of the illness, although these are often partial. Focal motor seizures or epilepsia partialis continua are particularly common, and may be very difficult to control with drugs.
In the chronic or residual stage, the inflammation is no longer active, but the sufferer is left with some or all of the symptoms because of the damage that the inflammation has caused. In the long term, most patients are left with some epilepsy, paralysis and cognitive problems, but the severity varies considerably.[1]
Investigations
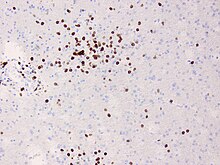
The diagnosis may be made on the clinical features alone, along with tests to rule out other possible causes. An EEG will usually show the electrical features of epilepsy and slowing of brain activity in the affected hemisphere, and MRI brain scans will show gradual shrinkage of the affected hemisphere with signs of inflammation or scarring. Brain biopsy can provide very strong confirmation of the diagnosis, but this is not always necessary.

A. December 2008, the patient was presented with headache and epilepsia partialis continua. There are lesions with local brain swelling in the right parietal and occipital lobes and right cerebellar hemisphere.
B. April 2009, the same patient, now she is comatose with epilepsia partialis continua. There is progression of the encephalitis - the left cerebral hemisphere has been involved with severe brain swelling and shift of the midline structures.
Treatment
During the acute stage, treatment is aimed at reducing the inflammation. As in other inflammatory diseases, steroids may be used first of all, either as a short course of high-dose treatment, or in a lower dose for long-term treatment. Intravenous immunoglobulin is also effective both in the short term and in the long term, particularly in adults where it has been proposed as first-line treatment.[7] Other similar treatments include plasmapheresis and tacrolimus, though there is less evidence for these. None of these treatments can prevent permanent disability from developing.
During the residual stage of the illness when there is no longer active inflammation, treatment is aimed at improving the remaining symptoms. Standard anti-epileptic drugs are usually ineffective in controlling seizures, and it may be necessary to surgically remove or disconnect the affected cerebral hemisphere, in an operation called hemispherectomy. This usually results in further weakness, hemianopsia and cognitive problems, but the other side of the brain may be able to take over some of the function, particularly in young children. The operation may not be advisable if the left hemisphere is affected, since this hemisphere contains most of the parts of the brain that control language. However, hemispherectomy is often very effective in reducing seizures.[1]
Name of the disease
It is named for the neurosurgeon Theodore Rasmussen (1910–2002), who succeeded Wilder Penfield as head of the Montreal Neurological Institute, and served as Neurosurgeon-in-Chief at the Royal Victoria Hospital.[8][9]
Foundations
The Hemispherectomy Foundation was formed in 2008 to assist families with children who have Rasmussen's Encephalitis and other conditions that require hemispherectomy.[10]
The RE Children's Project was founded in 2010 to increase awareness of Rasmussen's Encephalitis. Its primary purpose is to support scientific research directed toward finding a cure for this disease.
References
- ^ a b c Bien, CG (2005). "Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: a European consensus statement". Brain. 128 (Pt 3): 454–471. doi:10.1093/brain/awh415. PMID 15689357. 15689357.
{{cite journal}}: Invalid|display-authors=1(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Rogers SW; Andrews PI; Gahring LC; et al. (1994). "Autoantibodies to glutamate receptor GluR3 in Rasmussen's encephalitis". Science. 265 (5172): 648–51. doi:10.1126/science.8036512. PMID 8036512.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Watson R; Jiang Y; Bermudez I; et al. (2004). "Absence of antibodies to glutamate receptor type 3 (GluR3) in Rasmussen encephalitis". Neurology. 63 (1): 43–50. doi:10.1212/01.WNL.0000132651.66689.0F. PMID 15249609.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Takahashi Y; Mori H; Mishina M; et al. (2005). "Autoantibodies and cell-mediated autoimmunity to NMDA-type GluRepsilon2 in patients with Rasmussen's encephalitis (RE) and chronic progressive epilepsia partialis continua". Epilepsia. 46 (Suppl 5): 152–158. doi:10.1111/j.1528-1167.2005.01024.x. PMID 15987271.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Watson, R (2005 Dec 13). "Alpha7-acetylcholine receptor antibodies in two patients with Rasmussen encephalitis". Neurology. 65 (11): 1802–4. PMID 16344526.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Tziperman B, Garty BZ, Schoenfeld N, Hoffer V, Watemberg N, Lev D, Ganor Y, Levite M, Lerman-Sagie T. Acute intermittent porphyria, Rasmussen encephalitis, or both? J Child Neurol. 2007 Jan;22(1):99-105.
- ^ Hart, YM (1994). "Medical treatment of Rasmussen syndrome (chronic encephalitis and epilepsy): effect of high-dose steroids or immunoglobulins in 19 patients". Neurology. 44 (6): 1030–1036. doi:10.1212/WNL.44.6.1030. PMID 8208394. 8208394.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ synd/2828 at Who Named It?
- ^ Rasmussen T, Olszewski J, Lloyd-Smith D (1958). "Focal seizures due to chronic localized encephalitis". Neurology. 8 (6): 435–45. doi:10.1212/WNL.8.6.435. PMID 13566382.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "The Community News". Retrieved 2009-02-25. [dead link]
External links
- Rasmussen at NINDS (Note: parts of this entry were copied from this Public Domain source.)
