Neurosyphilis
| Neurosyphilis | |
|---|---|
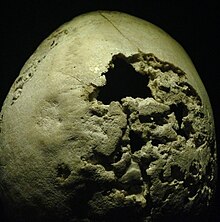 | |
| Section of human skull damaged by late stages of neurosyphilis. | |
| Specialty | Infectious diseases |
Neurosyphilis is an infection of the brain or spinal cord caused by the spirochete Treponema pallidum. It usually occurs in people who have had chronic, untreated syphilis, usually about 10 to 20 years after first infection[1] and develops in about 25%–40% of those who are not treated.[2] The United States' Centers for Disease Control and Prevention (CDC) advises that neurosyphilis can occur at any stage of a syphilis infection.[3]
Signs and symptoms
Neurosyphilis has four different forms: asymptomatic, meningovascular, tabes dorsalis, and general paresis.[4] In rare instances, active neurosyphilis can mimic Alzheimer's disease.[2]
Symptoms of neurosyphilis include the following:[1][4]
- Abnormal gait
- Blindness
- Confusion, disorientation
- Sudden personality changes
- Changes in mental stability
- Dementia
- Depression
- Headache
- Fecal and urinary incontinence
- Irritability
- Memory problems
- Mood disturbances
- Numbness in the toes, feet, or legs
- Poor concentration
- Psychosis[5]
- Seizures
- Neck stiffness
- Tremors
- Visual disturbances. There may be the sign of Argyll Robertson pupils, which are bilateral small pupils that constrict when the patient focuses on a near object but do not constrict when exposed to bright light.
- Muscle weakness
Upon further diagnostic workup, the following signs may be present:
- Abnormal reflexes
- Muscle atrophy
- Muscle contractions
Diagnosis
In addition to evaluation of any symptoms and signs, various blood tests can be done:[1]
- Venereal Disease Research Laboratory test (VDRL)
- Fluorescent treponemal antibody absorption (FTA-ABS)
- Rapid plasma reagin (RPR)
- Treponema pallidum particle agglutination assay (TPPA)
Also, it is important to test the cerebrospinal fluid for signs of syphilis.[1]
Additional tests to look for problems with the nervous system may include the following:[1]
- Cerebral angiogram
- Head CT scan
- Lumbar puncture ("spinal tap") to acquire a sample for cerebrospinal fluid analysis
- MRI scan of the brain, brainstem, or spinal cord
Treatment
Penicillin is used to treat neurosyphilis; however, early diagnosis and treatment is critical.[2] Two examples of penicillin therapies include:[1]
- Aqueous penicillin G 3–4 million units every four hours for 10 to 14 days.
- One daily intramuscular injection and oral probenecid four times daily, both for 10 to 14 days.
Follow-up blood tests are generally performed at 3, 6, 12, 24, and 36 months to make sure the infection is gone.[1] Lumbar punctures for CSF fluid analysis are generally performed every 6 months.
Neurosyphilis was almost at the point being unheard of in the United States after penicillin therapy was introduced.[6] However, concurrent infection of T. pallidum with human immunodeficiency virus (HIV) has been found to affect the course of syphilis. Syphilis can lie dormant for 10 to 20 years before progressing to neurosyphilis, but HIV may accelerate the rate of the progress. Also, infection with HIV has been found to cause penicillin therapy to fail more often. Therefore, neurosyphilis has once again been prevalent in societies with high HIV rates[2] and limited access to penicillin.[7] Blood testing for syphilis was once required in order to obtain a marriage license in most U.S. states, but that requirement has been discontinued by all 50 states over recent years, also contributing to the spread of the disease.
References
- ^ a b c d e f g "Neurosyphilis". A.D.A.M. Medical Encyclopedia on PubMed Health. Reviewed by David C. Dugdale, Jatin M. Vyas, David Zieve. 6 October 2012. Retrieved 2014-10-23.
{{cite web}}: CS1 maint: others (link) - ^ a b c d Mehrabian, S.; Raycheva, M.; Traykova, M.; Stankova, T.; Penev, L.; Grigorova, O.; Traykov, L. (20 September 2012). "Neurosyphilis with dementia and bilateral hippocampal atrophy on brain magnetic resonance imaging". BMC Neurology. 12 (1): 96. doi:10.1186/1471-2377-12-96.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Syphilis CDC Fact Sheet". Centers for Disease Control and Prevention. 4 September 2012. Retrieved 2014-10-23.
- ^ a b Kennard, Christine (10 September 2014). "Neurosyphilis". About.com. Retrieved 2014-10-23.
- ^ Murray, E. D.; Buttner, N.; Price, B. H. (2012). "Depression and Psychosis in Neurological Practice". In Bradley, W. G.; Daroff, R. B.; Fenichel, G. M.; et al. (eds.). Bradley's Neurology in Clinical Practice: Expert Consult. Vol. 1 (6 ed.). Philadelphia, PA: Elsevier/Saunders. pp. 101–102. ISBN 978-1-4377-0434-1.
- ^ Musher, D. M. (1 June 1991). "Syphilis, Neurosyphilis, Penicillin, and AIDS". Journal of Infectious Diseases. 163 (6): 1201–1206. doi:10.1093/infdis/163.6.1201.
- ^ Gordon, S. M.; Eaton, M. E.; George, R.; Larsen, S.; Lukeheart, S. A.; Kuypers, J.; Marra, C. M.; Thompson, S. (1 December 1994). "The Response of Symptomatic Neurosyphilis to High Dose Intravenous Penicillin G in Patients Human Immunodeficiency Infection". The New England Journal of Medicine. 331 (22): 1469–1473. doi:10.1056/nejm199412013312201. PMID 7969296. Retrieved 2014-10-23.
