Suprascapular notch
| Suprascapular notch | |
|---|---|
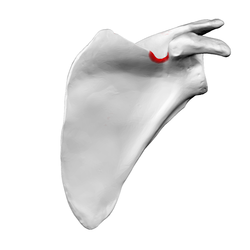 Costal surface of left scapula. Suprascapular notch shown in red. | |
 Costal surface of left scapula. Suprascapular notch visible in the red square. | |
| Details | |
| Identifiers | |
| Latin | Incisura scapulae |
| TA98 | A02.4.01.015 |
| TA2 | 1158 |
| FMA | 23236 |
| Anatomical terms of bone | |
The suprascapular notch (or scapular notch) is a notch in the superior border of the scapula, just lateral to the base of the coracoid process. It forms the entrance site into the suprascapular canal.[1]
Structure
This notch is converted into a foramen by the suprascapular ligament, and serves for the passage of the suprascapular nerve;[2] sometimes the ligament is ossified. The suprascapular vessels varies in number as well as in their course as they run at the suprascapular notch site. The suprascapular artery pass above the suprascapular ligament in most cases. The suprascapular vein been found to pass above the suprascapular ligament as well as passing through the suprascapular notch.[3][1]
Types
Two main classification systems exists with others being modified approaches of the same principle.
Typing based on subjective observation of the suprascapular notch shape. Introduced by Hrdicka 1942 and modified by Rengachary et al. 1979. There are six basic types of scapular notch:
- Type I: Notch is absent. The superior border forms a wide depression from the medial angle to the coracoid process.
- Type II: Notch is a blunted V-shape occupying the middle third of the superior border.
- Type III: Notch is U-shaped with nearly parallel margins.
- Type IV: Notch is V-shaped and very small. A shallow groove is frequently formed for the suprascapular nerve adjacent to the notch.
- Type V: Notch is minimal and U-shaped with a partially ossified ligament.
- Type VI: Notch is a foramen as the ligament is completely ossified.[4]
Typing based on parametric measurements of depth to upper width ratio of the suprascapular notch introduced by Natsis et al. 2007 and modified by Polguj et al. 2011. There are five basic types of scapular notch:
- Type I: Depth larger than upper width.
- Type II: Depth equal to upper width.
- Type III: Depth is smaller than upper width.
- Type IV: Notch is a foramen.
- Type V: Discrete notch.
The second method of suprascapular notch typing yields more practical approach in clinical diagnosis of the suprascapular nerve entrapment.[5]
Clinical Relevance
As the suprascapular nerve passes through the suprascapular notch, it is a common site of entrapment for the nerve.[1][6][7]
Suprascapular notch stenosis is a narrowing of the notch internal space that can potentially compress the suprascapular nerve leading to suprascapular nerve entrapment. Al-Redouan et al. 2020 predicted the morphological pattern of the suprascapular notch stenosis revealing higher incidence in the discrete notch (Type V according to the parametric measurements typing system). Two main suprascapular stenosis pattern:[5]
- Vertical stenosis. Treated surgically by cutting the suprascapular ligament (ligamentectomy).
- Horizontal stenosis. Treated surgically by trimming the notch borders (osteoplasty).
The suprascapular nerve predictably passes through the suprascapular notch, so it is a good place for a local nerve block of the entire nerve.[8][9]
Additional images
-
Left scapula. Suprascapular notch shown in red.
-
Animation. Suprascapular notch shown in red.
-
Left scapula. Dorsal surface. (Sup. notch visible at top center.)
-
Costal surface of left scapula. Suprascapular notch labeled at top center.
See also
References
- ^ a b c Al-Redouan, Azzat; Holding, Keiv; Kachlik, David (2021). ""Suprascapular canal": Anatomical and topographical description and its clinical implication in entrapment syndrome". Annals of Anatomy. 233: 151593. doi:10.1016/j.aanat.2020.151593. PMID 32898658.
- ^ Nathan, Jay K.; McGillicuddy, John E. (2015-01-01), Tubbs, R. Shane; Rizk, Elias; Shoja, Mohammadali M.; Loukas, Marios (eds.), "Chapter 38 - Anatomy of the Ventral Rami, Upper Trunk, and Its Divisions and Branches", Nerves and Nerve Injuries, San Diego: Academic Press, pp. 527–535, doi:10.1016/b978-0-12-410390-0.00040-8, ISBN 978-0-12-410390-0, retrieved 2020-10-19
- ^ Polguj, Michał; Rożniecki, Jacek; Sibiński, Marcin; Grzegorzewski, Andrzej; Majos, Agata; Topol, Mirosław (2015). "The variable morphology of suprascapular nerve and vessels at suprascapular notch: a proposal for classification and its potential clinical implications". Knee Surg Sports Traumatol Arthrosc. 23 (5): 1542–1548. doi:10.1007/s00167-014-2937-1. PMC 4555201. PMID 24633009.
- ^ White, Tim D.; Black, Michael T.; Folkens, Pieter A. (2012-01-01), White, Tim D.; Black, Michael T.; Folkens, Pieter A. (eds.), "Chapter 8 - Shoulder Girdle: Clavicle and Scapula", Human Osteology (Third Edition), San Diego: Academic Press, pp. 161–174, doi:10.1016/b978-0-12-374134-9.50008-8, ISBN 978-0-12-374134-9, retrieved 2020-10-19
- ^ a b Al-Redouan, Azzat; Hudak, Radovan; Nanka, Ondrej; Kachlik, David (2020). "The morphological stenosis pattern of the suprascapular notch is revealed yielding higher incidence in the discrete type and elucidating the inevitability of osteoplasty in horizontally oriented stenosis". Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-020-06168-1. PMID 32712687.
- ^ Preston, David C.; Shapiro, Barbara E. (2013-01-01), Preston, David C.; Shapiro, Barbara E. (eds.), "31 - Proximal Neuropathies of the Shoulder and Arm", Electromyography and Neuromuscular Disorders (Third Edition), London: W.B. Saunders, pp. 487–500, doi:10.1016/b978-1-4557-2672-1.00031-3, ISBN 978-1-4557-2672-1, retrieved 2020-10-19
- ^ Bouche, P. (2013-01-01), Said, Gérard; Krarup, Christian (eds.), "Chapter 19 - Compression and entrapment neuropathies", Handbook of Clinical Neurology, Peripheral Nerve Disorders, 115, Elsevier: 311–366, doi:10.1016/b978-0-444-52902-2.00019-9, PMID 23931789, retrieved 2020-10-19
- ^ Wilkinson, Laura J. "Defunct DOI". Crossref. doi:10.1016/b978-032304184-3.50050-9. Retrieved 2020-10-19.
- ^ Molloy, Robert E. (2005-01-01), Benzon, Honorio T.; Raja, Srinivasa N.; Molloy, Robert E.; Liu, Spencer S. (eds.), "Chapter 75 - Truncal Blocks: Intercostal, Paravertebral, Interpleural, Suprascapular, Ilioinguinal, and Iliohypogastric Nerve Blocks", Essentials of Pain Medicine and Regional Anesthesia (Second Edition), Philadelphia: Churchill Livingstone, pp. 636–644, doi:10.1016/b978-0-443-06651-1.50079-4, ISBN 978-0-443-06651-1, retrieved 2020-10-19
![]() This article incorporates text in the public domain from page 204 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 204 of the 20th edition of Gray's Anatomy (1918)
- Habermeyer, Peter; Magosch, Petra; Lichtenberg, Sven (2006). Classifications and Scores of the Shoulder. Springer. ISBN 978-3-540-24350-2. LCCN 2005938553.
- Rengachary, S. S.; Burr, D.; Lucas, S.; Hassanein, K. M.; Mohn, M. P.; Matzke, H. (1979). "Suprascapular entrapment neuropathy: a clinical, anatomical, and comparative study". Neurosurgery. 5 (4): 447–451. doi:10.1227/00006123-197910000-00007. PMID 534049.
- Hrdicka, Ales (1942). "The scapula: visual observations". American Journal of Physical Anthropology. 29: 73–94. doi:10.1002/ajpa.1330290107.
- Natsis, K; Totlis, T; Tsikaras, P; Appell, H J; Skandalakis, P; Koebke, J (2007). "Proposal for classification of the suprascapular notch: a study on 423 dried scapulas". Clinical Anatomy. 20 (2): 135–139. doi:10.1002/ca.20318. PMID 16838269.
- Polguj, Michał; Jędrzejewski, Kazimierz; Podgórski, Michał; Topol, Mirosław (2011). "Morphometric study of the suprascapular notch: proposal of classification". Surgical and Radiologic Anatomy. 33 (9): 781–787. doi:10.1007/s00276-011-0821-y. PMID 21590338.




