Polar surface area
This article includes a list of general references, but it lacks sufficient corresponding inline citations. (December 2017) |
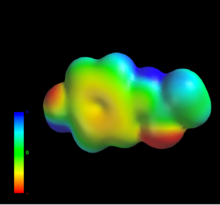
The polar surface area (PSA) or topological polar surface area (TPSA) of a molecule is defined as the surface sum over all polar atoms or molecules, primarily oxygen and nitrogen, also including their attached hydrogen atoms.
PSA is a commonly used medicinal chemistry metric for the optimization of a drug's ability to permeate cells. Molecules with a polar surface area of greater than 140 angstroms squared (Å2) tend to be poor at permeating cell membranes.[1] For molecules to penetrate the blood–brain barrier (and thus act on receptors in the central nervous system), a PSA less than 90 Å2 is usually needed.[2]
TPSA is a valuable tool in drug discovery and development. By analyzing a drug candidate's TPSA, scientists can predict its potential for oral bioavailability and ability to reach target sites within the body. This prediction hinges on a drug's ability to permeate biological barriers.
Permeating these barriers, such as the Blood-Brain Barrier (BBB), the Placental Barrier (PB), and the Blood-Mammary Barrier (BM), is crucial for many drugs to reach their intended targets.
The BBB, for example, protects the brain from harmful substances. Drugs with a lower TPSA (generally below 90 Ų) tend to permeate the BBB more easily, allowing them to reach the brain and exert their therapeutic effects (Shityakov et al[3]., 2013).
Similarly, for drugs intended to treat the fetus, a lower TPSA (below 60 Ų) is preferred to ensure they can pass through the placenta (Augustiño-Roubina[4] et al., 2019).
Breastfeeding mothers also need consideration. Here, an optimal TPSA for a drug is around 60-80 Ų to allow it to reach the breast tissue for milk production, while drugs exceeding 90 Ų are less likely to permeate the Blood-Mammary Barrier.[5]
See also
[edit]References
[edit]- ^ Pajouhesh H, Lenz GR (Oct 2005). "Medicinal Chemical Properties of Successful Central Nervous System Drugs". NeuroRx. 2 (4): 541–553. doi:10.1602/neurorx.2.4.541. PMC 1201314. PMID 16489364.
- ^ Hitchcock SA, Pennington LD (May 2006). "Structure - Brain Exposure Relationships". J. Med. Chem. 49 (26): 7559–7583. doi:10.1021/jm060642i. PMID 17181137.
- ^ Shityakov, Sergey; Neuhaus, Winfried; Dandekar, Thomas; Förster, Carola (2013). "Analysing molecular polar surface descriptors to predict blood-brain barrier permeation". International Journal of Computational Biology and Drug Design. 6 (1–2): 146–156. doi:10.1504/IJCBDD.2013.052195. ISSN 1756-0756. PMID 23428480.
- ^ Hester, Gabrielle; Lang, Tom; Madsen, Laura; Tambyraja, Rabindra; Zenker, Paul (January 2019). "Timely Data for Targeted Quality Improvement Interventions: Use of a Visual Analytics Dashboard for Bronchiolitis". Applied Clinical Informatics. 10 (1): 168–174. doi:10.1055/s-0039-1679868. ISSN 1869-0327. PMC 6402943. PMID 30841007.
- ^ "Δραστική: PARACETAMOL". farmako.net. Retrieved 2024-04-10.
Literature
[edit]- Pajouhesh, Hassan; Lenz, George R (2005). "Medicinal chemical properties of successful central nervous system drugs". NeuroRx. 2 (4): 541–553. doi:10.1602/neurorx.2.4.541. PMC 1201314. PMID 16489364.
- Clark, David E (1999). "Rapid calculation of polar molecular surface area and its application to the prediction of transport phenomena. 1. Prediction of intestinal absorption". Journal of Pharmaceutical Sciences. 88 (8): 807–14. doi:10.1021/js9804011. PMID 10430547.
- Palm, Katrin; Stenberg, Patric; Luthman, Kristina; Artursson1, Per (1997). "Polar molecular surface properties predict the intestinal absorption of drugs in humans". Pharmaceutical Research. 14 (5): 568–71. doi:10.1023/A:1012188625088. PMID 9165525. S2CID 7178582.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - Ertl, Peter; Rohde, Bernhard; Selzer, Paul (2000). "Fast Calculation of Molecular Polar Surface Area as a Sum of Fragment-Based Contributions and Its Application to the Prediction of Drug Transport Properties". Journal of Medicinal Chemistry. 43 (20): 3714–3717. doi:10.1021/jm000942e. PMID 11020286.
- Ertl, P. Polar Surface Area, in Molecular Drug Properties, R. Mannhold (ed), Wiley-VCH, pp. 111–126, 2007
- Shityakov, Sergey; Neuhaus, Winfried; Dandekar, Thomas; Förster, Carola (2013). "Analysing molecular polar surface descriptors to predict blood-brain barrier permeation". International Journal of Computational Biology and Drug Design. 6 (1–2): 146–56. doi:10.1504/IJCBDD.2013.052195. PMID 23428480.
External links
[edit]
