Neonatal resuscitation: Difference between revisions
m →Training and Certification: added more info about NRP |
Added outcomes section |
||
| Line 46: | Line 46: | ||
* Ceasing [[oropharyngeal]] and [[nasopharyngeal]] [[suctioning]] for newborns with clear or meconium-stained amniotic fluid. |
* Ceasing [[oropharyngeal]] and [[nasopharyngeal]] [[suctioning]] for newborns with clear or meconium-stained amniotic fluid. |
||
* Newborns who receive [[Positive pressure ventilation|Positive Pressure Ventilation]] (PPV) for either ineffective respirations or bradycardia should not also receive initial sustained inflations greater than 5 seconds. |
* Newborns who receive [[Positive pressure ventilation|Positive Pressure Ventilation]] (PPV) for either ineffective respirations or bradycardia should not also receive initial sustained inflations greater than 5 seconds. |
||
* Intravenous [[epinephrine]] |
* Intravenous [[epinephrine]] is administered if heart rate does not increase to 60 beats per minute after ventilation and [[chest compressions]] have been optimized. |
||
* [[umbilical venous catheterization]] should be the primary vascular access route during delivery.<ref name=":2" /> |
* [[umbilical venous catheterization]] should be the primary vascular access route during delivery.<ref name=":2" /> |
||
| Line 55: | Line 55: | ||
* Monitoring of heart rate is the best indicator of response to resuscitation efforts.<ref name=":0" /> |
* Monitoring of heart rate is the best indicator of response to resuscitation efforts.<ref name=":0" /> |
||
* Epinephrine should be administered [[intravenously]] if response to chest compressions is poor.<ref name=":1" /> |
* Epinephrine should be administered [[intravenously]] if response to chest compressions is poor.<ref name=":1" /> |
||
== Outcomes == |
|||
Most neonatal deaths (roughly 75%) after resuscitation occur within the first week, but the vast majority occur within 24 hours.<ref name=":3">{{Cite journal|last=Shikuku|first=Duncan N.|last2=Milimo|first2=Benson|last3=Ayebare|first3=Elizabeth|last4=Gisore|first4=Peter|last5=Nalwadda|first5=Gorrette|date=2018-05-15|title=Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya: a direct observation study|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5953400/|journal=BMC Pediatrics|volume=18|pages=167|doi=10.1186/s12887-018-1127-6|issn=1471-2431|pmc=5953400|pmid=29764391}}</ref> This statistic is based on a [[Average|mean]] [[Apgar score|Apgar]] score if 5.9, which is considered intermediate. More data is needed to understand outcomes for more severe patients. Outcomes after resuscitation for neonates vary widely based on many factors. One study in [[Norway]] analyzed 15 [[Peer review|peer-reviewed]] published articles and found that high-income countries have a mortality rate as high as 10% while low-income countries have a mortality rate as high as 28%.<ref>{{Cite journal|last=Boldingh|first=Anne Marthe|last2=Solevåg|first2=Anne Lee|last3=Nakstad|first3=Britt|date=2018-05-28|title=Outcomes following neonatal cardiopulmonary resuscitation|url=https://tidsskriftet.no/en/2018/05/oversiktsartikkel/outcomes-following-neonatal-cardiopulmonary-resuscitation|journal=Tidsskrift for Den norske legeforening|language=en|doi=10.4045/tidsskr.17.0358|issn=0029-2001}}</ref> One major factor that improved survival was how quickly medical responders were able to intervene, noting that the first minutes are critical.<ref name=":3" /> |
|||
Currently, it is the gold standard to place neonates on a cooling blanket for 72 hours to achieve [[Targeted temperature management|total body cooling]]. This is done in order to minimize brain swelling. After cooling is achieved, an MRI is obtained roughly 1 week after [[Hypoxia (medical)|hypoxic brain injury]] in order to classify the severity of brain damage. However, one study found that there was no significant correlation between MRI findings and developmental delay up to 2 years of life.<ref>{{Cite journal|last=Rusli|first=Emilia Rosniza Mohammed|last2=Ismail|first2=Juriza|last3=Wei|first3=Wong Saw|last4=Ishak|first4=Shareena|last5=Jaafar|first5=Rohana|last6=Zaki|first6=Faizah Mohd|date=2019|title=Neonatal hypoxic encephalopathy: Correlation between post-cooling brain MRI findings and 2 years neurodevelopmental outcome|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6958878/|journal=The Indian Journal of Radiology & Imaging|volume=29|issue=4|pages=350–355|doi=10.4103/ijri.IJRI_62_19|issn=0971-3026|pmc=6958878|pmid=31949335}}</ref> |
|||
==References== |
==References== |
||
{{reflist}} |
{{reflist}} |
||
Revision as of 01:47, 11 November 2021
| Neonatal resuscitation | |
|---|---|
 | |
| Specialty | neonatology |
| ICD-10-PCS | P29.81 |
| Other codes | P28.81 |
| MedlinePlus | https://medlineplus.gov/ency/article/000011.htm |
| eMedicine | https://emedicine.medscape.com/article/977002-overview |
| CPT | 99465 |
Neonatal resuscitation also known as newborn resuscitation is an emergency procedure focused on supporting the approximately 10%[1] of newborn children who do not readily begin breathing, putting them at risk of irreversible organ injury and death. Through positive airway pressure, and in severe cases chest compressions, medical personnel can often stimulate neonates to begin breathing on their own, with attendant normalization of heart rate. [2]
About a quarter of all neonatal deaths globally are caused by birth asphyxia.[3] This dangerous condition of oxygen deprivation may begin before birth, for example if the umbilical cord, which supplies oxygen throughout fetal development, is compressed or tears during delivery. Depending on how quickly and successfully the infant is resuscitated, hypoxic damage can occur to most of the infant's organs (heart, lungs, liver, gut, kidneys). One serious complication is a brain injury known as neonatal hypoxic-ischemic encephalopathy.
The International Liaison Committee on Resuscitation (ILCOR) has published Consensus on science and treatment recommendations for neonatal resuscitation in 2000, 2005 and 2010. Traditionally, newborn children have been resuscitated using mechanical ventilation with 100% oxygen, but there has since the 1980s increasingly been debated whether newborn infants with asphyxia should be resuscitated with 100% oxygen or normal air, and notably Ola Didrik Saugstad has been a major advocate of using normal air.[4][5] It has been demonstrated that high concentrations of oxygen lead to generation of oxygen free radicals, which have a role in reperfusion injury after asphyxia.[6] Clinical trial evidence suggests that resuscitation using air probably reduces the risk of death[7] and the 2010 ILCOR guidelines recommend the use of normal air rather than 100% oxygen.[8]
In 2020, the International Liaison Committee on Resuscitation (ILCOR) published its 4th and most recent recommendations for newborn life support. The committee reviewed 8 major topics, including anticipation and preparation, initial assessment and intervention, physiologic monitoring and feedback devices, ventilation and oxygenation, circulatory support, drug and fluid administration, prognostication during CPR, and post-resuscitation care.[9]
For preterm infants, there may be little or no difference in risk of death or neurodevelopment disability when higher concentrations of oxygen are used compared to lower concentrations but the evidence from clinical trials is still relatively uncertain.[10]
Training and Certification
The most widely known training/certification for neonatal resuscitation is the Neonatal Resuscitation Program (NRP).
- Neonatal Resuscitation Program - Started by the American Academy of Pediatrics, this course has been revised several times and is currently offered to anyone who participates in neonatal resuscitation including but not limited to: Nurses, Physicians, Respiratory Therapists, Certified Nursing Assistants, and others. The course is broken down into 11 sections and a final skills assessment. There are currently 4 million healthcare providers that are certified. It is estimated that roughly 200,000 healthcare providers take this course every year.[11]
- Pediatric Advanced Life Support (PALS) - This program is more general to all pediatric patients, but does provide some neonatal resuscitation training.
- On-the-job training.
Resuscitation Guidelines
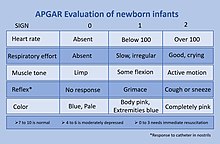
Initial evaluation of a newborn is done by obtaining an Apgar score, which gives the clinician a rough idea of the infants cardiovascular and neurologic condition at birth. A score of 7-10 at 5 minutes is normal, a score of 4 to 6 at 5 minutes is intermediate, and a score of 0-3 is considered low. It is important to understand that an Apgar score is not a diagnosis, it is merely a clinical finding.[12] If a newborns score is 0-3, then resuscitation efforts are initiated.
Neonatal resuscitation guidelines closely resemble those of the pediatric basic and advanced life support. The main differences in training include an emphasis on positive pressure ventilation (PPV), updated timings on ventilation assistance rates, and some differences in the cardiac arrest chain of survival.
Guidelines for neonatal resuscitation are assessed annually and are developed in collaboration with multiple organizations of numerous experts, including the American Academy of Pediatrics (AAP).
In 2020, the International Liaison Committee on Resuscitation (ILCOR) recommended the following changes to current resuscitation guidelines:
- Ceasing oropharyngeal and nasopharyngeal suctioning for newborns with clear or meconium-stained amniotic fluid.
- Newborns who receive Positive Pressure Ventilation (PPV) for either ineffective respirations or bradycardia should not also receive initial sustained inflations greater than 5 seconds.
- Intravenous epinephrine is administered if heart rate does not increase to 60 beats per minute after ventilation and chest compressions have been optimized.
- umbilical venous catheterization should be the primary vascular access route during delivery.[9]
While some guidelines do tend to change, certain elements of neonatal resuscitation have persisted. These include the following bulleted items.
- For uncomplicated term or preterm infants, delayed cord clamping is standard so that the child can immediately be placed in the mothers arms to be evaluated.[13]
- Supplemental oxygen is used judiciously.[14]
- Monitoring of heart rate is the best indicator of response to resuscitation efforts.[13]
- Epinephrine should be administered intravenously if response to chest compressions is poor.[14]
Outcomes
Most neonatal deaths (roughly 75%) after resuscitation occur within the first week, but the vast majority occur within 24 hours.[15] This statistic is based on a mean Apgar score if 5.9, which is considered intermediate. More data is needed to understand outcomes for more severe patients. Outcomes after resuscitation for neonates vary widely based on many factors. One study in Norway analyzed 15 peer-reviewed published articles and found that high-income countries have a mortality rate as high as 10% while low-income countries have a mortality rate as high as 28%.[16] One major factor that improved survival was how quickly medical responders were able to intervene, noting that the first minutes are critical.[15]
Currently, it is the gold standard to place neonates on a cooling blanket for 72 hours to achieve total body cooling. This is done in order to minimize brain swelling. After cooling is achieved, an MRI is obtained roughly 1 week after hypoxic brain injury in order to classify the severity of brain damage. However, one study found that there was no significant correlation between MRI findings and developmental delay up to 2 years of life.[17]
References
- ^ "Neonatal Resuscitation - Pediatrics". Merck Manuals Professional Edition. Retrieved 2019-11-13.
- ^ Johnson, Peter A.; Schmölzer, Georg M. (23 February 2020). "Heart Rate Assessment during Neonatal Resuscitation". Healthcare. 8 (1): 43. doi:10.3390/healthcare8010043. PMC 7151423. PMID 32102255.
- ^ Guidelines on basic newborn resuscitation, 2012, World Health Organization
- ^ Saugstad, OD; Rootwelt, T; Aalen, O (1998). "Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study". Pediatrics. 102 (1): e1. doi:10.1542/peds.102.1.e1. PMID 9651453.
- ^ Davis, PG; Tan, A; O'Donnell, CPF; Schulze, A (2004). "Resuscitation of newborn infants with 100% oxygen or air: a systematic review and meta-analysis". The Lancet. 364 (9442): 1329–1333. doi:10.1016/S0140-6736(04)17189-4. PMID 15474135. S2CID 24825982.
- ^ Kutzsche, S; Ilves, P; Kirkeby, OJ; Saugstad, OD (2001). "Hydrogen peroxide production in leukocytes during cerebral hypoxia and reoxygenation with 100% or 21% oxygen in newborn piglets". Pediatric Research. 49 (6): 834–842. doi:10.1203/00006450-200106000-00020. PMID 11385146.
- ^ Tan, A; Schulze, A; O'Donnell, CP; Davis, PG (18 April 2005). "Air versus oxygen for resuscitation of infants at birth". The Cochrane Database of Systematic Reviews (2): CD002273. doi:10.1002/14651858.CD002273.pub3. PMC 7017642. PMID 15846632.
- ^ ILCOR Neonatal Resuscitation Guidelines 2010
- ^ a b Wyckoff, Myra H.; Wyllie, Jonathan; Aziz, Khalid; de Almeida, Maria Fernanda; Fabres, Jorge; Fawke, Joe; Guinsburg, Ruth; Hosono, Shigeharu; Isayama, Tetsuya; Kapadia, Vishal S.; Kim, Han-Suk (2020-10-20). "Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations". Circulation. 142 (16_suppl_1): S185–S221. doi:10.1161/CIR.0000000000000895.
- ^ Lui, K; Jones, LJ; Foster, JP; Davis, PG; Ching, SK; Oei, JL; Osborn, DA (4 May 2018). "Lower versus higher oxygen concentrations titrated to target oxygen saturations during resuscitation of preterm infants at birth". The Cochrane Database of Systematic Reviews. 5: CD010239. doi:10.1002/14651858.CD010239.pub2. PMC 6494481. PMID 29726010.
- ^ Heartbeat, Project (2019-03-13). "Who Can Benefit from a Neonatal Resuscitation Program? | NRP Training". Project Heartbeat. Retrieved 2021-11-11.
- ^ "Neonatal Resuscitation - Pediatrics". Merck Manuals Professional Edition. Retrieved 2021-11-09.
- ^ a b Aziz, Khalid; Lee, Chair; Henry C.; Escobedo, Marilyn B.; Hoover, Amber V.; Kamath-Rayne, Beena D.; Kapadia, Vishal S.; Magid, David J.; Niermeyer, Susan; Schmölzer, Georg M.; Szyld, Edgardo; Weiner, Gary M. (2021-01-01). "Part 5: Neonatal Resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Pediatrics. 147 (Supplement 1). doi:10.1542/peds.2020-038505E. ISSN 0031-4005.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Aziz, Khalid; Lee, Chair; Henry C.; Escobedo, Marilyn B.; Hoover, Amber V.; Kamath-Rayne, Beena D.; Kapadia, Vishal S.; Magid, David J.; Niermeyer, Susan; Schmölzer, Georg M.; Szyld, Edgardo; Weiner, Gary M. (2021-01-01). "Part 5: Neonatal Resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Pediatrics. 147 (Supplement 1). doi:10.1542/peds.2020-038505E. ISSN 0031-4005.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Shikuku, Duncan N.; Milimo, Benson; Ayebare, Elizabeth; Gisore, Peter; Nalwadda, Gorrette (2018-05-15). "Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya: a direct observation study". BMC Pediatrics. 18: 167. doi:10.1186/s12887-018-1127-6. ISSN 1471-2431. PMC 5953400. PMID 29764391.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Boldingh, Anne Marthe; Solevåg, Anne Lee; Nakstad, Britt (2018-05-28). "Outcomes following neonatal cardiopulmonary resuscitation". Tidsskrift for Den norske legeforening. doi:10.4045/tidsskr.17.0358. ISSN 0029-2001.
- ^ Rusli, Emilia Rosniza Mohammed; Ismail, Juriza; Wei, Wong Saw; Ishak, Shareena; Jaafar, Rohana; Zaki, Faizah Mohd (2019). "Neonatal hypoxic encephalopathy: Correlation between post-cooling brain MRI findings and 2 years neurodevelopmental outcome". The Indian Journal of Radiology & Imaging. 29 (4): 350–355. doi:10.4103/ijri.IJRI_62_19. ISSN 0971-3026. PMC 6958878. PMID 31949335.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
