Schistosoma bovis: Difference between revisions
ShortDescBot (talk | contribs) ShortDescBot adding short description "Species of fluke" |
+==Gene expression==, moonlighting protein, one of few known outside bacteria, from Henderson & Martin 2011. "Pigs" failed verification & are not ruminants. Less specific [[]] ⇨ sporocyst (Trematode). +'' Latin names. Typos. |
||
| Line 17: | Line 17: | ||
== Life cycle == |
== Life cycle == |
||
[[File:Schistosoma life cycle.svg|thumb|Schistosoma life cycle]] |
[[File:Schistosoma life cycle.svg|thumb|Schistosoma life cycle]] |
||
''Schistosoma bovis'' infects two hosts, namely [[ruminant]]s (cattle, goats, sheep, horses |
''Schistosoma bovis'' infects two hosts, namely [[ruminant]]s (cattle, goats, sheep, horses and camels) and freshwater snails (''[[Bulinus]]'' sp. and ''[[Planorbarius]]'' sp.).<ref name=Mahmoud/>{{rp|392}} |
||
In water, its free swimming infective larval [[cercariae]] can burrow into the skin of its [[definite host]], the ruminant, upon contact. The cercariae enter the host's blood stream, and travel to the liver to mature into adult [[Trematoda|flukes]]. Adult flukes can coat themselves with host [[antigen]] thus avoiding detection by the host immune system. After a period of about three weeks the young flukes migrate to the [[mesenteric]] veins of the gut to copulate. The female fluke lays eggs, which migrate into the [[Lumen (anatomy)|lumen]] of the gut and leave the host upon defecation. In fresh water, the eggs hatch, forming free swimming [[miracidia]]. |
In water, its free swimming infective larval [[cercariae]] can burrow into the skin of its [[definite host]], the ruminant, upon contact. The cercariae enter the host's blood stream, and travel to the liver to mature into adult [[Trematoda|flukes]]. Adult flukes can coat themselves with host [[antigen]] thus avoiding detection by the host immune system. After a period of about three weeks the young flukes migrate to the [[mesenteric]] veins of the gut to copulate. The female fluke lays eggs, which migrate into the [[Lumen (anatomy)|lumen]] of the gut and leave the host upon defecation. In fresh water, the eggs hatch, forming free swimming [[miracidia]]. |
||
Miracidia penetrate into the [[intermediate host]], the freshwater snails<ref name="Black 2005">{{cite book | author=Black, J. | year=2005 | title=Microbiology: Principles and Explorations | publisher=Wiley, New York}}</ref> of the ''Bulinus'' spp., (e.g. ''[[Bulinus globosus|B. globosus]]'', ''[[Bulinus forskalii|B. forskalii]]'', ''[[Bulinus nyassanus|B. nyassanus]]'' and ''[[Bulinus truncatus|B. truncatus]]''), except in Spain,<ref name=Mahmoud/>{{rp|20}} Portugal and |
Miracidia penetrate into the [[intermediate host]], the freshwater snails<ref name="Black 2005">{{cite book | author=Black, J. | year=2005 | title=Microbiology: Principles and Explorations | publisher=Wiley, New York}}</ref> of the ''Bulinus'' spp., (e.g. ''[[Bulinus globosus|B. globosus]]'', ''[[Bulinus forskalii|B. forskalii]]'', ''[[Bulinus nyassanus|B. nyassanus]]'' and ''[[Bulinus truncatus|B. truncatus]]''), except in Spain,<ref name=Mahmoud/>{{rp|20}} Portugal and Morocco, where ''[[Planorbarius metidjensis]]'' can transmit.<ref>{{cite journal | vauthors = Mouahid A, Théron A | date = Dec 1987 | title = ''Schistosoma bovis'': variability of cercarial production as related to the snail hosts: ''Bulinus truncatus'', ''B. wright'' and ''Planorbarius metidjensis'' | journal = Int J Parasitol | volume = 17 | issue = 8| pages = 1431–4 | pmid = 3440697 | doi=10.1016/0020-7519(87)90078-6}}</ref> Inside the snail, the miracidium sheds its [[epithelium]], and develops into a mother [[sporocyst (Trematode)|sporocyst]]. After two weeks the mother begins forming daughter sporocysts. One month – or more with cooler ambient temperatures – after a miracidium has penetrated into the snail, hundreds to thousands of cercariae of the same sex begin to be released through special areas of the sporocyst wall.<ref name="Mahmoud" />{{rp|30}} The cercariae cycle from the top of the water to the bottom in search of a host. They can enter the host epithelium within minutes.<ref>{{cite book | author=Roberts, L. | author2=Janovy, J. | year=1996 | title=Foundations of Parasitology | edition=5th | publisher=Wm. C. Brown Publishers, Dubuque, Iowa}}</ref><ref name="Mahmoud" />{{rp|34}} |
||
== Geographical distribution == |
== Geographical distribution == |
||
| Line 41: | Line 41: | ||
=== Immunopathology === |
=== Immunopathology === |
||
The immune system responds to eggs in liver causing [[hypersensitivity]]; an immune response is necessary to prevent damage to [[hepatocyte]]s. The hosts' antibodies bind to the [[Tegument (helminth)|tegument]] of the schistosome but not for long since the tegument is shed every few hours. The schistosome can also take on host proteins. Schistomiasis can be divided into three phases; Within the haematobium group ''S. bovis'' and ''S. curassoni'' appear to be closely related: (1) the migratory phase lasting from penetration to maturity, (2) the acute phase which occurs when the schistosomes begin producing eggs, and (3) the chronic phase which occurs mainly in endemic areas.<ref name="Black 2005" /> |
The immune system responds to eggs in the liver causing [[hypersensitivity]]; an immune response is necessary to prevent damage to [[hepatocyte]]s. The hosts' antibodies bind to the [[Tegument (helminth)|tegument]] of the schistosome but not for long since the tegument is shed every few hours. The schistosome can also take on host proteins. Schistomiasis can be divided into three phases; Within the haematobium group ''S. bovis'' and ''S. curassoni'' appear to be closely related: (1) the migratory phase lasting from penetration to maturity, (2) the acute phase which occurs when the schistosomes begin producing eggs, and (3) the chronic phase which occurs mainly in endemic areas.<ref name="Black 2005" /> |
||
== Gene expression == |
|||
''S. bovis'' is one of the few non-bacterial species with a known [[moonlighting protein]]. [[Glyceraldehyde-3-phosphate dehydrogenase]] (GAPD) is also a common MP in bacteria.<ref name="Henderson-Martin-2011">{{cite book | editor-first1=Ulrich| editor-last1=Dobrindt | editor-first2=Jörg H. | editor-last2=Hacker | editor-first3=Catharina | editor-last3=Svanborg | last1=Henderson | first1=Brian | last2=Martin | first2=Andrew | title=Between Pathogenicity and Commensalism | chapter=Bacterial Moonlighting Proteins and Bacterial Virulence | publisher=[[Springer Berlin Heidelberg]] | publication-place=[[Berlin]], [[Heidelberg]] | year=2011 | isbn=978-3-642-36559-1 | issn=0070-217X | doi=10.1007/82_2011_188 | pages=155–213}}</ref> |
|||
== Treatment == |
== Treatment == |
||
Historically, [[antimonial]]s and [[trichlorphon]] |
Historically, [[antimonial]]s and [[trichlorphon]] were tested against visceral schistosome infection in cattle.<ref name=Reinecke>{{cite book | title=Veterinary helminthology | publisher=Butterworths | author=Reinecke, RK | year=1983 | location=Durban, SouthAfrica | chapter=Phylum plathelminthes}}</ref>{{rp|245–248, 265–273}} |
||
Antimony affects [[phosphofructokinase]] activity in ''Schistosoma'', [[hycanthone]] intercalates ''Schistosoma'' DNA and the organophosphorus metabolite [[dichlorvos]] inhibits [[acetylcholinesterase]], "but progressively less so in ''S. bovis''".<ref name=Mahmoud/>{{rp|44}} |
Antimony affects [[phosphofructokinase]] activity in ''Schistosoma'', [[hycanthone]] intercalates ''Schistosoma'' DNA and the organophosphorus metabolite [[dichlorvos]] inhibits [[acetylcholinesterase]], "but progressively less so in ''S. bovis''".<ref name=Mahmoud/>{{rp|44}} |
||
Revision as of 17:32, 19 January 2022
| Schistosoma bovis | |
|---|---|
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Animalia |
| Phylum: | Platyhelminthes |
| Class: | Trematoda |
| Order: | Diplostomida |
| Family: | Schistosomatidae |
| Genus: | Schistosoma |
| Species: | S. bovis
|
| Binomial name | |
| Schistosoma bovis (Bilharz, 1852)
| |
Schistosoma bovis is a two-host blood fluke, that causes intestinal schistosomiasis in ruminants in North Africa, Mediterranean Europe and the Middle East. S bovis is mostly transmitted by Bulinus freshwater snail species. It is one of nine haematobium group species and exists in the same geographical areas as Schistosoma haematobium, with which it can hybridise. S. bovis-S. haematobium hybrids can infect humans, and have been reported in West African countries, namely Senegal, and during a 2013 outbreak on Corsica.
Taxonomy
Schistosoma bovis is a digenetic, two-host blood fluke in cattle. It is one of nine Schistosoma species that share a similar lifecycle in the mammals they infect, called the haematobium group of schistosomes.[citation needed]
Hybrids between S. bovis and the human schistosome, Schistosoma haematobium were first described in 2009 in Northern Senegalese children, and to a lesser degree hybrids between S. bovis and cattle schistosome S. curassoni found only in cattle.[1] S. bovis / S. haematobium hybrids were also found during the 2013 outbreak traced to the Cavu river on Corsica.[2] As a hybrid increases the host range of the parent species, they affect transmission, and as is known from other schistosome hybrid pairings, morbidity and drug susceptibility, so they are epidemiologically important.[1]
Life cycle
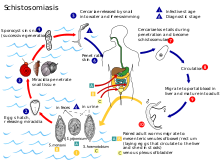
Schistosoma bovis infects two hosts, namely ruminants (cattle, goats, sheep, horses and camels) and freshwater snails (Bulinus sp. and Planorbarius sp.).[3]: 392
In water, its free swimming infective larval cercariae can burrow into the skin of its definite host, the ruminant, upon contact. The cercariae enter the host's blood stream, and travel to the liver to mature into adult flukes. Adult flukes can coat themselves with host antigen thus avoiding detection by the host immune system. After a period of about three weeks the young flukes migrate to the mesenteric veins of the gut to copulate. The female fluke lays eggs, which migrate into the lumen of the gut and leave the host upon defecation. In fresh water, the eggs hatch, forming free swimming miracidia.
Miracidia penetrate into the intermediate host, the freshwater snails[4] of the Bulinus spp., (e.g. B. globosus, B. forskalii, B. nyassanus and B. truncatus), except in Spain,[3]: 20 Portugal and Morocco, where Planorbarius metidjensis can transmit.[5] Inside the snail, the miracidium sheds its epithelium, and develops into a mother sporocyst. After two weeks the mother begins forming daughter sporocysts. One month – or more with cooler ambient temperatures – after a miracidium has penetrated into the snail, hundreds to thousands of cercariae of the same sex begin to be released through special areas of the sporocyst wall.[3]: 30 The cercariae cycle from the top of the water to the bottom in search of a host. They can enter the host epithelium within minutes.[6][3]: 34
Geographical distribution
S. bovis infects snails in Africa north of the equator, Europe (Sardinia, Corsica, Spain) and the Middle East as far as Iraq.[3]: 20 S. bovis – S. haematobium hybrids have been reported in Senegal, and as of 2013 in Corsica.[citation needed]
Diagnosis
Laboratory
The diagnosis of schistosomiasis can be made by microscopically examining the feces for the egg. The S. bovis egg is terminally spiked, spindle shaped, and the largest in size compared to other Schistosoma eggs at 202 μm length and 72μm width.[3]: 396 In chronic infections, or if eggs are difficult to find, an intradermal injection of Schistosome antigen to form a wheal can determine infection. Alternatively diagnosis can be made by complement fixation tests.[4]
As of 2012[update] commercial serological tests have included ELISA and an indirect immunofluorescence test, hampered by a low sensitivity ranging from 21% to 71%.[7] Exposure to any Schistosoma eggs or cercariae can cause false positive serological test results for individual Schistosoma species, unless highly specific antigens are used.[3]: 402
Various polymerase chain reaction (PCR) assays to differentiate S. bovis from other schistosomes in urine and naturally infected snails for surveillance purposes have been described since 2010.[8]
Pathology
The ova are initially deposited in the muscularis propria of the gut which leads to ulceration of the overlaying tissue. Infections are characterized by pronounced acute inflammation, blood and reactive epithelial changes. Granulomas and multinucleated giant cells may be seen.
Immunopathology
The immune system responds to eggs in the liver causing hypersensitivity; an immune response is necessary to prevent damage to hepatocytes. The hosts' antibodies bind to the tegument of the schistosome but not for long since the tegument is shed every few hours. The schistosome can also take on host proteins. Schistomiasis can be divided into three phases; Within the haematobium group S. bovis and S. curassoni appear to be closely related: (1) the migratory phase lasting from penetration to maturity, (2) the acute phase which occurs when the schistosomes begin producing eggs, and (3) the chronic phase which occurs mainly in endemic areas.[4]
Gene expression
S. bovis is one of the few non-bacterial species with a known moonlighting protein. Glyceraldehyde-3-phosphate dehydrogenase (GAPD) is also a common MP in bacteria.[9]
Treatment
Historically, antimonials and trichlorphon were tested against visceral schistosome infection in cattle.[10]: 245–248, 265–273 Antimony affects phosphofructokinase activity in Schistosoma, hycanthone intercalates Schistosoma DNA and the organophosphorus metabolite dichlorvos inhibits acetylcholinesterase, "but progressively less so in S. bovis".[3]: 44
Since the 1980s the drug of choice is praziquantel, a quinolone derivative which disrupts membranes, leading to calcium influx. It clears eggs from stool, and affects adult but not immature worms.[3]: 44–45 Damaged and dying flukes can be trapped in the liver and cause fatal portal vein thrombosis.[10]
Disease prevention
The main cause of schistosomiasis is the dumping of human and animal waste into water supplies. Hygienic disposal of waste would be sufficient to eliminate the disease.[4]
References
- ^ a b Huyse T, Webster BL, Geldof S, et al. (2009). "Bidirectional introgressive hybridization between a cattle and human schistosome species". PLOS Pathog. 5 (9): e1000571. doi:10.1371/journal.ppat.1000571. PMC 2731855. PMID 19730700.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Jérôme Boissier; Sébastien Grech-Angelini; Bonnie L Webster; et al. (2016). "Outbreak of urogenital schistosomiasis in Corsica (France): an epidemiological case study". The Lancet Infectious Diseases. 16 (8): 971–979. doi:10.1016/S1473-3099(16)00175-4. PMID 27197551.
- ^ a b c d e f g h i Adel A. F. Mahmoud (2001). Schistosomiasis. Imperial College Press. p. 524. ISBN 978-186094-146-7. Retrieved 31 July 2016.
- ^ a b c d Black, J. (2005). Microbiology: Principles and Explorations. Wiley, New York.
- ^ Mouahid A, Théron A (Dec 1987). "Schistosoma bovis: variability of cercarial production as related to the snail hosts: Bulinus truncatus, B. wright and Planorbarius metidjensis". Int J Parasitol. 17 (8): 1431–4. doi:10.1016/0020-7519(87)90078-6. PMID 3440697.
- ^ Roberts, L.; Janovy, J. (1996). Foundations of Parasitology (5th ed.). Wm. C. Brown Publishers, Dubuque, Iowa.
- ^ Kinkel HF, Dittrich S, Bäumer B, Weitzel T (2012). "Evaluation of eight serological tests for diagnosis of imported schistosomiasis". Clin Vaccine Immunol. 19 (6): 948–53. doi:10.1128/CVI.05680-11. PMC 3370443. PMID 22441394.
- ^ Akinwale OP, Hock TT, Chia-Kwung F, Zheng Q, Haimo S, Ezeh C, Gyang PV (2014). "Differentiating Schistosoma haematobium from Schistosoma magrebowiei and other closely related schistosomes by polymerase chain reaction amplification of a species specific mitochondrial gene". Tropical Parasitology. 4 (1): 38–42. doi:10.4103/2229-5070.129163. PMC 3992801. PMID 24754026.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Henderson, Brian; Martin, Andrew (2011). "Bacterial Moonlighting Proteins and Bacterial Virulence". In Dobrindt, Ulrich; Hacker, Jörg H.; Svanborg, Catharina (eds.). Between Pathogenicity and Commensalism. Berlin, Heidelberg: Springer Berlin Heidelberg. pp. 155–213. doi:10.1007/82_2011_188. ISBN 978-3-642-36559-1. ISSN 0070-217X.
- ^ a b Reinecke, RK (1983). "Phylum plathelminthes". Veterinary helminthology. Durban, SouthAfrica: Butterworths.
