Breast reconstruction: Difference between revisions
m Removing Link GA template (handled by wikidata) |
m added source that shows there is little evidence to favour immediate vs delayed reconstruciton. |
||
| Line 3: | Line 3: | ||
==Overview== |
==Overview== |
||
The primary part of the procedure can often be carried out immediately following the mastectomy. As with many other surgeries, patients with significant medical comorbidities ([[high blood pressure]], [[obesity]], [[diabetes]]) and [[Tobacco smoking|smokers]] are higher-risk candidates. Surgeons may choose to perform delayed reconstruction to decrease this risk. The infection rate may be higher with primary reconstruction (done at the same time as mastectomy), but there are psychologic and financial benefits to having a single primary reconstruction. Patients expected to receive [[radiation therapy]] as part of their adjuvant treatment are also commonly considered for delayed autologous reconstruction due to significantly higher complication rates with tissue expander-implant techniques in those patients. |
The primary part of the procedure can often be carried out immediately following the mastectomy. As with many other surgeries, patients with significant medical comorbidities ([[high blood pressure]], [[obesity]], [[diabetes]]) and [[Tobacco smoking|smokers]] are higher-risk candidates. Surgeons may choose to perform delayed reconstruction to decrease this risk. There is little evidence available from randomised studies to favour immediate or delayed reconstruction<ref>{{cite journal|last1=D'Souza|first1=N|last2=Darmanin|first2=G|last3=Fedorowicz|first3=Z|title=Immediate versus delayed reconstruction following surgery for breast cancer.|journal=The Cochrane database of systematic reviews|date=2011 Jul 6|issue=7|pages=CD008674|pmid=21735435}}</ref>. The infection rate may be higher with primary reconstruction (done at the same time as mastectomy), but there are psychologic and financial benefits to having a single primary reconstruction. Patients expected to receive [[radiation therapy]] as part of their adjuvant treatment are also commonly considered for delayed autologous reconstruction due to significantly higher complication rates with tissue expander-implant techniques in those patients. |
||
Breast reconstruction is a large undertaking that usually takes multiple operations. Sometimes these follow-up surgeries are spread out over weeks or months. If an implant is used, the individual runs the same risks and complications as those who use them for [[breast augmentation]] but has higher rates of [[capsular contracture]] (tightening or hardening of the scar tissue around the implant) and revisional surgeries. |
Breast reconstruction is a large undertaking that usually takes multiple operations. Sometimes these follow-up surgeries are spread out over weeks or months. If an implant is used, the individual runs the same risks and complications as those who use them for [[breast augmentation]] but has higher rates of [[capsular contracture]] (tightening or hardening of the scar tissue around the implant) and revisional surgeries. |
||
Revision as of 22:03, 22 October 2014

Breast reconstruction is the rebuilding of a breast, usually in women. It involves using autologous tissue or prosthetic material to construct a natural-looking breast. Often this includes the reformation of a natural-looking areola and nipple. This procedure involves the use of implants or relocated flaps of the patient's own tissue.
Overview
The primary part of the procedure can often be carried out immediately following the mastectomy. As with many other surgeries, patients with significant medical comorbidities (high blood pressure, obesity, diabetes) and smokers are higher-risk candidates. Surgeons may choose to perform delayed reconstruction to decrease this risk. There is little evidence available from randomised studies to favour immediate or delayed reconstruction[1]. The infection rate may be higher with primary reconstruction (done at the same time as mastectomy), but there are psychologic and financial benefits to having a single primary reconstruction. Patients expected to receive radiation therapy as part of their adjuvant treatment are also commonly considered for delayed autologous reconstruction due to significantly higher complication rates with tissue expander-implant techniques in those patients.
Breast reconstruction is a large undertaking that usually takes multiple operations. Sometimes these follow-up surgeries are spread out over weeks or months. If an implant is used, the individual runs the same risks and complications as those who use them for breast augmentation but has higher rates of capsular contracture (tightening or hardening of the scar tissue around the implant) and revisional surgeries.
Outcomes based research on quality of life improvements and psychosocial benefits associated with breast reconstruction [2][3] served as the stimulus in the United States for the 1998 Women's Health and Cancer Rights Act[1], which mandated health care payer coverage for breast and nipple reconstruction, contralateral procedures to achieve symmetry, and treatment for the sequelae of mastectomy. This was followed in 2001 by additional legislation imposing penalties on noncompliant insurers. Similar provisions for coverage exist in most countries worldwide through national health care programs.
Techniques
There are many methods for breast reconstruction. The two most common are:
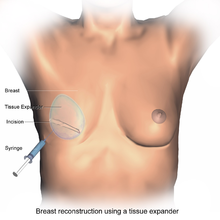
- Tissue Expander - Breast implants This is the most common technique used worldwide. The surgeon inserts a tissue expander, a temporary silastic implant, beneath a pocket under the pectoralis major muscle of the chest wall. The pectoral muscles may be released along its inferior edge to allow a larger, more supple pocket for the expander at the expense of thinner lower pole soft tissue coverage. The use of acellular human or animal dermal grafts have been described as an onlay patch to increase coverage of the implant when the pectoral muscle is released, which purports to improve both functional and aesthtic outcomes of implant-expander breast reconstruction.[4][5]
- In a process that can take weeks to months, saline solution is injected to progressively expand the overlaying tissue. Once the expander has reached an acceptable size, it may be removed and replaced with a more permanent implant. Reconstruction of the areola and nipple are usually performed in a separate operation after the skin has stretched to its final size.
- Flap reconstruction The second most common procedure uses tissue from other parts of the patient's body, such as the back, buttocks, thigh or abdomen. This procedure may be performed by leaving the donor tissue connected to the original site to retain its blood supply (the vessels are tunnelled beneath the skin surface to the new site) or it may be cut off and new blood supply may be connected.
- The latissimus dorsi muscle flap is the donor tissue available on the back. It is a large flat muscle which can be employed without significant loss of function. It can be moved into the breast defect while still attached to its blood supply under the arm pit (axilla). A latissimus flap is usually used to recruit soft-tissue coverage over an underlying implant. Enough volume can be recruited occasionally to reconstruct small breasts without an implant.


- Abdominal flaps The abdominal flap for breast reconstruction is the TRAM flap (Transverse Rectus Abdominis Myocutaneous flap) or its technically distinct variants of microvascular "perforator flaps" like the DIEP/SIEP flaps. In a TRAM procedure, a portion of the abdomen tissue group, including skin, adipose tissues, minor muscles and connective tissues, is taken from the patient's abdomen and transplanted onto the breast site. Both TRAM and DIEP/SIEP use the abdominal tissue between the umbilicus and the pubis. The DIEP flap and free-TRAM flap require advanced microsurgical technique and are less common as a result. Both can provide enough tissue to reconstruct large breasts. These procedures are preferred by some breast cancer patients because they result in an abdominoplasty (tummy tuck), and allow the breast to be reconstructed with one's own tissues instead of a foreign implant. TRAM flap procedures may weaken the abdominal wall and torso strength, but are tolerated well in most patients. To prevent muscle weakness and incisional hernias, the portion of abdominal wall exposed by reflection of the rectus abdominis muscle may be strengthened by a piece of surgical mesh placed over the defect and sutured in place. Perforator techniques such as the DIEP (deep inferior epigastric perforator) flap and SIEA (superficial inferior epigastric artery) flap require precise dissection of small perforating vessels through the rectus muscle, and purport the advantage of less weakening of the abdominal wall, though rectus abdominus muscle function may still be compromised. Other total autologous tissue breast reconstruction donor sites include the buttocks (superior or inferior gluteal artery perforator flaps (SGAP or IGAP)). The purpose of perforator flaps (DIEP, SIEA, SGAP, IGAP) is to provide sufficient skin and fat for an aesthetic reconstruction while minimizing morbidity from harvesting the underlying muscles. See free flap breast reconstruction for more information.
- Mold-assisted reconstruction Made using laser scanning and 3D printing, a patient-specific silicone mold can be used as an aid during surgery. It is used as a guide for orienting and shaping the flap to improve accuracy and symmetry.[6]
Other considerations
To restore the appearance of the breast with surgical reconstruction, there are a few options regarding the nipple and areola.
- A nipple prosthesis can be used to restore the appearance of the reconstructed breast. Impressions can be made and photographs can be used to accurately replace the nipple lost with some types of mastectomies. This can be instrumental in restoring the psychological well-being of the breast cancer survivor. The same process can be used to replicate the remaining nipple in cases of a single mastectomy. Ideally, a prosthesis is made around the time of the mastectomy and it can be used just weeks after the surgery.
- Nipple reconstruction is usually delayed until after the breast mound reconstruction is completed so that the positioning can be planned precisely. There are several methods of reconstructing the nipple-areolar complex, including:
- Nipple-Areolar Composite Graft (Sharing) - if the contralateral breast has not been reconstructed and the nipple and areolar are sufficiently large, tissue may be harvested and used to recreate the nipple-areolar complex on the reconstructed side.
- Local Tissue Flaps - a nipple may be created by raising a small flap in the target area and producing a raised mound of skin. To create an areola, a circular incision may be made around the new nipple and sutured back again. The nipple and areolar region may then be tattooed to produce a realistic colour match with the contralateral breast.
- Local Tissue Flaps With Use of AlloDerm - as above, a nipple may be created by raising a small flap in the target area and producing a raised mound of skin. AlloDerm (cadaveric dermis) can then be inserted into the core of the new nipple acting like a "strut" which may help maintain the projection of the nipple for a longer period of time. The nipple and areolar region may then be tattooed later.[7] There are however some important issues in relation to NAC Tattooing that should be considered prior to opting for tattooing, such as the choice of pigments and equipment used for the procedure.[8]
One of the challenges in breast reconstruction is to match the reconstructed breast to the mature breast on the other side (often fairly 'ptotic' - droopy.) This often requires a lift (mastopexy), reduction, or augmentation of the other breast.
Follow-up and recovery
Recovery from implant-based reconstruction is generally faster than with flap-based reconstructions, but both take at least three to six weeks of recovery and both require follow-up surgeries in order to construct a new areola and nipple. All recipients of these operations should refrain from strenuous sports, overhead lifting, and sexual activity during the recovery period. TRAM flap patients can show abdominal-muscle weakness on electromyogram (EMG) studies, but clinically most patients who have undergone unilateral breast reconstruction (reconstruction of one breast only) return to normal activities after recovery.
Patients who have undergone bilateral breast reconstruction with TRAM flaps (i.e. reconstruction of both breasts) require sacrifice of both rectus muscles and tend to have permanent abdominal strength loss. For this reason, many plastic surgeons now frown upon bilateral breast reconstruction with TRAM flaps. This also explains the significant patient interest in perforator flap techniques such as the DIEP flap which preserves abdominal muscle function long-term. These patients tend to return to full activity after several weeks without permanent limitations.
There is little information about upper body exercise post-mastectomy. Issues such as simple mastectomy, mastectomy with reconstruction, and mastectomy with lymph node excision and reconstruction all factor into limitations to amount and extent of upper body exercise. Generally, cardiac exercise (treadmill, walking, etc.) are approved for rehabilitation post-surgery and for weight control.[citation needed]
Women who have undergone breast reconstruction must still be followed for local or regional recurrence of their cancer with manual exams of the breast/chest wall and axilla.
The most effective relief from breast reconstruction is hilotherapy, a therapy that provides relief from hematoma, pain, and swelling post-surgery without the dangers of frostbite and skin necrosis.[citation needed]
See also
- Breast implant
- Breast lift
- Breast reduction plasty
- Free flap breast reconstruction
- Nipple prosthesis
Additional images
-
Breast Reconstruction using a Prosthesis
References
- ^ D'Souza, N; Darmanin, G; Fedorowicz, Z (2011 Jul 6). "Immediate versus delayed reconstruction following surgery for breast cancer". The Cochrane database of systematic reviews (7): CD008674. PMID 21735435.
{{cite journal}}: Check date values in:|date=(help) - ^ Harcourt, DM, Rumsey, NJ, Ambler, NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg 2003; 111:1060. PMID 12621175
- ^ Brandberg, Y, Malm, M, Blomqvist, L. A prospective and randomized study, "SVEA," comparing effects of three methods for delayed breast reconstruction on quality of life, patient-defined problem areas of life, and cosmetic result. Plast Reconstr Surg 2000; 105:66. PMID 10626972
- ^ Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg. 2005 Sep;55(3):232-9. PMID 16106158
- ^ Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg. 2006 Jul;57(1):1-5. PMID 16799299
- ^ Ferry Melchels et al. 2011 Biofabrication 3 034114 doi:10.1088/1758-5082/3/3/034114
- ^ Garramone, D.O., Charles E; Lam, Ben (May 2007). "Use of AlloDerm in primary nipple reconstruction to improve long-term nipple projection". Plastic and reconstructive surgery. 119 (6): 1663–8. doi:10.1097/01.prs.0000258831.38615.80. PMID 17440338.
{{cite journal}}:|access-date=requires|url=(help) - ^ A. Darby. 3D Nipple Tattooing a New Service? (inc revisions). CosmeticTattoo.org Educational Articles 24/10/2013
External links
- Breast Reconstruction Following Breast Removal from the American Society of Plastic Surgeons
- National Cancer Institute breast cancer page
- US Dept. of Labor - Women's Health & Cancer Rights Act of 1998
- Plastic Surgery Stirs a Debate

