Corticobasal degeneration
| Corticobasal degeneration | |
|---|---|
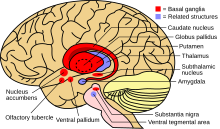 | |
| Basal ganglia along with cerebral cortex are involved in this condition | |
| Specialty | Neurology |
Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia.[1] CBD symptoms typically begin in people from 50 to 70 years of age, and the average disease duration is six years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.
Signs and symptoms
Because CBD is progressive, a standard set of diagnostic criteria can be used, which is centered on the disease's evolution. Included in these fundamental features are problems with cortical processing, dysfunction of the basal ganglia, and a sudden and detrimental onset.[2] Psychiatric and cognitive dysfunctions, although present in CBD, are much less prevalent and lack establishment as common indicators of the presence of the disease.[3]
Although corticobasal degeneration has a plethora of symptoms, some are more prevalent than others. In a study of 147 patients with CBD, it was found that all of them had at least one Parkinsonian sign, 95% having two and 93% had some higher order dysfunction (cognitive impairments like acalculia, sensory loss, dementia, neglect, etc.). In a separate study of 14 patients recorded 3 years after the onset of symptoms, many patients had high numbers of motor symptoms. 71% had bradykinesia (slow movements), 64% showed apraxia, 43% reported limb dystonia, and although more cognitive 36% had dementia. In another study of 36, over half had a useless/alien arm and 27% had a gait impediment[21]. From this, we can see why CBD is hard to diagnose. Even if it can be distinguished as different from one of the other similar diseases, the varying combinations of symptoms create a difficult path to diagnosis.[citation needed]
Motor and associated cortical dysfunctions
Some of the most prevalent symptom types in people exhibiting CBD pertain to identifiable movement disorders and problems with cortical processing. These symptoms are initial indicators of the presence of the disease. Each of the associated movement complications typically appears asymmetrically and the symptoms are not observed uniformly throughout the body. For example, a person exhibiting an alien hand syndrome (explained later) in one hand, will not correspondingly display the same symptom in the other hand. Predominant movement disorders and cortical dysfunctions associated with CBD include:[citation needed]
- Parkinsonism
- Alien hand syndrome
- Apraxia (ideomotor apraxia and limb-kinetic apraxia)
- Aphasia[3]
Parkinsonism
The presence of parkinsonism as a clinical symptom of CBD is largely responsible for complications in developing unique diagnostic criteria for the disease.[4] Other such diseases in which parkinsonism forms an integral diagnostic characteristic are Parkinson's disease (PD) and progressive supranuclear palsy (PSP). Parkinsonism in CBD is largely present in an extremity such as the arm, and is always asymmetric. It has been suggested that non-dominant arm is involved more often.[5] Common associated movement dysfunctions that comprise parkinsonism are rigidity, bradykinesia, and gait disorder, with limb rigidity forming the most typical manifestation of parkinsonism in CBD. Despite being relatively indistinct, this rigidity can lead to disturbances in gait and correlated movements. Bradykinesia in CBD occurs when there is notable slowing in the completion of certain movements in the limbs. In an associated study, it was determined that, three years following first diagnosis, 71% of persons with CBD demonstrate the presence of bradykinesia.[3]
Alien hand syndrome
Alien hand syndrome has been shown to be prevalent in roughly 60% of those people diagnosed with CBD.[6] This disorder involves the failure of an individual to control the movements of their hand, which results from the sensation that the limb is "foreign".[2] The movements of the alien limb are a reaction to external stimuli and do not occur sporadically or without stimulation. The presence of an alien limb has a distinct appearance in CBD, in which the diagnosed individual may have a "tactile mitgehen". This mitgehen (German, meaning "to go with") is relatively specific to CBD, and involves the active following of an experimenter's hand by the subject's hand when both hands are in direct contact. Another, rarer form of alien hand syndrome has been noted in CBD, in which an individual's hand displays an avoidance response to external stimuli. Additionally, sensory impairment, revealed through limb numbness or the sensation of prickling, may also concurrently arise with alien hand syndrome, as both symptoms are indicative of cortical dysfunction. Like most of the movement disorders, alien hand syndrome also presents asymmetrically in those diagnosed with CBD.[7]
Apraxia
Ideomotor apraxia (IMA), although clearly present in CBD, often manifests atypically due to the additional presence of bradykinesia and rigidity in those individuals exhibiting the disorders. The IMA symptom in CBD is characterized by the inability to repeat or mimic particular movements (whether significant or random) both with or without the implementation of objects. This form of IMA is present in the hands and arms, while IMA in the lower extremities may cause problems with walking. Those with CBD that exhibit IMA may appear to have trouble initiating walking, as the foot may appear to be fixed to floor. This can cause stumbling and difficulties in maintaining balance.[3] IMA is associated with deterioration in the premotor cortex, parietal association areas, connecting white matter tracts, thalamus, and basal ganglia. Some individuals with CBD exhibit limb-kinetic apraxia, which involves dysfunction of more fine motor movements often performed by the hands and fingers.[6]
Aphasia
Aphasia in CBD is revealed through the inability to speak or a difficulty in initiating spoken dialogue and falls under the non-fluent (as opposed to fluent or flowing) subtype of the disorder. This may be related to speech impairment such as dysarthria, and thus is not a true aphasia, as aphasia is related to a change in language function, such as difficulty retrieving words or putting words together to form meaningful sentences. The speech and/or language impairments in CBD result in disconnected speech patterns and the omission of words. Individuals with this symptom of CBD often lose the ability to speak as the disease progresses.[3]
Psychiatric and cognitive disorders
Psychiatric problems associated with CBD often present as a result of the debilitating symptoms of the disease. Prominent psychiatric and cognitive conditions cited in individuals with CBD include dementia, depression, and irritability, with dementia forming a key feature that sometimes leads to the misdiagnosis of CBD as another cognitive disorder such as Alzheimer's disease (AD). Frontotemporal dementia can be an early feature.[8]
Molecular features
Neuropathological findings associated with CBD include the presence of astrocytic abnormalities within the brain and improper accumulation of the protein tau (referred to as tauopathy).[9]
Astroglial inclusions
Postmortem histological examination of the brains of individuals diagnosed with CBD reveal unique characteristics involving the astrocytes in localized regions.[10] The typical procedure used in the identification of these astroglial inclusions is the Gallyas-Braak staining method.[11] This process involves exposing tissue samples to a silver staining material which marks for abnormalities in the tau protein and astroglial inclusions.[12] Astroglial inclusions in CBD are identified as astrocytic plaques, which present as annularly displays of blurry outgrowths from the astrocyte. A recent study indicated that produces a high density of astrocytic plaques in the anterior portion of the frontal lobe and in the premotor area of the cerebral cortex.[13]
Tauopathy
The protein tau is an important microtubule-associated protein (MAP), and is typically found in neuronal axons. However, malfunctioning of the development of the protein can result in unnatural, high-level expression in astrocytes and glial cells. As a consequence, this is often responsible for the astrocytic plaques prominently noted in histological CBD examinations. Although they are understood to play a significant role in neurodegenerative diseases such as CBD, their precise effect remains a mystery.[12]
In recent years Corticobasal Degeneration is seen to be a tauopathy[22]. This is believed due to the most common indicator of CBD being a faulty tau protein. Tau proteins are integral in keeping microtubules stable and these defective cells create 4 microtubule-binding repeats[23]. These 4 binding repeats have increased affinity in binding with microtubules[25]. Because of this increased affinity, they form insoluble fibers (also called "paired helical filaments). Microtubules themselves keep the cell and cytoskeletal structure stable[24]. Thus, when Tau proteins create unnatural configurations, microtubules become unstable, and eventually leads to cell death.[citation needed]
Diagnosis
New diagnostic criteria known as the Armstrong criteria were proposed in 2013, although the accuracy of these is limited and further research is needed.[14]
Recent findings in clinicopathology have made it possible to distinguish CBD from Parkinson's and increase the accuaracy of diagnosis, using developments in MRI and nuclear medicine. [15]
Criteria
- Insidious onset and gradual progression
- Lasts 1 year or more
- Meets one of the four subtypes:
- Possible CBS
- FBS or NAV
- PSPS plus at least one CBS feature other than limb rigidity or akinesia
- No exclusion criteria present
- More likely if onset is after age 50
- More likely if no family history (2 or more relatives)
- More likely if no genetic mutation affecting T[clarification needed] (e.g., MAPT)[16]
Possible corticobasal syndrome subtype
Symptoms may be symmetric or asymmetric.
One or more of:[citation needed]
- limb rigidity or akinesia
- limb dystonia
- limb myoclonus, plus one of:
- orobuccal or limb apraxia
- cortical sensory deficit
- alien limb phenomena (more than simple levitation)
More likely (probable sporadic CBS) if:[citation needed]
- Asymmetric presentation
- Onset after age 50
- No family history (2 or more relatives)
- No genetic mutation affecting T (e.g. MAPT)
- plus two of:
- limb rigidity or akinesia
- limb dystonia
- limb myoclonus
- plus two of:
- orobuccal or limb apraxia,
- cortical sensory deficit
- alien limb phenomena (more than simple levitation)[16]
Frontal behavioural-spatial syndrome subtype
Two of:[citation needed]
- executive dysfunction
- behavioural or personality changes
- visuospatial deficits
NAV of primary progressive aphasia subtype
Effortful, agrammatic speech plus at least one of:[citation needed]
- impaired grammar/sentence comprehension with relatively preserved single word comprehension or
- groping, distorted speech production (apraxia of speech)
Progressive supranuclear palsy syndrome subtype
Three of:[citation needed]
- axial or symmetric limb rigidity or akinesia
- postural instability or falls
- urinary incontinence
- behavioural changes
- supranuclear vertical gaze palsy or decreased vertical saccade velocity
Exclusion criteria
These apply to all types of CBD.
- Evidence of Lewy body disease
- multiple system atrophy
- Alzheimer's disease
- ALS
- semantic or logopenic variant primary progressive aphasia
- structural lesion suggestive of focal cause
- granulin mutation or reduced plasma progranulin levels
- TDP-43 or fused in sarcoma (FUS) mutations[16]
The diagnostic criteria for clinical use may result in a misdiagnosis of other tau-based diseases.[14]
The probable criteria are proposed for clinical research.[14]
Clinical vs. postmortem
One of the most significant problems associated with CBD is the inability to perform a definitive diagnosis while an individual exhibiting the symptoms associated with CBD is still alive. A clinical diagnosis of CBD is performed based upon the specified diagnostic criteria, which focus mainly on the symptoms correlated with the disease. However, this often results in complications as these symptoms often overlap with numerous other neurodegenerative diseases.[17] Frequently, a differential diagnosis for CBD is performed, in which other diseases are eliminated based on specific symptoms that do not overlap. However, some of the symptoms of CBD used in this process are rare to the disease, and thus the differential diagnosis cannot always be used.[3]
Postmortem diagnosis provides the only true indication of the presence of CBD. Most of these diagnoses utilize the Gallyas-Braak staining method, which is effective in identifying the presence of astroglial inclusions and coincidental tauopathy.[citation needed]
Overlap with other diseases
Progressive supranuclear palsy (PSP) is frequently the disease most often confused with CBD. Both PSP and CBD result in similar symptoms, and both display tauopathies upon histological inspection.[18] However, it has been noted that tauopathy in PSP results in tuft-shaped astrocytes in contrast with the ring-shaped astrocytic plaques found as a result of CBD.[13]
Individuals diagnosed with PD often exhibit similar movement dysfunction as those diagnosed with CBD, which adds complexity to its diagnosis. Some other neurodegenerative diseases including Alzheimer's disease (AD), dementia with Lewy bodies (DLB), chronic traumatic encephalopathy (CTE) and frontotemporal dementia (FTD) also show commonalities with CBD.[3][19][8]
Neuroimaging
The types of imaging techniques that are most prominently utilized when studying and/or diagnosing CBD are:[citation needed]
- magnetic resonance imaging (MRI)
- single-photon emission computed tomography (SPECT)
- fluorodopa positron emission tomography (FDOPA PET)
Developments or improvements in imaging techniques provide the future possibility for definitive clinical diagnosis prior to death. However, despite their benefits, information learned from MRI and SPECT during the beginning of CBD progression tend to show no irregularities that would indicate the presence of such a neurodegenerative disease.[3] FDOPA PET is used to study the efficacy of the dopamine pathway.[20]
Despite the undoubted presence of cortical atrophy (as determined through MRI and SPECT) in individuals experiencing the symptoms of CBD, this is not an exclusive indicator for the disease. Thus, the utilization of this factor in the diagnosis of CBD should be used only in combination with other clinically present dysfunctions.[4]
MRI
MRI images are useful in displaying atrophied portions of neuroanatomical positions within the brain. As a result, it is especially effective in identifying regions within different areas of the brain that have been negatively affected due to the complications associated with CBD. To be specific, MRI of CBD typically shows posterior parietal and frontal cortical atrophy with unequal representation in corresponding sides. In addition, atrophy has been noted in the corpus callosum.[20]
Functional MRI (fMRI) has been used to evaluate the activation patterns in various regions of the brain of individuals affected with CBD. Upon the performance of simple finger motor tasks, subjects with CBD experienced lower levels of activity in the parietal cortex, sensorimotor cortex, and supplementary motor cortex than those individuals tested in a control group.[20]
SPECT
SPECT is currently being used to try to detect CBD. With many patients of CBD, there are areas in the basal ganglia which have difficulties receiving dopamine, typically asymmetrically. Specifically affected, are dopamine transporters which are presynaptic on the nigrostriatal cells. SPECT is used to detect these abnormalities in Dopamine transporters. Given that many patients have asymmetrical loss of function and metabolism this can help differentiate patients with CBD and those with Alzheimer's.[citation needed]
SPECT studies of individuals diagnosed with CBD involve perfusion analysis throughout the parts of the brain. SPECT evaluation through perfusion observation consists of monitoring blood release into different locations in tissue or organ regions, which, in the case of CBD, pertains to localized areas within the brain. Tissue can be characterized as experiencing overperfusion, underperfusion, hypoperfusion, or hyperperfusion. Overperfusion and underperfusion relate to a comparison with the overall perfusion levels within the entire body, whereas hypoperfusion and hyperperfusion are calculated in comparison to the blood flow requirements of the tissue in question. In general, the measurements taken for CBD using SPECT are referred to as regional cerebral blood flow (rCBF).[20]
In general, SPECT reveals hypoperfusion within both the posterior regions of the frontal and parietal lobes. As in images gathered through MRI, SPECT images indicated asymmetry in the presentation of abnormalities throughout the brain.[4] Additional studies have revealed the presence of perfusion anomalies in the thalamus, temporal cortex, basal ganglia, and pontocerebellar (from the pons to the cerebellum) locations within subjects' brains.[20]
FDOPA PET
Research has suggested that the integrity of the dopamine system in the striatum has been damaged as an effect of CBD. Current studies employing the use of FDOPA PET scanning (FDOPA PET) as a possible method for identifying CBD have focused on analyzing the efficiency of neurons in the striatum that utilize the neurotransmitter dopamine. These studies have concluded that, in general, dopamine uptake was diminished in the caudate and the putamen. This characteristic also has the potential to be useful in distinguishing CBD from the similar PD, as individuals having been diagnosed with PD were more likely to have a lower uptake of dopamine than in individuals with CBD.[20]
Other clinical tests or procedures that monitor the presence of dopamine within the brain (β-CIT SPECT and IBZM SPECT) have shown similar findings. β-CIT serves as an indicator for presynaptic dopaminergic neurons, whereas IBZM is a tracer that shows an affinity for the postsynaptic neurons of the same type. Despite agreement with other imaging studies, these two SPECT methods suffer some scrutiny due to better accuracy in other imaging methods. However, β-CIT SPECT has proven to be helpful in distinguishing CBD from PSP and multiple system atrophy (MSA).[20]
Corticobasal syndrome
All of the disorders and dysfunctions associated with CBD can often be categorized into a class of symptoms that present with the disease of CBD. These symptoms that aid in clinical diagnosis are collectively referred to as corticobasal syndrome (CBS) or corticobasal degeneration syndrome (CBDS). Alzheimer's disease, Pick's disease, FTDP-17 and progressive supranuclear palsy can display a corticobasal syndrome.[21][22] It has been suggested that the nomenclature of corticobasal degeneration only be used for naming the disease after it has received verification through postmortem analysis of the neuropathology.[4] CBS patients with greater temporoparietal degeneration are more likely to have AD pathology as opposed to frontotemporal lobar degeneration.[23]
Treatment
Because the exact cause of CBD is unknown, there exists no formal treatment for the disease. Instead, treatments focus on minimizing the appearance or effect of the symptoms resulting from CBD. The most easily treatable symptom of CBD is parkinsonism, and the most common form of treatment for this symptom is the application of dopaminergic drugs. However, in general only moderate improvement is seen and the relief from the symptom is not long-lasting. In addition, palliative therapies, including the implementation of wheelchairs, speech therapy, and feeding techniques, are often used to alleviate many of the symptoms that show no improvement with drug administration.[24]
There is no consensus on what causes CBD and so most of the treatment goes in helping symptoms. Many treatments have low success rates or have not been tested thoroughly or produced frequently. For example, in relation to the motor aspect of disability, CBD has a high resistance against treatments to help the dopamine intake like levodopa. A number of studies have reported no real levels of improvement based with the use of similar drugs/dopaminergic agonists. Because of the brains levels of inhibition, some medications have focused on creating an inhibition that would negate the effect. Many of these relaxants and anticonvulsants have some success but also have unwanted side effects[21]. Cognitive and associative effects of CBD are also hard to treat as we[who?] are still unsure of many of the treatments for the symptomatic diseases that ensue like dementia, aphasia, neglect, apraxia and others.[citation needed]
Epidemiology
Clinical presentation of CBD usually does not occur until age 60, with the earliest recorded diagnosis and subsequent postmortem verification being age 28.[20] Although men and women present with the disease, some analysis has shown a predominant appearance of CBD in women. Current calculations suggest that the prevalence of CBD is approximately 4.9 to 7.3 per 100,000 people. The prognosis for an individual diagnosed with CBD is death within approximately eight years, although some patients have been diagnosed over 17 years ago (2017) and are still in relatively good standing, but with serious debilitation such as dysphagia, and overall limb rigidity.[citation needed] The partial (or total) use of a feeding tube may be necessary and will help prevent aspiration pneumonia, primary cause of death in CBD. Incontinence is common, as patients often can't express their need to go, due to eventual loss of speech. Therefore, proper hygiene is mandatory to prevent urinary tract infections.[3]
CBD research has been limited by the rarity of the disease and the lack of research criteria. It is estimated to affect 0.6-0.9 per 100,000 per year.[citation needed]
Progressive supranuclear palsy (PSP) without CBD is estimated to be ten times more common. CBD represents roughly 4–6% of patients with Parkinsonism. Average age at disease onset is about 64, with the youngest confirmed onset being at age 43. There may be a slight female predominance.[25]
History
Corticobasal syndrome was first recognized in 1967 when Rebeiz, Kolodny, and Richardson Jr described three people with a progressive asymmetric akinetic-rigid syndrome combined with apraxia, which they named corticodentatonigral degeneration with neuronal achromasia.[25][26] The condition was "mostly forgotten" until 1989, when Marsden et al. used the name corticobasal degeneration.[25] In 1989 Gibb and colleagues provided detailed clinical and pathological descriptions in a further three cases adopting the name corticobasal degeneration,[27] after which various other names included "corticonigral degeneration with nuclear achromasia" and "cortical basal ganglionic degeneration".[2] Although the underlying cause of CBD is unknown, the disease occurs as a result of damage to the basal ganglia, specifically marked by neuronal degeneration or depigmentation (loss of melanin in a neuron) in the substantia nigra.[18] Additional distinguishing neurological features of those diagnosed with CBD consist of asymmetric atrophy of the frontal and parietal cortical regions of the brain.[2] Postmortem studies of patients diagnosed with CBD indicate that histological attributes often involve ballooning of neurons, gliosis, and tauopathy.[18] Much of the pioneering advancements and research performed on CBD has been completed within the past decade or so, due to the relatively recent formal recognition of the disease.[citation needed]
The Office of Rare Diseases in the United States created the first criteria in 2002, and the Armstrong clinical diagnostic criteria were created in 2013.[25]
Society and culture
The Salt Path by Raynor Winn is an inspiring account of walking England's 630 mile South West Coast Path with her husband who had corticobasal degeneration.[28]
See also
References
- ^ "Corticobasalganglionic Degeneration Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". Archived from the original on 2009-03-23. Retrieved 2009-03-20.
- ^ a b c d Wadia PM, Lang AE (2007). "The many faces of corticobasal degeneration". Parkinsonism & Related Disorders. 13: S336–S40. doi:10.1016/s1353-8020(08)70027-0. PMID 18267261.
- ^ a b c d e f g h i Mahapatra RK, Edwards MJ, Schott JM, Bhatia KP (2004). "Corticobasal degeneration". Lancet Neurology. 3 (12): 736–43. doi:10.1016/s1474-4422(04)00936-6. PMID 15556806. S2CID 15324889.
- ^ a b c d Koyama M, Yagishita A, Nakata Y, helloHayashi M, Bandoh M, et al. (2007). "Imaging of corticobasal degeneration syndrome". Neuroradiology. 49 (11): 905–12. doi:10.1007/s00234-007-0265-6. PMID 17632713. S2CID 35778587.
- ^ Rana AQ, Ansari H, Siddiqui I (2012). "The relationship between arm dystonia in corticobasal degeneration and handedness". Journal of Clinical Neuroscience. 19 (8): 1134–6. doi:10.1016/j.jocn.2011.10.012. PMID 22705141. S2CID 2233432.
- ^ a b Belfor N, Amici S, Boxer AL, Kramer JH, Gorno-Tempini ML, et al. (2006). "Clinical and neuropsychological features of corticobasal degeneration". Mechanisms of Ageing and Development. 127 (2): 203–7. doi:10.1016/j.mad.2005.09.013. PMID 16310834. S2CID 35169781.
- ^ FitzGerald DB, Drago V, Jeong Y, Chang YL, White KD, et al. (2007). "Asymmetrical alien hands in corticobasal degeneration". Movement Disorders. 22 (4): 581–4. doi:10.1002/mds.21337. PMID 17230447. S2CID 41998716.
- ^ a b Lee SE, Rabinovici GD, Mayo MC, Wilson SM, Seeley WW, et al. (August 2011). "Clinicopathological correlations in corticobasal ganglionic degeneration". Annals of Neurology. 70 (2): 327–340. doi:10.1002/ana.22424. PMC 3154081. PMID 21823158.
- ^ Rizzo G, Martinelli P, Manners D, Scaglione C, Tonon C, et al. (October 2008). "Diffusion-weighted brain imaging study of patients with clinical diagnosis of corticobasal degeneration, progressive supranuclear palsy and Parkinson's disease". Brain. 131 (Pt 10): 2690–700. doi:10.1093/brain/awn195. PMID 18819991.
- ^ Zhu MW, Wang LN, Li XH, Gui QP (April 2004). "Glial abnormalities in progressive supranuclear palsy and corticobasal degeneration". Zhonghua Bing Li Xue Za Zhi. 33 (2): 125–9. doi:10.3760/j.issn:0529-5807.2004.02.008. PMID 15132848.
- ^ "CBD Identification - Chemistry and Toxicology". The Drug Store. 2020-08-26. Retrieved 2020-10-17.
- ^ a b Komori T (1999). "Tau-positive glial inclusions in progressive supranuclear palsy, corticobasal degeneration and Pick's disease". Brain Pathology. 9 (4): 663–79. doi:10.1111/j.1750-3639.1999.tb00549.x. PMC 8098509. PMID 10517506. S2CID 3142586.
- ^ a b Hattori M, Hashizume Y, Yoshida M, Iwasaki Y, Hishikawa N, et al. (2003). "Distribution of astrocytic plaques in the corticobasal degeneration brain and comparison with tuft-shaped astrocytes in the progressive supranuclear palsy brain". Acta Neuropathologica. 106 (2): 143–9. doi:10.1007/s00401-003-0711-4. PMID 12732936. S2CID 25741692.
- ^ a b c Shimohata T, Aiba I, Nishizawa M (2016). "[Diagnoses of corticobasal syndrome and corticobasal degeneration]". Rinsho Shinkeigaku (in Japanese). 56 (3): 149–57. doi:10.5692/clinicalneurol.cn-000841. PMID 26876110.
- ^ Svenningsson, Per (August 2019). "Corticobasal degeneration: advances in clinicopathology and biomarkers". Current Opinion in Neurology. 32 (4): 597–603. doi:10.1097/WCO.0000000000000707. ISSN 1350-7540.
- ^ a b c Alexander SK, Rittman T, Xuereb JH, Bak TH, Hodges JR, Rowe JB (August 2014). "Validation of the new consensus criteria for the diagnosis of corticobasal degeneration". J. Neurol. Neurosurg. Psychiatry. 85 (8): 925–29. doi:10.1136/jnnp-2013-307035. PMC 4112495. PMID 24521567.
- ^ Litvan I, Agid Y, Goetz C, Jankovic J, Wenning GK, et al. (January 1997). "Accuracy of the clinical diagnosis of corticobasal degeneration: a clinicopathologic study" (PDF). Neurology. 48 (1): 119–25. doi:10.1212/wnl.48.1.119. PMID 9008506. S2CID 30401542. Archived from the original (PDF) on 2011-07-16. Retrieved 2010-11-21.
- ^ a b c Scaravilli T, Tolosa E, Ferrer I (2005). "Progressive supranuclear palsy and corticobasal degeneration: Lumping versus splitting". Movement Disorders. 20: S21–S8. doi:10.1002/mds.20536. PMID 16092076. S2CID 21358152.
- ^ Jendroska K, Rossor MN, Mathias CJ, Daniel SE (January 1995). "Morphological overlap between corticobasal degeneration and Pick's disease: a clinicopathological report". Movement Disorders. 10 (1): 111–4. doi:10.1002/mds.870100118. PMID 7885345. S2CID 43288223.
- ^ a b c d e f g h Seritan AL, Mendez MF, Silverman DH, Hurley RA, Taber KH (2004). "Functional imaging as a window to dementia: Corticobasal degeneration". Journal of Neuropsychiatry and Clinical Neurosciences. 16 (4): 393–9. doi:10.1176/jnp.16.4.393. PMID 15616165.
- ^ Hassan A, Whitwell JL, Josephs KA (November 2011). "The corticobasal syndrome-Alzheimer's disease conundrum". Expert Review of Neurotherapeutics. 11 (11): 1569–78. doi:10.1586/ern.11.153. PMC 3232678. PMID 22014136.
- ^ Alladi S, Xuereb J, Bak T, Nestor P, Knibb J, et al. (October 2007). "Focal cortical presentations of Alzheimer's disease". Brain. 130 (10): 2636–45. doi:10.1093/brain/awm213. PMID 17898010.
- ^ Sha SJ, Ghosh PM, Lee SE, Corbetta-Rastelli C, Jagust WJ, et al. (March 2015). "Predicting amyloid status in corticobasal syndrome using modified clinical criteria, magnetic resonance imaging and fluorodeoxyglucose positron emission tomography". Alzheimer's Research & Therapy. 7 (1): 8. doi:10.1186/s13195-014-0093-y. PMC 4346122. PMID 25733984.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lang AE (2005). "Treatment of progressive supranuclear palsy and corticobasal degeneration". Movement Disorders. 20: S83–S91. doi:10.1002/mds.20545. PMID 16092096. S2CID 45848876.
- ^ a b c d Constantinides VC, Paraskevas GP, Paraskevas PG, Stefanis L, Kapaki E (August 2019). "Corticobasal degeneration and corticobasal syndrome: A review". Clinical Parkinsonism & Related Disorders. 1: 66–71. doi:10.1016/j.prdoa.2019.08.005. ISSN 2590-1125. PMC 8288513. PMID 34316603.
- ^ Fredericks CA, Lee SE (2016). "The cognitive neurology of corticobasal degeneration and progressive supranuclear palsy". In Miller, Bruce L.; Boeve, Bradley F. (eds.). The Behavioral Neurology of Dementia (Second ed.). Cambridge, United Kingdom: Cambridge University Press. pp. 203–6. ISBN 9781107077201. OCLC 934020279.
[CBD is] reminiscent of classic CBS but with executive function deficits
- ^ Gibb WR, Luthert PJ, Marsden CD (1989). "Corticobasal degeneration". Brain. 112 (5): 1171–1192. doi:10.1093/brain/112.5.1171. PMID 2478251.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Raynor Winn (2018) The Salt Path, Penguin Books.
- Boeve BF (2011). "The multiple phenotypes of corticobasal syndrome and corticobasal degeneration: Implications for further study". Journal of Molecular Neuroscience. 45 (3): 350–3. doi:10.1007/s12031-011-9624-1. PMID 21853287. S2CID 30307394.
- Hassan A, Whitwell JL, Josephs KA (2011). "The corticobasal syndrome-alzheimer's disease conundrum". Expert Review of Neurotherapeutics. 11 (11): 1569–78. doi:10.1586/ern.11.153. PMC 3232678. PMID 22014136.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Goode BL, Chau M, Denis PE, Feinstein SC (2000). "Structural and Functional Differences between 3-Repeat and 4-Repeat Tau Isoforms". Journal of Biological Chemistry. 275 (49): 38182–38189. doi:10.1074/jbc.m007489200. PMID 10984497. S2CID 30896096.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Mahapatra RK, Edwards MJ, Schott JM, Bhatia KP (2004). "Corticobasal degeneration". The Lancet Neurology. 3 (12): 736–43. doi:10.1016/s1474-4422(04)00936-6. PMID 15556806. S2CID 15324889. ProQuest 201513368.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Avila J (1992). "Microtubule functions". Life Sci. 50 (5): 327–334. doi:10.1016/0024-3205(92)90433-p. PMID 1732704.
