Dental abscess
| Dental abscess | |
|---|---|
| Specialty | Dentistry |
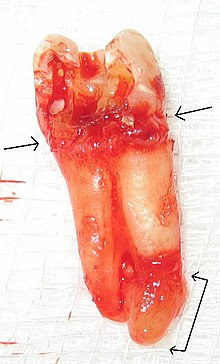
A dental abscess (also termed a dentoalveolar abscess, tooth abscess or root abscess), is a localized collection of pus associated with a tooth. The most common type of dental abscess is a periapical abscess, and the second most common is a periodontal abscess. In a periapical abscess, usually the origin is a bacterial infection that has accumulated in the soft, often dead, pulp of the tooth. This can be caused by tooth decay, broken teeth or extensive periodontal disease (or combinations of these factors). A failed root canal treatment may also create a similar abscess.
A dental abscess is a type of odontogenic infection, although commonly the latter term is applied to an infection which has spread outside the local region around the causative tooth.
Classification
The main types of dental abscess are:
- Periapical abscess: The result of a chronic, localized infection located at the tip, or apex, of the root of a tooth.[1]
- Periodontal abscess: begin in a periodontal pocket (see: periodontal abscess)
- Gingival abscess: involving only the gum tissue, without affecting either the tooth or the periodontal ligament (see: periodontal abscess)
- Pericoronal abscess: involving the soft tissues surrounding the crown of a tooth (see: Pericoronitis)
- Combined periodontic-endodontic abscess: a situation in which a periapical abscess and a periodontal abscess have combined (see: Combined periodontic-endodontic lesions).
Signs and symptoms

Symptoms from a dental abscess may range from light discomfort in the localized area to severe pain. The pain is continuous and may be described as extreme, growing, sharp, shooting, or throbbing. Putting pressure or warmth on the tooth may induce extreme pain. The area may be sensitive to touch and possibly swollen as well. This swelling may be present at either the base of the tooth, the gum, and/or the cheek, and sometimes can be reduced by applying ice packs.
An acute abscess may be painless but still have a swelling present on the gum. It is important to get anything that presents like this checked by a dental professional as it may become chronic later.
In some cases, a tooth abscess may perforate bone and start draining into the surrounding tissues creating local facial swelling. In some cases, the lymph glands in the neck will become swollen and tender in response to the infection. It may even feel like a migraine as the pain can transfer from the infected area. The pain does not normally transfer across the face, only upwards or downwards as the nerves that serve each side of the face are separate.
Severe aching and discomfort on the side of the face where the tooth is infected is also fairly common, with the tooth itself becoming unbearable to touch due to extreme amounts of pain.
Diagnostic approach
In order to diagnose a dental abscess thorough medical and dental histories must be taken, extraoral and intraoral examinations performed and radiographic images obtained. A periodontal abscess may be difficult to distinguish from a periapical abscess. Indeed sometimes they can occur together.[2] Since the management of a periodontal abscess is different from a periapical abscess, this differentiation is important to make. The following factors may help to this:
- If the swelling is over the area of the root apex, it is more likely to be a periapical abscess; if it is closer to the gingival margin, it is more likely to be a periodontal abscess.
- Similarly, in a periodontal abscess pus most likely discharges via the periodontal pocket, whereas a periapical abscess generally drains via a parulis nearer to the apex of the involved tooth.[2]
- If the tooth has pre-existing periodontal disease, with pockets and loss of alveolar bone height, it is more likely to be a periodontal abscess; whereas if the tooth with relatively healthy periodontal condition, it is more likely to be a periapical abscess.
- In periodontal abscesses, the swelling usually precedes the pain, and in periapical abscesses, the pain usually precedes the swelling.[2]
- A history of toothache with sensitivity to hot and cold suggests previous pulpitis, and indicates that a periapical abscess is more likely.
- If the tooth which gives normal results on pulp sensibility testing, is free of dental caries and has no large restorations; it is more likely to be a periodontal abscess.
- A dental radiograph is of little help in the early stages of an dental abscess, but later usually the position of the abscess, and hence indication of endodontal/periodontal etiology determined. If there is a sinus, a gutta percha point is sometimes inserted before the x-ray in the hope that it will point to the origin of the infection.
- Generally, periodontal abscesses will be more tender to lateral percussion than to vertical, and periapical abscesses will be more tender to apical percussion.[2]
Differential Diagnosis • On radiographs, cemento-osseous dysplasia and periapical dental abscesses have a similar manifestation. This is a condition where fibrous, cementum-like connective tissue replaces the bone in the maxilla or mandible in areas surrounding the tooth or in areas that previously contained teeth. A way to differentiate periapical abscesses from cemento-osseous dysplasia is to use percussion and/or a vitality test to determine the presence of an abscess. Also, if caries or previous restorations are present, this also is an indicator of possible dental abscess in comparison to cemento-osseous dysplasia. • Non-Hodgkin Lymphoma can occur in the oral cavity and can present clinically as a dental abscess. If patients fail to respond to conventional therapies, such as endodontic procedures, then the clinician needs to be on alert for a differential diagnosis. Not taking a biopsy could result in a delay in treatment of a neoplastic condition. This in turn could influence the overall prognosis and outcome.(9) • Plasmacytomas exhibit bucco-palatal swelling, expansion, well-defined margins and a smooth surface; the swelling can cause nasal obstruction and epistaxis. Radiographs show a hazy radiolucent area. Once blood work is done and no abnormalities are found a histological analysis has to be performed. The analysis shows sheet-like proliferations at different levels of maturity with atypic cells that mimic cartwheels. The blood work, atypic histopathology, and radiographs all need to be utilized to accurately differentiate between a plasmacytoma and a dental abscess.(10)
Treatment
Successful treatment of a dental abscess centers on the reduction and elimination of the offending organisms. This can include treatment with antibiotics[3] and drainage. If the tooth can be restored, root canal therapy can be performed. Non-restorable teeth must be extracted, followed by curettage of all apical soft tissue.
Unless they are symptomatic, teeth treated with root canal therapy should be evaluated at 1- and 2-year intervals after the root canal therapy to rule out possible lesional enlargement and to ensure appropriate healing.
Abscesses may fail to heal for several reasons:
- Cyst formation
- Inadequate root canal therapy
- Vertical root fractures
- Foreign material in the lesion
- Associated periodontal disease
- Penetration of the maxillary sinus
Following conventional, adequate root canal therapy, abscesses that do not heal or enlarge are often treated with surgery and filling the root tips; and will require a biopsy to evaluate the diagnosis.[4]
Untreated consequences

If left untreated, a severe tooth abscess may become large enough to perforate bone and extend into the soft tissue eventually becoming osteomyelitis and cellulitis respectively. From there it follows the path of least resistance and may spread either internally or externally. The path of the infection is influenced by such things as the location of the infected tooth and the thickness of the bone, muscle and fascia attachments.
External drainage may begin as a boil which bursts allowing pus drainage from the abscess, intraorally (usually through the gum) or extraorally. Chronic drainage will allow an epithelial lining to form in this communication to form a pus draining canal (fistula). Sometimes this type of drainage will immediately relieve some of the painful symptoms associated with the pressure.
Internal drainage is of more concern as growing infection makes space within the tissues surrounding the infection. Severe complications requiring immediate hospitalization include Ludwig's angina, which is a combination of growing infection and cellulitis which closes the airway space causing suffocation in extreme cases. Also infection can spread down the tissue spaces to the mediastinum which has significant consequences on the vital organs such as the heart. Another complication, usually from upper teeth, is a risk of septicaemia (infection of the blood) from connecting into blood vessels, brain abscess (extremely rare), or meningitis (also rare).
Depending on the severity of the infection, the sufferer may feel only mildly ill, or may in extreme cases require hospital care.
Society and culture
In 2011, Kyle Willis died from an untreated dental abscess in Cincinnati,[5] as did fashion designer Hugo Boss, in 1948.[6]
See also
References
- ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Kathleen FM Fan, Judith Jones (2009). OSCEs for dentistry (2nd ed., new and updated. ed.). 2nd: PasTest Ltd. p. 68. ISBN 9781905635504.
{{cite book}}: CS1 maint: location (link) - ^ http://www.cks.nhs.uk/dental_abscess/management/detailed_answers/waiting_to_see_a_dental_practitioner/recommended_antibiotic
- ^ Neville, Brad W. ; et al. (1995). Oral and Maxillofacial Pathology (1st ed.). Saunders. pp. 104–5. ISBN 9781416034353.
{{cite book}}: Explicit use of et al. in:|author=(help) - ^ Gann, Carrie. "Man Dies From Toothache, Couldn't Afford Meds". ABC News. ABC News. Retrieved 20 January 2012.
- ^ http://www.metzingen-zwangsarbeit.de/Kober-Studie/7_Die_Firma_Hugo_Boss/body_7_die_firma_hugo_boss.html
