Chronic granulomatous disease
In medicine (genetics and pediatrics) chronic granulomatous disease (CGD) is a diverse group of hereditary diseases in which certain cells of the immune system have difficulty forming the reactive oxygen compounds used to kill certain ingested pathogens. This leads to the formation of granulomata in many organs[1]. CGD affects about 1 in 200,000 people in the United States, with at least 20 new cases diagnosed each year.
This condition was first described in 1959 as "a fatal granulomatosis of childhood"[2]. The underlying cellular mechanism that causes chronic granulomatous disease was discovered in 1967, and reasearch since that time has further elucidated the molecular mechanisms underlying the disease[3].
Pathophysiology

Phagocytes (i.e., neutrophils, eosinophils, monocytes, and macrophages) require a set of enzymes to produce reactive oxygen species to destroy bacteria after they ingest the bacteria in a process called phagocytosis. Together these enzymes are termed "phagocyte NADPH oxidase" (PHOX). The reactive oxygen compounds these enzymes produce are toxic to bacteria and help the phagocyte kill them once they are ingested. Defects in one of these enzymes can all cause CGD of varying severity, dependent on the defect. There are over 410 known possible defects in the PHOX enzyme complex that can lead to chronic granulomatous disease[1].
Genetics
Four genes have been implicated in CGD (p is the weight of the protein in kDa; the g means glycoprotein)[1]:
- CYBB, coding the gp91-phox subunit (X-linked, accounts for 2/3 of the cases);
- CYBA, coding p22-phox
- NCF-1, coding p47-phox
- NCF-2, coding p67-phox
- A fifth gene, coding for p40-phox, has not been implicated
A low level of NADPH, the cofactor required for superoxide synthesis, can lead to CGD. This has been reported in women who are homozygous for the genetic defect causing glucose-6-phosphate dehydrogenase deficiency (G6PD), which is characterised by reduced NADPH levels.
X-linked Chronic Granulomatous disease: defect in membrane NADPH oxidase. Autosomal Recessive Chronic Granulomatous disease: defect in cytoplasmic NADPH oxidase.
Clinical manifestations
Classically, patients with chronic granulomatous disease will suffer from recurrent bouts of infection due to the decreased capacity of their immune system to fight off disease-causing organisms. The recurrent infections they acquire are specific and are, in decreasing order of frequency:
- pneumonia
- abscesses of the skin, tissues, and organs
- suppurative arthritis
- osteomyelitis
- bacteremia/fungemia
- superficial skin infections such as cellulitis or impetigo
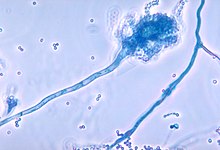
People with CGD are sometimes infected with unique organisms that usually do not cause disease in people with normal immune systems. Some of the organisms that cause disease in CGD patients are Staphylococcus aureus, Escheria coli, Klebsiella species, Aspergillus species, and Candida species.
Aspergillus has a unique propensity to cause infection in people with CGD. Of the Aspergillus species, Aspergillus fumigatus seems to be the one that most commonly causes disease. Thus, CGD should be considered as a diagnosis in patients with an Aspergillus infection whose cause in unknown.
Most people with CGD are diagnosed in childhood, usually before age 5 [4]. Early diagnosis is important since these people can be placed on antibiotics to ward off infections before they occur.
Laboratory findings
The nitroblue-tetrazolium test (NBT) is the original and most widely-known test for chronic granulomatous disease. This test is simple to perform and gives rapid results, but only tells whether or not there is a problem with the PHOX enzymes, not how much they are affected. An advanced test called the cytochrome C reduction assay tells physicians how much oxygen radicals a patient's phagocytes are capable of producing. Once the diagnosis of CGD is established, a genetic analysis may be used to determine exactly which mutation is the underlying cause.
Treatment
Management of chronic granulomatous disease revolves around two goals: 1) diagnose the disease early so that antibiotics can be given to keep an infection from occurring, and 2) educate the patient about his or her condition so that prompt treatment can be given if an infection occurs.
Physicians often prescribe the antibiotic trimethoprim-sulfamethoxazole to prevent bacterial infections[5]. This drug also has the benefit of sparing the normal bacteria of the digestive tract. Fungal infection is commonly prevented with itraconazole[6], although a newer drug of the same type called voriconazole may be more effective[7]. The use of this drug for this purpose is still under scientific investigation.
Interferon, in the form of interferon gamma-1b (Actimmune®) is approved by the Food and Drug Administration for the prevention of CGD. It has been shown to prevent infections in CGD patients by 70% and to reduce their severity. Although its exact mechanism is still not entirely understood, it has the ability to give CGD patients more immune function and therefore, greater ability to fight off infections. This therapy has been standard treatment for CGD for several years[8].
A 2006 study[9] suggested that gene therapy had been successful in two cases (men ages 16 and 25). One has since died in April 2006 [10]
Prognosis
The prognosis of chronic granulomatous disease is guarded, with long-term outcomes closely tied to early diagnosis and eary therapeutic intervention. With increasing treatment options for CGD the life-span for these patients is expected to also increase.
References
- ^ a b c Heyworth PG, Cross AR, Curnutte JT. Chronic granulomatous disease. Curr Opin Immunol 2003;15:578–584. PMID 14499268.
- ^ Bridges ,RA, Berendes ,H, Good, RA. A fatal granulomatosis of childhood: the clinical, pathological, and laboratory features of a new syndrome. AMA J Dis Child 1959; 97:387.
- ^ Baehner, RL, Nathan, DG. Leukocyte oxidase: a defective activity in chronic granulomatous disease. Science 1967; 155:835.
- ^ Winkelstein, JA, Marino, MC, Johnson, RB Jr, et al. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine (Baltimore) 2000; 79:155
- ^ Weening, RS, Kabel, P, Pijman, P, Roos, D. Continuous therapy with sulfamethoxazole-trimethoprim in patients with chronic granulomatous disease. J Pediatrics 1983; 103:127.
- ^ Cale, CM, Jones, AM, Goldblatt, D. Follow up of patients with chronic granulomatous disease diagnosed since 1990. Clin Exp Immunol 2000; 120:351.
- ^ Sabo, JA, Abdel-Rahman, SM. Voriconazole: a new triazole antifungal. Ann Pharmacother 2000; 34:1032.
- ^ A controlled trial of interferon gamma to prevent infection in chronic granulomatous disease. The International Chronic Granulomatous Disease Cooperative Study Group. N Engl J Med 1991;324:509-16. PMID 1846940
- ^ Ott MG, Schmidt M, Schwarzwaelder K, Stein S, Siler U, Koehl U, Glimm H, Kuhlcke K, Schilz A, Kunkel H, Naundorf S, Brinkmann A, Deichmann A, Fischer M, Ball C, Pilz I, Dunbar C, Du Y, Jenkins NA, Copeland NG, Luthi U, Hassan M, Thrasher AJ, Hoelzer D, von Kalle C, Seger R, Grez M. Correction of X-linked chronic granulomatous disease by gene therapy, augmented by insertional activation of MDS1-EVI1, PRDM16 or SETBP1. Nat Med 2006;12:401-9. PMID 16582916.
- ^ Abbott A. Scientists investigate gene-therapy death. http://www.nature.com/news/2006/060424/pf/060424-14_pf.html
