Evidence-based dentistry
This article needs additional citations for verification. (April 2019) |
| Part of a series on |
| Evidence-based practices |
|---|
|
|
Evidence-based dentistry (EBD) is the dental part of the more general movement toward evidence-based medicine and other evidence-based practices. The pervasive access to information on the internet includes different aspects of dentistry for both the dentists and patients. This has created a need to ensure that evidence referenced to are valid, reliable and of good quality.[1]
Evidence-based dentistry has become more prevalent than ever, as information, derived from high-quality, evidence-based research is made available to clinicians and patients in clinical guidelines. By formulating evidence-based best-practice clinical guidelines that practitioners can refer to with simple chairside and patient-friendly versions, this need can be addressed.
Evidence-based dentistry has been defined by the American Dental Association (ADA) as "an approach to oral healthcare that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient's oral and medical condition and history, with the dentist's clinical expertise and the patient's treatment needs and preferences."[2]
Three main pillars or principles[3] exist in evidence-based dentistry. The three pillars are defined as:
- Relevant scientific evidence
- Patient needs and preferences
- Clinician's expertise
The use of high-quality research to establish the guidelines for best practices defines evidence-based practice. In essence, evidence-based dentistry requires clinicians to remain constantly updated on current techniques and procedures so that patients can continuously receive the best treatment possible.
History
Evidence-based dentistry (EBD) was first introduced by Gordon Guyatt and the Evidence-Based Medicine Working Group at McMaster University in Ontario, Canada in the 1990s as part of the larger movement toward evidence-based medicine and other evidence-based practices.
Clinical Decision Making
Much praise has gone to the dentistry approach of clinical decision making. In an EB case report written by Miller SA, is focused on the “use of evidence-based decision-making in private practice for emergency treatment of dental trauma”. The case concludes with high praise for this method, going as far to say that “[the] evidence-based method was efficient, and very helpful in optimizing the management of the emergency dental treatment”.[4] However, it is important to ensure that the collection of data in the evidence during evidence-based clinical decision making isn’t corrupted. Crawford JM writes about publication bias, as well as the possible effects it can have on evidence-based clinical making. He writes that it is important to watch out for publication bias, as it can “hinder advancements in oral health care by decreasing the availability of scientific evidence and threatening the validity of evidence-based practice”.[5]
There are many tools that have been developed for dental-based clinical decision making. Authors Rios Santos JV, Castello Castaneda C, and Bullon P all documented the “development of a computer application to help the decision making process in teaching dentistry.” It offers the ability to review information, to help reinforce information that is learned by students. Teaching staff can also “design any theme they wish, increasing the efficiency and support capabilities of the program”.[6]
Principles
In summary, there are three main pillars[7] exist in Evidence-based dentistry which serves as its main principles. The three pillars are defined as:
- Dentists' clinical expertise
- Patient needs and preferences
- Relevant scientific evidence
Dentists' clinical expertise
Much less attention is paid to both the other two spheres of Evidence Based Dentistry; clinical expertise and patient values.[8]
Clinical expertise plays a part in the successful outcomes of treatment with diagnostic skills preventing over and under-treatments, technical dental skills maximizing the longevity of surgical and restorative procedures and communication skills being core to patient management and perceived success.
Patients needs and preferences
Not all patients have the same priorities for their care. Understanding patient's individual needs, wants and circumstances gives the clinician a place from which to discuss treatment options available with the patient. This might be competing priorities between dentists/ therapists/ hygienists who generally aim for longevity and aesthetics and patients who may be more interested in keeping costs down, aesthetics or would prefer less invasive treatments.
Relevant scientific evidence
Given that "Patient needs and preferences" and "Dentist's clinical expertise" are variable and will differ among numerous clinicians and population, "Relevant scientific evidence" is of critical importance. Therefore, it is imperative that information referenced to are derived from high-quality, evidence-based research, which can be used to establish the guidelines for providing the best practices.
In essence, Evidence-based dentistry can allow clinicians to remain constantly updated on the newest techniques and procedures so that patients can continuously receive the best treatment possible.
Evidence based process
Best scientific evidence
The new model set by EBM uses a systematic process to incorporate current research into practice. The evidence-based process requires the practitioner to develop five key skills:
- Formulate information needs/questions into four part questions to identify the patient/problem (P), intervention (I), comparison (C), and outcomes (O), known mnemonically as the PICO questions.
- Conduct an efficient computerized search of the literature for the appropriate type and level of evidence.
- Critically appraise the evidence for validity with an understanding of research methods.
- Apply the results of the evidence to patient care or practice in consideration for the patient's preferences, values and circumstances.
- Evaluate the process and your performance through self-evaluation.[9]
The American Dental Association defined evidence-based dentistry like so:
Evidence-based dentistry (EBD) is an approach to oral health care that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient's oral and medical condition and history, with the dentist's clinical expertise and the patient's treatment needs and preferences.
— ADA[10]
The American Dental Education Association (ADEA) has incorporated the definition of evidence-based dentistry into core competencies required by dental education programs. These competencies focus on graduates to become lifelong learners and consumers of current research findings and require students to develop skills that are reflective of evidence-based dentistry.[11]
A dentist's learning curve for using the evidence-based process can be steep, but there are continuing education courses, workbooks and tools available to simplify the integration of current research into practice.
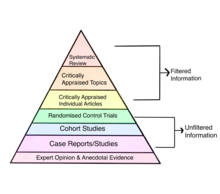
Assessing the quality of evidence
Need for continuing education
Dental Graduates around the globe are, possibly up to date at the time they graduate but usually are fundamentally lacking in the understanding of trials/studies design and relevance/importance. Dental speciality training, however stresses evidence ~based outcomes results and methodologies. But this becomes out of date as new information and technology appear. Hence it is important, especially with regards to patient safety, for dentists to be able to keep up to date with developments. Having an understanding of how to interpret research results, and some practice in reading the literature in a structured way, can turn the dental literature into a useful and comprehensible practice tool. For this to happen, EBD learning absolutely needs to be at the heart of dental education. Dental students can be taught EBD concept during their time in dental school so that they will develop the ability to evaluate critically new knowledge and determine its relevance to the clinical problems and challenges presented by the individual patient. They also acquire the ability to interpret, assess, integrate, and apply data and information in the process of clinical problem solving, reasoning, and decision making. EBD is a life long learning process and help to develop ability to learn independently.
Organisations that develop evidence-based guidelines and policies
Scottish Intercollegiate Guidelines Network
Formed in 1993, the Scottish Intercollegiate Guidelines Network (SIGN) goals are to decrease the discrepancy in treatments and results, through the creation and dissemination of nation-wide clinical guidelines encompassing recommendations for effective practice established on up-to-date evidence to improve the quality of health care for patients in Scotland.[13]
SIGN guidelines are established using a clear methodology[14] constructed on three fundamental principles, which are:
- Development is carried out by multidisciplinary, nationwide representative groups
- A systematic review is conducted to recognise and analytically evaluate the evidence
- Recommendations are clearly connected to the supporting evidence
As of 2009, SIGN has also adopted the practise of implementing[15] the GRADE methodology to all its SIGN guidelines.
Scottish Dental Clinical Effectiveness Programme
Part of NHS Education for Scotland (NES), the Scottish Dental Clinical Effectiveness Programme (SDCEP)[16] is an initiative of the National Dental Advisory Committee (NDAC) which is an organisation of dental professionals, across all specialities, that functions as consultative wing to the Chief Dental Officer. Its main goal is to appraise the best available and pertinent information with regards to dentistry and convert it into guidelines which are easily comprehensible and executable.
The Scottish Dental Clinical Effectiveness Programme consist of a central group for Programme Development and multiple other groups for guideline development. With
the principal objective of developing guidance that delivers the best quality of patient care through supporting dental teams, the Scottish Dental Clinical Effectiveness Programme uses the most suitable high-quality evidences from a plethora of sources to make guidelines recommendations.
Founded under the intention of the National Dental Advisory Committee (NDAC) to give a systematized methodology[17] when providing clinical guidance for the dental profession, the Scottish Dental Clinical Effectiveness Programme has since become a crucial factor between the gold standard practice guidelines and dental education and practice.
Limitations and Criticism
Despite the high praise for evidence-based dentistry, there are a number of limitation and criticism that has been given to the process. Chambers DW provides quite a bit of criticism, as well as a number of limitations that evidence-based dentistry provides. In no particular order of importance, a number of mentioned objections towards this format are:
- Evidence-based dentistry is too clumsy due to the concept being poorly defined
- The implementation of evidence-based dentistry has been distorted by too heavy of an emphasis of computerized searches for research findings that meet the standards of academics
- Although EBD advocates enjoy sharing anecdotal accounts of mistakes others have made, faulting others is not proof that one's own position is correct
- There is no systematic, high-quality evidence that EBD is effective
- Patient and practitioner values are the shortest leg of the stool. As they are so little recognized, their integration in EBD is problematic and ethical tensions exist where paternalism privileges science over patient's self-determined best interests.[18]
Literature
Evidence-based dental journals have been developed as resources for busy clinicians to aid in the integration of current research into practice. These journals publish concise summaries of original studies as well as review articles. These critical summaries, consist of an appraisal of original research, with discussion of the relevant, practical information of the research study.
Systematic reviews are also helpful for the busy practitioner because they combine the results of multiple studies that have investigated the same specific phenomenon or question.
References
- ^ Dhar V (2016). "Evidence-based dentistry: An overview". Contemporary Clinical Dentistry. 7 (3): 293–4. doi:10.4103/0976-237X.188539. PMC 5004537. PMID 27630488.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Ismail AI, Bader JD (January 2004). "Evidence-based dentistry in clinical practice". Journal of the American Dental Association. 135 (1): 78–83. doi:10.14219/jada.archive.2004.0024. PMID 14959878.
- ^ "About EBD". ebd.ada.org. Retrieved 2020-02-19.
- ^ Miller SA, Miller G (September 2010). "Use of evidence-based decision-making in private practice for emergency treatment of dental trauma: EB case report". The Journal of Evidence-Based Dental Practice. 10 (3): 135–46. doi:10.1016/j.jebdp.2009.12.004. PMID 20797655.
- ^ Chiappelli F (2010). "Future Avenues of Research Synthesis for Evidence-Based Clinical Decision Making". Evidence-Based Practice: Toward Optimizing Clinical Outcomes. Springer Berlin Heidelberg. pp. 243–247. doi:10.1007/978-3-642-05025-1_15. ISBN 978-3-642-05024-4.
- ^ Castañeda E, Garmendia L, Santos M (October 2009). "Desing of an Intelligent System for Computer Aided Musical Composition". Intelligent Decision Making Systems. World Scientific: 13–18. doi:10.1142/9789814295062_0002. ISBN 978-981-4295-05-5.
- ^ "About EBD". Center for Evidence-Based Dentistry (EBD). American Dental Association. Retrieved 6 November 2019.
- ^ Innes NP, Schwendicke F, Lamont T (June 2016). "How do we create, and improve, the evidence base?" (PDF). British Dental Journal. 220 (12): 651–5. doi:10.1038/sj.bdj.2016.451. PMID 27338909.
- ^ Straus S, Glasziou P, Richardson WS, Haynes RB (April 2018). Evidence-Based Medicine: How to Practice & Teach EBM (5th ed.). London, England: Churchill Livingston. ISBN 978-0-7020-6297-1.
- ^ "ADA Policy Statement on Evidence-based Dentistry". American Dental Association. Retrieved 17 August 2010.
- ^ "ADEA Competencies for the New General Dentist: (As approved by the 2008 ADEA House of Delegates)" (PDF). Journal of Dental Education. 81 (7): 844–847. July 2017. PMID 28668789.
- ^ Ingham-Broomfield R (March 2016). "A nurses' guide to the hierarchy of research designs and evidence" (PDF). The Australian Journal of Advanced Nursing. 33 (3): 38.
- ^ "Who we are". Scottish Intercollegiate Guidelines Network (SIGN). Retrieved 6 November 2019.
- ^ "What we do". Healthcare Improvement Scotland. Retrieved 6 November 2019.
- ^ "Applying the GRADE Methodology to SIGN Guidelines: Core Principles" (PDF). Scottish Intercollegiate Guidelines Network (SIGN). Scotland NHS.
- ^ "Background". Scottish Dental Clinical Effectiveness Programme (SDCEP). Retrieved 6 November 2019.
- ^ "What We Do". Scottish Dental Clinical Effectiveness Programme (SDCEP). Retrieved 6 November 2019.
- ^ Richards D (December 2010). "Questions and answers in Evidence-based Dentistry volume 11". Evidence-Based Dentistry. 11 (4): 119–122. doi:10.1038/sj.ebd.6400762. ISSN 1462-0049.
Further reading
- Afrashtehfar KI, Assery MK (July 2017). "From dental science to clinical practice: Knowledge translation and evidence-based dentistry principles". review. The Saudi Dental Journal. 29 (3): 83–92. doi:10.1016/j.sdentj.2017.02.002. PMC 5503095. PMID 28725125.
- Chiappelli F (March 2019). "Evidence-Based Dentistry: Two Decades and Beyond". review. The Journal of Evidence-Based Dental Practice. 19 (1): 7–16. doi:10.1016/j.jebdp.2018.05.001. PMID 30926103.
- Clarkson J, Worthington H (August 2019). "Leadership in evidence based dentistry" (PDF). review. Journal of Dentistry. 87: 16–19. doi:10.1016/j.jdent.2019.05.012. PMID 31075375.
- Fontana M, Gonzalez-Cabezas C (January 2019). "Evidence-Based Dentistry Caries Risk Assessment and Disease Management". review. Dental Clinics of North America. 63 (1): 119–128. doi:10.1016/j.cden.2018.08.007. PMID 30447787.
- France K, Sollecito TP (January 2019). "How Evidence-Based Dentistry Has Shaped the Practice of Oral Medicine". review. Dental Clinics of North America. 63 (1): 83–95. doi:10.1016/j.cden.2018.08.006. PMID 30447794.
- Lang LA, Teich ST (June 2014). "A critical appraisal of evidence-based dentistry: the best available evidence". review. The Journal of Prosthetic Dentistry. 111 (6): 485–92. doi:10.1016/j.prosdent.2013.12.001. PMID 24589122.
