Healthcare in New Zealand
The health care system of New Zealand has undergone significant changes throughout the past several decades. From an essentially fully public system in the early 20th century, reforms have introduced market and health insurance elements primarily in the last three decades, creating a mixed public-private system for delivering healthcare.
- The Accident Compensation Corporation covers the costs of treatment for cases deemed 'accidents', including medical misadventure, for all people legally in New Zealand (including tourists). The costs are recovered via levies on employers, employees, petrol and vehicle registration, and contributions from the general tax pool.
- The relatively extensive and high-quality system of public hospitals treats citizens or permanent residents free of charge and is managed by District Health Boards. However, costly or difficult operations often require long waiting list delays unless the treatment is medically urgent.[1] Because of this, a secondary market of health insurance schemes exists which fund operations and treatments for their members privately. Southern Cross Health Insurance, a non-profit-scheme, is the largest of these at about 60% of the health insurance market and covering almost a quarter of all New Zealanders in 2007, even operating its own chain of hospitals.[2]
- Primary care (non-specialist doctors / family doctors) and medications on the list of the New Zealand government agency PHARMAC require co-payments, but are subsidised, especially for patients with community health services cards or high user health cards.
- Emergency services are primarily provided by St. John New Zealand charity (as well as Wellington Free Ambulance in the Wellington Region), supported with a mix of private (donated) and public (subsidy) funds.
In 2012, New Zealand spent 8.7% of GDP on health care, or US$3,929 per capita. Of that, approximately 77% was government expenditure.[3] In a 2010 study, New Zealand came last in a study for the level of medications use in 14 developed countries (i.e. used least medicines overall), and also spent the lowest amount on healthcare amongst the same list of countries, with US$2510 ($3460) per capita, compared to the United States at US$7290.[4]
Structure
The Ministry of Health is responsible for the oversight and funding of the twenty District Health Boards (DHBs). These are responsible for organizing healthcare in the district and meeting the standards set by the Ministry of Health. Twenty-one DHBs came into being on January 1, 2001 with Southland and Otago DHBs merging into Southern DHB on 1 May 2010.
The boards for each DHB are elected in elections held every three years, with the exception of one of the eight board members, who is appointed by the Ministry of Health.
The DHBs oversee the forty six Primary Health Organizations established throughout the country. These were first set up in July, 2002, with a mandate to focus on the health of communities. Originally there were 81 of these, but this has been reduced down to 46 in 2008. They are funded by DHBs, and are required to be entirely non-profit, democratic bodies that are responsive to their communities' needs. Almost all New Zealanders are enrolled in a PHO, as there are financial incentives for the patients to become enrolled.
The Northern Region DHBs also use shared services provided by the Northern DHB Support Agency and HealthAlliance. These services deliver region wide health initiatives and shared IT services and logistics.
The Canterbury District health board has been successful in redesigning services to reduce hospital use. Some of this transformation was precipitated by the 2011 Christchurch earthquake when several healthcare buildings were damaged or destroyed. It now has lower rates of acute medical admissions, low rates of average length of stay, fewer readmissions in acute care, fewer cancelled planned admissions and more conditions treated out of hospital.[5]
Public vs. private payment
Hospital and specialist care in New Zealand is totally covered by the government if the patient is referred by a general or family practitioner and this is funded from government expenditure (approx. 77%).[3] Private payment by individuals also plays an important role in the overall system although the cost of these payments are comparatively minor. Those earning less than certain amounts, depending on the number of dependents in their household, can qualify for a Community Services Card (CSC). This reduces the cost of after-hours doctors' visits, and prescription fees, but no longer reduces the cost of visits to a person's regular doctor.
Injuries which occur as a result of "accidents", ranging from minor to major physical but including psychological trauma from sexual abuse are generally covered by the Accident Compensation Corporation (ACC). This may include coverage for doctors visits and lump-sum payments.
Access
In 2016, concerns were raised about phantom waiting lists - for people who needed surgery but were not on a waiting list.[6] Research conducted on behalf of the Health Funds Association of New Zealand and the New Zealand Private Surgical Hospitals Association found that out of 280,000 people waiting for surgery, only 110,000 were on an official waiting list and 170,000 had not been placed on a list despite being told they required surgery. Health Funds Association chief executive Roger Styles said "Of particular concern is the increase observed in overall waiting times" which for public surgery is now an average of 304 days.[7]
Health statistics
The following statistics are a sample from the World Health Organization Statistical Information System (WHOSIS). The year on which the data were sampled follows the statistic in brackets.
- Demographics
- Population (in thousands): 4,460 (2012)
- Total fertility rate (per woman): 2.07 (2012)
- Adolescent fertility rate (%): 27 (2004)
- Funding
- Life expectancy
- Life expectancy at birth (years): 82 (2012)
- Life expectancy for females (years): 84 (2012)
- Life expectancy for males (years): 80 (2012)
- Neonatal mortality (per 1,000 live births): 3 (2012)
- Infant mortality (per 1,000 live births): 5 (2012)
- Years of life lost to communicable diseases (%): 5 (2002)
- Years of life lost to injuries (%): 17 (2002)
- Years of life lost to non-communicable diseases (%): 79 (2002)
Abortion
Abortion is legal in New Zealand, if certain criteria are met. In general, either the health of the pregnant woman or the foetus must be in jeopardy. Additionally, two doctors must give their consent to the procedure. There were 18,380 abortions carried out in 2007, following a general increase in both the absolute number and per capita rate since 1991.
Medications
The Pharmaceutical Management Agency of New Zealand (PHARMAC) was set up in 1993 to decide which medications the government will subsidise. In general, PHARMAC will select an effective and safe medication from a class of drugs, and negotiate with the drug manufacturer to obtain the best price. There are approximately 2,000 drugs listed on the national schedule that are either fully or partially subsidised.
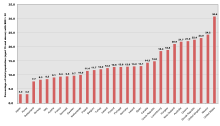
In a sample of 13 developed countries New Zealand was thirteenth in its population weighted usage of medication in 14 classes in 2009 and also in 2013. The drugs studied were selected on the basis that the conditions treated had high incidence, prevalence and/or mortality, caused significant long-term morbidity and incurred high levels of expenditure and significant developments in prevention or treatment had been made in the last 10 years. The study noted considerable difficulties in cross border comparison of medication use.[8]
Emergency service
Outside the Wellington Region, Emergency and non-urgent ambulance transportation is carried out by the charitable organization St. John New Zealand. In Greater Wellington Region ambulance services are provided by the Wellington Free Ambulance organisation.
See also
References
- ^ "OECD iLibrary: Statistics / Health at a Glance / 2011 / Waiting time of four months or more for elective surgery". Organisation for Economic Cooperation and Development (OECD). Retrieved 2012-12-27.
- ^ Hudson, Alice (14 October 2007). "Health cover under the knife". The New Zealand Herald. Retrieved 2 October 2011.
- ^ a b "WHO Statistical Information System". World Health Organization. Retrieved 2008-09-23.
- ^ Johnston, Martin (30 July 2010). "NZ ranks last in medicine use and lowest health spender". The New Zealand Herald. Retrieved 30 July 2010.
- ^ "International examples of prudent approaches to healthcare". Public health Wales. Prudent Healthcare. Retrieved 11 July 2015.
- ^ "Who is missing out on surgery? Government releases first figures of 'phantom waiting list'".
- ^ "Thousands missing out on surgery, funding boost fails to make dent in 'phantom waitlists'".
- ^ Office of health Economics. "International Comparison of Medicines Usage: Quantitative Analysis" (PDF). Association of the British Pharmaceutical Industry. Retrieved 2 July 2015.
Further reading
- Gerritsen, Sarah; Niki Stefanogiannis; Yvonne Galloway (2008). A portrait of health key results of the 2006/07 New Zealand health survey (PDF). Wellington, N.Z.: Ministry of Health. ISBN 978-0-478-31741-1. Retrieved 2012-01-21.
