Perineural invasion
In pathology, perineural invasion, abbreviated PNI, refers to cancer spreading to the space surrounding a nerve. It is common in head and neck cancer, prostate cancer and colorectal cancer.
Significance
Cancers with PNI usually have a poorer prognosis,[1] as PNI is thought to be indicative of perineural spread, which can make resection of malignant lesions more difficult.
Prostate cancer
In prostate cancer, PNI in needle biopsies is poor prognosticator;[1] however, in prostatectomy specimens it is unclear whether it carries a worse prognosis.[2]
In one study, PNI was found in approximately 90% of radical prostatectomy specimens, and PNI outside of the prostate, especially, was associated with a poorer prognosis.[3] However, there exists controversies about whether PNI has prognostic significance toward cancer malignancy.
Additional images
-
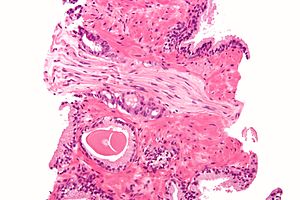
Micrograph demonstrating perineural invasion. HPS stain.
See also
References
- ^ a b Potter, SR.; Partin, AW. (2000). "The significance of perineural invasion found on needle biopsy of the prostate: implications for definitive therapy". Rev Urol. 2 (2): 87–90. PMC 1476100. PMID 16985741.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Bostwick, DG.; Foster, CS. (Nov 1999). "Predictive factors in prostate cancer: current concepts from the 1999 College of American Pathologists Conference on Solid Tumor Prognostic Factors and the 1999 World Health Organization Second International Consultation on Prostate Cancer". Semin Urol Oncol. 17 (4): 222–72. PMID 10632123.
- ^ Merrilees, AD.; Bethwaite, PB.; Russell, GL.; Robinson, RG.; Delahunt, B. (Sep 2008). "Parameters of perineural invasion in radical prostatectomy specimens lack prognostic significance". Mod Pathol. 21 (9): 1095–100. doi:10.1038/modpathol.2008.81. PMID 18500264.

