Rectouterine pouch
| Recto-uterine pouch | |
|---|---|
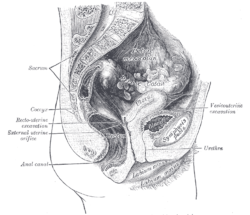
 Sagittal section of the lower part of a female trunk, right segment. (Excavatio recto-uterina labeled at bottom right.) | |
 Median sagittal section of female pelvis. (Rectouterine excavation labeled at center left.) | |
| Details | |
| Identifiers | |
| Latin | excavatio rectouterina, cavum douglassi, fossa douglasi |
| MeSH | D004312 |
| TA98 | A10.1.02.512F |
| TA2 | 3726 |
| FMA | 14728 |
| Anatomical terminology | |
The recto-uterine pouch (or rectouterine excavation, rectovaginal, Ehrhardt-Cole Recess, cul-de-sac, cavum Douglasi or Pouch of Douglas) is the extension of the peritoneal cavity between the rectum and the posterior wall of the uterus in the female human body.
Structure and physiology
In women it is the deepest point of the peritoneal cavity, posterior to (behind) the uterus and anterior to (in front of) the rectum. (The pouch on the other side of the uterus is the vesico-uterine pouch.) It is near the posterior fornix of the vagina.
It is normal to have approximately 1 to 3 ml (or mL) in the recto-uterine pouch throughout the menstrual cycle.[1] After ovulation there is between 4 and 5 ml of fluid in the recto-uterine pouch.[1]
In men, the region corresponding to the recto-uterine pouch is the recto-vesical pouch, which lies between the urinary bladder and rectum. (There is no equivalent to the vesico-uterine pouch).
Pathology
The recto-uterine pouch, being the lowest part of the peritoneal cavity in a woman at supine position, is a common site for the spread of pathology such as ascites, tumour, endometriosis, pus, etc.
Naming and etymology
It is also known by the names Douglas pouch, Douglas cavity, Douglas space and Douglas cul-de-sac.[2]
It is named after the Scottish anatomist Dr. James Douglas (1675–1742) who extensively explored this region of the female body. Three other nearby anatomical structures are also named for him - the Douglas fold, the Douglas line and the Douglas septum.
Culdotomy
A culdotomy incision or needle puncture of this "cul-de-sac" pouch by way of the vagina.
Clinical significance
As it is the furthest point of the abdominopelvic cavity in women, it is a site where infection and fluids typically collect.[3]
The recto-uterine pouch is used in the treatment of end-stage renal failure in patients who are treated by peritoneal dialysis. The tip of the dialysis catheter is placed into the deepest point of the pouch.
Additional images
-
The epiploic foramen, greater sac or general cavity (red) and lesser sac, or omental bursa (blue).
-
Illu female pelvis
See also
References
- ^ a b Severi FM, Bocchi C, Vannuccini S, Petraglia F (2012). "Ovary and ultrasound: from physiology to disease" (PDF). Archives of Perinatal Medicine. 18 (1): 7–19.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ synd/2937 at Who Named It?
- ^ Drake, RL (2010). Gray's Anatomy for Students. Churchill Livingstone. p. 460.
Further reading
- Gullmo A (1980). "Herniography. The diagnosis of hernia in the groin and incompetence of the pouch of Douglas and pelvic floor". Acta Radiologica. Supplementum. 361: 1–76. PMID 6297246.
- Anaf V, Simon P, El Nakadi I, Simonart T, Noel J, Buxant F (February 2001). "Impact of surgical resection of rectovaginal pouch of douglas endometriotic nodules on pelvic pain and some elements of patients' sex life". The Journal of the American Association of Gynecologic Laparoscopists. 8 (1): 55–60. doi:10.1016/s1074-3804(05)60549-x. PMID 11172115.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Baessler K, Schuessler B (March 2000). "The depth of the pouch of Douglas in nulliparous and parous women without genital prolapse and in patients with genital prolapse". American Journal of Obstetrics and Gynecology. 182 (3): 540–4. doi:10.1067/mob.2000.104836. PMID 10739505.
- Ostör AG, Nirenberg A, Ashdown ML, Murphy DJ (June 1994). "Extragenital adenosarcoma arising in the pouch of Douglas". Gynecologic Oncology. 53 (3): 373–5. doi:10.1006/gyno.1994.1151. PMID 8206414.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
External links
- Anatomy photo:43:02-0300 at the SUNY Downstate Medical Center - "The Female Pelvis: Distribution of the Peritoneum in the Female Pelvis"
- Anatomy image:9610 at the SUNY Downstate Medical Center
- Anatomy image:9737 at the SUNY Downstate Medical Center
- Douglas'+Pouch at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- peritoneum at The Anatomy Lesson by Wesley Norman (Georgetown University)
- figures/chapter_35/35-8.HTM: Basic Human Anatomy at Dartmouth Medical School
- Template:RocheLexicon


