Fungal infection: Difference between revisions
common |
→Causes: COVID-19 and fungal infection |
||
| Line 119: | Line 119: | ||
Children whose [[immune systems]] are not functioning properly (such as children with cancer) are at risk of invasive fungal infections.<ref name=Blyth>{{Cite journal|last1=Blyth|first1=Christopher C|last2=Hale|first2=Katherine|last3=Palasanthiran|first3=Pamela|last4=O'Brien|first4=Tracey|last5=Bennett|first5=Michael H|date=2010-02-17|title=Antifungal therapy in infants and children with proven, probable or suspected invasive fungal infections|journal=Cochrane Database of Systematic Reviews|issue=2|pages=CD006343|doi=10.1002/14651858.cd006343.pub2|pmid=20166083|issn=1465-1858}}</ref> |
Children whose [[immune systems]] are not functioning properly (such as children with cancer) are at risk of invasive fungal infections.<ref name=Blyth>{{Cite journal|last1=Blyth|first1=Christopher C|last2=Hale|first2=Katherine|last3=Palasanthiran|first3=Pamela|last4=O'Brien|first4=Tracey|last5=Bennett|first5=Michael H|date=2010-02-17|title=Antifungal therapy in infants and children with proven, probable or suspected invasive fungal infections|journal=Cochrane Database of Systematic Reviews|issue=2|pages=CD006343|doi=10.1002/14651858.cd006343.pub2|pmid=20166083|issn=1465-1858}}</ref> |
||
===COVID-19=== |
|||
During the [[COVID-19 pandemic]] some fungal infections have been associated with [[COVID-19]].<ref name="CDCF">{{cite web |title=Fungal Diseases and COVID-19 {{!}} CDC |url=https://www.cdc.gov/fungal/covid-fungal.html |website=www.cdc.gov |access-date=7 August 2021 |language=en-us |date=7 June 2021}}</ref><ref name="Hoenigl">{{cite book |editor1-last=Hoenigl |editor1-first=Martin |editor2-last=Talento |editor2-first=Alida Fe |title=Fungal Infections Complicating COVID-19 |date=2021 |publisher=MDPI |isbn=978-3-0365-0554-1 |url=https://books.google.com/books?id=6rcsEAAAQBAJ |language=en}}</ref><ref name="Gangneux2020">{{cite journal |last1=Gangneux |first1=J.-P. |last2=Bougnoux |first2=M.-E. |last3=Dannaoui |first3=E. |last4=Cornet |first4=M. |last5=Zahar |first5=J.R. |title=Invasive fungal diseases during COVID-19: We should be prepared |journal=Journal De Mycologie Medicale |date=June 2020 |volume=30 |issue=2 |pages=100971 |doi=10.1016/j.mycmed.2020.100971 |pmid=32307254 |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7136887/ |issn=1156-5233}}</ref> Fungal infections can mimic COVID-19, occur at the same time as COVID-19 and more serious fungal infections can [[COVID-19#Prognosis|complicate]] COVID-19.<ref name="CDCF"/> A fungal infection may occur after [[antibiotics]] for a bacterial infection which has occurred following COVID-19.<ref name=Saxena>{{cite book |last1=Saxena |first1=Shailendra K. |title=Coronavirus Disease 2019 (COVID-19): Epidemiology, Pathogenesis, Diagnosis, and Therapeutics |date=2020 |publisher=Springer |location=Singapore |isbn=978-981-15-4813-0 |url=https://books.google.com/books?id=OWzqDwAAQBAJ&pg=PA73 |language=en|page=73}}</ref> The most common serious fungal infections in people with COVID-19 include [[aspergillosis]] and invasive [[candidiasis]].<ref name="CDC1">{{cite web |title=Fungal Diseases and COVID-19 |url=https://www.cdc.gov/fungal/covid-fungal.html |website=www.cdc.gov |access-date=7 August 2021 |language=en-us |date=7 June 2021}}</ref> COVID-19–associated [[mucormycosis]] is generally less common, but in 2021 was noted to be significantly more prevalent in India.<ref name="CDCF"/><ref name=Qu2021>{{cite book |last1=Qu |first1=Jie-Ming |last2=Cao |first2=Bin |last3=Chen |first3=Rong-Chang |title=COVID-19: The Essentials of Prevention and Treatment |date=2021 |publisher=Elsevier |location=Amsterdam, Netherlands |isbn=978-0-12-824003-8 |url=https://books.google.com/books?id=OWzqDwAAQBAJ |language=en}}</ref> |
|||
Some fungal infections such as [[coccidioidomycosis]], [[histoplasmosis]], and [[blastomycosis]] can present with [[fever]], [[cough]], and [[shortness of breath]], thereby resembling [[COVID-19]].<ref name="CDCF"/> |
|||
==Mechanism== |
==Mechanism== |
||
Revision as of 06:31, 7 August 2021
| Mycosis | |
|---|---|
| Other names | mycoses,[1] fungal disease,[2] fungal infection[3] ICD-10CM codes: Mycoses B35-B49 [4] |
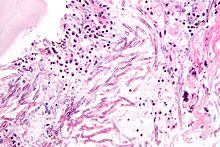 | |
| Micrograph showing a mycosis (aspergillosis). The Aspergillus (which is spaghetti-like) is seen in the center and surrounded by inflammatory cells and necrotic debris. H&E stain. | |
| Specialty | Infectious Diseases[5] |
| Types | Systemic, superficial, subcutaneous[3] |
| Causes | Pathogenic fungus: dermatophytes, yeasts, molds[6][7] |
| Risk factors | Immunodeficiency, cancer treatment, organ transplant,[6] Tuberculosis, COVID-19 |
| Diagnostic method | Based on symptoms, culture, microscopic examination[6] |
| Treatment | Antifungals[3] |
| Frequency | Common[8] |
| Deaths | 1.7 million (2020)[9] |
Mycoses, also known as fungal infections,[3] are infections caused by disease causing fungi, and are traditionally divided into superficial, subcutaneous, and systemic.[5][6] They include common tinea of the skin, yeast infections such as candidiasis and pityriasis versicolor, and several other opportunistic fungal infections such as systemic candidiasis, aspergillosis and mucormycosis, which are more severe.[1][7] Signs and symptoms range widely.[3] There is usually a rash in superficial infections.[2] Mycoses within the skin or under the skin may present with a lump and skin changes.[3] Pneumonia-like symptoms or meningitis may occur in deeper infections.[2]
Fungi that cause infections in people include yeasts, molds and fungi that are able to exist as both a mold and yeast.[3] Candida is the most common cause of fungal infection in people, particularly as oral thrush or vaginal yeast infection, often following taking antibiotics.[3] Mycoses occur after spores are either breathed in, come into contact with skin or enter the body through the skin such as via a cut, wound or injection.[3] Fungal infections are more likely in people with weak immune systems.[10] This includes people with illnesses such as HIV/AIDS, and people taking medicines such as steroids or cancer treatments.[10]
Diagnosis is generally based on signs and symptoms, microscopy, culture, sometimes requiring biopsy and aid from medical imaging.[6] Some superficial infections of the skin can appear similar to eczema and lichen planus.[7] Treatment is with antifungal medicines, usually in the form of a cream or by mouth or injection, depending on the specific infection and its extent.[11] Some require surgically cutting out infected tissue.[3]
Worldwide, fungal infections affect more than one billion people every year.[8] An estimated 1.7 million deaths from fungal disease were reported in 2020.[9] Several, including sporotrichosis, chromoblastomycosis and mycetoma are neglected.[12]
Classification
Mycoses are traditionally divided into superficial, subcutaneous, or systemic, where infection is deep, more widespread and involving internal body organs.[3][8] They can affect the nails, vagina, skin and mouth.[13] Some types such as blastomycosis, cryptococcus, coccidioidomycosis and histoplasmosis, affect people who live or visit certain parts of the world.[13] Others such as aspergillosis, pneumocystis pneumonia, candidiasis, mucormycosis and talaromycosis, tend to affect people who are unable to fight infection themselves.[13] Mycoses might not always conform strictly to the three divisions of superficial, subcutaneous and systemic.[3] Some superficial fungal infections can cause systemic infections in people who are immunocompromised.[3] Some subcutaneous fungal infections can invade into deeper structures, resulting in systemic disease.[3] Candida albicans can live in people without producing symptoms, and is able to cause both mild candidiasis in healthy people and severe invasive candidiasis in those who cannot fight infection themselves.[3][7]
ICD-11 codes
- 1F20 Aspergillosis
- 1F21 Basidiobolomycosis
- 1F22 Blastomycosis
- 1F23 Candidosis
- 1F24 Chromoblastomycosis
- 1F25 Coccidioidomycosis
- 1F26 Conidiobolomycosis
- 1F27 Cryptococcosis
- 1F28 Dermatophytosis
- 1F29 Eumycetoma
- 1F2A Histoplasmosis
- 1F2B Lobomycosis
- 1F2C Mucormycosis
- 1F2D Non-dermatophyte superficial dermatomycoses
- 1F2F Phaeohyphomycosis
- 1F2G Pneumocystosis
- 1F2H Scedosporiosis
- 1F2J Sporotrichosis
- 1F2K Talaromycosis
- 1F2L Emmonsiosis
Superficial mycoses
Superficial mycoses include candidiasis in healthy people, common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and malassezia infections such as pityriasis versicolor.[3][7]
-
Oral candidiasis
-
Tinea corporis
-
Pityriasis versicolor
-
Onychomycosis
Subcutaneous

Subcutaneous fungal infections include sporotrichosis, chromoblastomycosis, and eumycetoma.[3]
Systemic
Systemic fungal infections include histoplasmosis, cryptococcosis, coccidioidomycosis, blastomycosis, mucormycosis, aspergillosis, pneumocystis pneumonia and systemic candidiasis.[3]
Systemic mycoses due to primary pathogens originate normally in the lungs and may spread to other organ systems. Organisms that cause systemic mycoses are inherently virulent.[further explanation needed].[citation needed] Systemic mycoses due to opportunistic pathogens are infections of people with immune deficiencies who would otherwise not be infected. Examples of immunocompromised conditions include AIDS, alteration of normal flora by antibiotics, immunosuppressive therapy, and metastatic cancer. Examples of opportunistic mycoses include Candidiasis, Cryptococcosis and Aspergillosis.[citation needed]
Other
Fungal infections might not always conform strictly to the three divisions of superficial, subcutaneous and systemic.[3] Some superficial fungal infections can cause systemic infections in people who are immunocompromised.[3] Some subcutaneous fungal infections can invade into deeper structures, resulting in systemic disease.[3] Candida albicans can live in people without producing symptoms, and is able to cause both mild candidiasis in healthy people and severe invasive candidiasis in those who cannot fight infection themselves.[3][7]
Signs and symptoms
Most common mild mycoses often present with a rash.[2] Infections within the skin or under the skin may present with a lump and skin changes.[3] Less common deeper fungal infections may present with pneumonia like symptoms or meningitis.[2]
Causes
Mycoses are caused by certain fungi; yeasts, molds and some fungi that can exist as both a mold and yeast.[3][6] They are everywhere and infection occurs after spores are either breathed in, come into contact with skin or enter the body through the skin such as via a cut, wound or injection.[3] Candida albicans is the most common cause of fungal infection in people, particularly as oral or vaginal thrush, often following taking antibiotics.[3]
Risk factors
Fungal infections are more likely in people with weak immune systems.[10] This includes people with illnesses such as HIV/AIDS, and people taking medicines such as steroids or cancer treatments.[10] People with diabetes also tend to develop fungal infections.[14] Very young and very old people, also, are groups at risk.[15][dead link]
Individuals being treated with antibiotics are at higher risk of fungal infections.[16]
Children whose immune systems are not functioning properly (such as children with cancer) are at risk of invasive fungal infections.[17]
COVID-19
During the COVID-19 pandemic some fungal infections have been associated with COVID-19.[18][19][20] Fungal infections can mimic COVID-19, occur at the same time as COVID-19 and more serious fungal infections can complicate COVID-19.[18] A fungal infection may occur after antibiotics for a bacterial infection which has occurred following COVID-19.[21] The most common serious fungal infections in people with COVID-19 include aspergillosis and invasive candidiasis.[22] COVID-19–associated mucormycosis is generally less common, but in 2021 was noted to be significantly more prevalent in India.[18][23]
Some fungal infections such as coccidioidomycosis, histoplasmosis, and blastomycosis can present with fever, cough, and shortness of breath, thereby resembling COVID-19.[18]
Mechanism
Mycoses occur after spores are either breathed in, come into contact with skin or enter the body through a wound.[3]
Diagnosis
Diagnosis is generally by signs and symptoms, microscopy, biopsy, culture and sometimes with the aid of medical imaging.[6]
Differential diagnosis
Some tinea and candidiasis infections of the skin can appear similar to eczema and lichen planus.[7] Pityriasis versicolor can look like seborrheic dermatitis, pityriasis rosea, pityriasis alba and vitiligo.[7]
Some fungal infections such as coccidioidomycosis, histoplasmosis, and blastomycosis can present with fever, cough, and shortness of breath, thereby resembling COVID-19.[24]
Prevention
Keeping the skin clean and dry, as well as maintaining good hygiene, will help larger topical mycoses. Because some fungal infections are contagious, it is important to wash after touching other people or animals. Sports clothing should also be washed after use.[clarification needed][citation needed]
Treatment
Treatment usually requires topical or systemic antifungal medicines.[11] Sometimes, infected tissue needs to be surgically cut away.[3]
Epidemiology
Worldwide, every year fungal infections affect more than one billion people.[8] An estimated 1.6 million deaths from fungal disease were reported in 2017.[25] The figure has been rising, with an estimated 1.7 million deaths from fungal disease reported in 2020.[9]
Fungal infection also constitute a significant cause of morbidity and mortality in pediatric population.[26]
See also
References
- ^ a b Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. pp. 438–465. ISBN 978-0-7020-6830-0.
- ^ a b c d e "Fungal Diseases Homepage | CDC". www.cdc.gov. 29 March 2021. Retrieved 17 June 2021.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab Barlow, Gavin; Irving, Irving; moss, Peter J. (2020). "20. Infectious diseases". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. pp. 559–563. ISBN 978-0-7020-7870-5.
- ^ ICD-10CM. mycoses B35-B49.
{{cite book}}: CS1 maint: numeric names: authors list (link) - ^ a b c "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 25 May 2021.
- ^ a b c d e f g Willinger, Birgit (2019). "1. What is the target? Clinical mycology and diagnostics". In Elisabeth Presterl (ed.). Clinically Relevant Mycoses: A Practical Approach. Springer. pp. 3–19. ISBN 978-3-319-92299-7.
- ^ a b c d e f g h Kutzner, Heinz; Kempf, Werner; Feit, Josef; Sangueza, Omar (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. p. 77-108. ISBN 978-1-119-64706-5.
- ^ a b c d Nakazato, Gerson; Alesandra, Audrey; Lonni, Stringhen Garcia; Panagio, Luciano Aparecido; de Camargo, Larissa Ciappina; Goncalves, Marcelly Chue; Reis, Guilherne Fonseca; Miranda-Sapla, Milena Menegazzo; Tomiotto-Pellissier, Fernanda; Kobayashi, Renata Katsuko Takayama (2020). "4. Applications of nanometals in cutaneous infections". In Rai, Mahendra (ed.). Nanotechnology in Skin, Soft Tissue, and Bone Infections. Switzerland: Springer. ISBN 978-3-030-35146-5.
- ^ a b c Kainz, Katharina; Bauer, Maria A.; Madeo, Frank; Carmona-Gutierrez, Didac (2020). "Fungal infections in humans: the silent crisis". Microbial Cell. 7 (6): 143–145. doi:10.15698/mic2020.06.718. ISSN 2311-2638. PMC 7278517. PMID 32548176.
- ^ a b c d "Fungal Infections | Fungal | CDC". www.cdc.gov. 29 January 2019. Retrieved 16 June 2021.
- ^ a b Graininger, Wolfgang; Diab-Elschahawi, Magda; Presterl, Elisabeth (2019). "3. Antifungal agents". In Elisabeth Presterl (ed.). Clinically Relevant Mycoses: A Practical Approach. Springer. pp. 31–44. ISBN 978-3-319-92299-7.
- ^ Queiroz-Telles, Flavio; Fahal, Ahmed Hassan; Falci, Diego R.; Caceres, Diego H.; Chiller, Tom; Pasqualotto, Alessandro C. (1 November 2017). "Neglected endemic mycoses". The Lancet Infectious Diseases. 17 (11): e367–e377. doi:10.1016/S1473-3099(17)30306-7. ISSN 1473-3099. PMID 28774696.
- ^ a b c "Types of Fungal Diseases | Fungal Diseases | CDC". www.cdc.gov. 27 June 2019. Retrieved 12 June 2021.
- ^ "Thrush in Men". NHS. Retrieved 2013-07-13.
- ^ "Fungal infections: Introduction". Retrieved May 26, 2010.
- ^ Britt, L. D.; Peitzman, Andrew; Barie, Phillip; Jurkovich, Gregory (2012). Acute Care Surgery. p. 186. ISBN 9781451153934.
- ^ Blyth, Christopher C; Hale, Katherine; Palasanthiran, Pamela; O'Brien, Tracey; Bennett, Michael H (2010-02-17). "Antifungal therapy in infants and children with proven, probable or suspected invasive fungal infections". Cochrane Database of Systematic Reviews (2): CD006343. doi:10.1002/14651858.cd006343.pub2. ISSN 1465-1858. PMID 20166083.
- ^ a b c d "Fungal Diseases and COVID-19 | CDC". www.cdc.gov. 7 June 2021. Retrieved 7 August 2021.
- ^ Hoenigl, Martin; Talento, Alida Fe, eds. (2021). Fungal Infections Complicating COVID-19. MDPI. ISBN 978-3-0365-0554-1.
- ^ Gangneux, J.-P.; Bougnoux, M.-E.; Dannaoui, E.; Cornet, M.; Zahar, J.R. (June 2020). "Invasive fungal diseases during COVID-19: We should be prepared". Journal De Mycologie Medicale. 30 (2): 100971. doi:10.1016/j.mycmed.2020.100971. ISSN 1156-5233. PMID 32307254.
- ^ Saxena, Shailendra K. (2020). Coronavirus Disease 2019 (COVID-19): Epidemiology, Pathogenesis, Diagnosis, and Therapeutics. Singapore: Springer. p. 73. ISBN 978-981-15-4813-0.
- ^ "Fungal Diseases and COVID-19". www.cdc.gov. 7 June 2021. Retrieved 7 August 2021.
- ^ Qu, Jie-Ming; Cao, Bin; Chen, Rong-Chang (2021). COVID-19: The Essentials of Prevention and Treatment. Amsterdam, Netherlands: Elsevier. ISBN 978-0-12-824003-8.
- ^ "Fungal Diseases and COVID-19". www.cdc.gov. 7 June 2021. Retrieved 19 June 2021.
- ^ "Stop neglecting fungi". Nature Microbiology. 2 (8): 17120. 25 July 2017. doi:10.1038/nmicrobiol.2017.120. ISSN 2058-5276. PMID 28741610.
- ^ Sehgal, Mukul; Ladd, Hugh J.; Totapally, Balagangadhar (2020-12-01). "Trends in Epidemiology and Microbiology of Severe Sepsis and Septic Shock in Children". Hospital Pediatrics. 10 (12): 1021–1030. doi:10.1542/hpeds.2020-0174. ISSN 2154-1663. PMID 33208389.




