TREM2: Difference between revisions
Citation bot (talk | contribs) Alter: pages. Add: pmc, s2cid, doi-access. Formatted dashes. | Use this bot. Report bugs. | Suggested by Headbomb | Linked from Wikipedia:WikiProject_Academic_Journals/Journals_cited_by_Wikipedia/Sandbox | #UCB_webform_linked 25/414 |
Added more information based on more recent publications |
||
| Line 1: | Line 1: | ||
{{Infobox_gene}} |
{{Infobox_gene}} |
||
'''Triggering receptor expressed on myeloid cells 2''' |
'''Triggering receptor expressed on myeloid cells 2''' '''(TREM2)''' is a [[protein]] that in humans is encoded by the ''TREM2'' [[gene]].<ref name="pmid10799849">{{cite journal | vauthors = Bouchon A, Dietrich J, Colonna M | title = Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes | journal = Journal of Immunology | volume = 164 | issue = 10 | pages = 4991–4995 | date = May 2000 | pmid = 10799849 | doi = 10.4049/jimmunol.164.10.4991 | doi-access = free }}</ref><ref name="pmid12080485">{{cite journal | vauthors = Paloneva J, Manninen T, Christman G, Hovanes K, Mandelin J, Adolfsson R, Bianchin M, Bird T, Miranda R, Salmaggi A, Tranebjaerg L, Konttinen Y, Peltonen L | display-authors = 6 | title = Mutations in two genes encoding different subunits of a receptor signaling complex result in an identical disease phenotype | journal = American Journal of Human Genetics | volume = 71 | issue = 3 | pages = 656–662 | date = September 2002 | pmid = 12080485 | pmc = 379202 | doi = 10.1086/342259 }}</ref><ref name="entrez">{{cite web | title = Entrez Gene: TREM2 triggering receptor expressed on myeloid cells 2| url = https://www.ncbi.nlm.nih.gov/sites/entrez?Db=gene&Cmd=ShowDetailView&TermToSearch=54209}}</ref> The TREM2 protein is expressed primarily in immune cells in different tissues. In the [[brain]], TREM2 is expressed by [[microglia]],<ref>{{cite journal | vauthors = Rodríguez-Gómez JA, Kavanagh E, Engskog-Vlachos P, Engskog MK, Herrera AJ, Espinosa-Oliva AM, Joseph B, Hajji N, Venero JL, Burguillos MA | display-authors = 6 | title = Microglia: Agents of the CNS Pro-Inflammatory Response | journal = Cells | volume = 9 | issue = 7 | pages = E1717 | date = July 2020 | pmid = 32709045 | pmc = 7407646 | doi = 10.3390/cells9071717 | doi-access = free }}</ref> which are the [[Central nervous system|central nervous system's]] immune response system.<ref>{{cite journal | vauthors = Masuda T, Sankowski R, Staszewski O, Prinz M | title = Microglia Heterogeneity in the Single-Cell Era | journal = Cell Reports | volume = 30 | issue = 5 | pages = 1271–1281 | date = February 2020 | pmid = 32023447 | doi = 10.1016/j.celrep.2020.01.010 | s2cid = 211047418 }}</ref> In the [[liver]], TREM2 is expressed by several cell types, including macrophages that respond to insults to the tissue.<ref name=":42">{{cite journal | vauthors = Sun H, Feng J, Tang L | title = Function of TREM1 and TREM2 in Liver-Related Diseases | journal = Cells | volume = 9 | issue = 12 | pages = 2626 | date = December 2020 | pmid = 33297569 | pmc = 7762355 | doi = 10.3390/cells9122626 | doi-access = free }}</ref> In the [[bowel]] and [[intestine]], TREM2 is found on [[dendritic cell]]s.<ref name=":03">{{cite journal | vauthors = Genua M, Rutella S, Correale C, Danese S | title = The triggering receptor expressed on myeloid cells (TREM) in inflammatory bowel disease pathogenesis | journal = Journal of Translational Medicine | volume = 12 | pages = 293 | date = October 2014 | pmid = 25347935 | pmc = 4231187 | doi = 10.1186/s12967-014-0293-z }}</ref> TREM2 is overexpressed in many tumor types and is increasingly recognized as an important factor in development of inflammatory diseases and cancer. It therefore appears to be a good therapeutic target. |
||
== Gene == |
== Gene == |
||
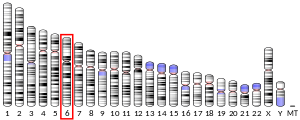
The TREM2 gene lies on the [[Chromosome 6|sixth chromosome]] in humans, specifically in location 6p21.1. The gene has 5 coding [[exon]] regions.<ref name=":1">{{Cite web|title=TREM2 triggering receptor expressed on myeloid cells 2 [Homo sapiens (human)] - Gene - NCBI|url=https://www.ncbi.nlm.nih.gov/gene/54209|access-date=2021-11-02|website=www.ncbi.nlm.nih.gov}}</ref><ref name=":132">{{cite journal | vauthors = Natale G, Biagioni F, Busceti CL, Gambardella S, Limanaqi F, Fornai F | title = TREM Receptors Connecting Bowel Inflammation to Neurodegenerative Disorders | journal = Cells | volume = 8 | issue = 10 | pages = E1124 | date = September 2019 | pmid = 31546668 | pmc = 6829526 | doi = 10.3390/cells8101124 | doi-access = free }}</ref> [[Alternative splicing]] of the TREM2 [[Messenger RNA|mRNA]] transcript leads to different [[Protein isoform|isoforms]] of the protein being produced upon translation.<ref name=":1" /> Specifically, TREM2 mRNA has 3 different isoforms containing three consistent exons, and two that vary between the isoforms.<ref name=":84">{{cite journal | vauthors = Yang J, Fu Z, Zhang X, Xiong M, Meng L, Zhang Z | title = TREM2 ectodomain and its soluble form in Alzheimer's disease | journal = Journal of Neuroinflammation | volume = 17 | issue = 1 | pages = 204 | date = July 2020 | pmid = 32635934 | pmc = 7341574 | doi = 10.1186/s12974-020-01878-2 }}</ref> Encoding for receptors in many different cell types, TREM2 mRNA is found in different organs across the body, but is most expressed in the brain, lungs, [[adrenal gland]]s, [[placenta]], [[Gallbladder|gall bladder]], and colon.<ref name=":1" /> The TREM2 gene is present not only in humans, but in mice as well, which has allowed researchers to create a plethora of genetic models containing different mutations of the TREM2 gene to study the effects of these mutations in disease states.<ref>{{Cite web|title=Jackson Laboratory Search- TREM2|url=https://www.jax.org/search?q=trem2&filter=Url%3A(%22%2Fjax-mice-and-services%22%20OR%20%22https%3A%2F%2Fresources.jax.org%22)%20OR%20Author%3A%22JMCRS%22 |website=Jackson Laboratory}}</ref> In addition to the mouse, the TREM2 gene can be found in many animals along the evolutionary tree, including rats, dogs, monkeys and more.<ref>{{cite journal | vauthors = Smith JR, Hayman GT, Wang SJ, Laulederkind SJ, Hoffman MJ, Kaldunski ML, Tutaj M, Thota J, Nalabolu HS, Ellanki SL, Tutaj MA, De Pons JL, Kwitek AE, Dwinell MR, Shimoyama ME | display-authors = 6 | title = The Year of the Rat: The Rat Genome Database at 20: a multi-species knowledgebase and analysis platform | journal = Nucleic Acids Research | volume = 48 | issue = D1 | pages = D731–D742 | date = January 2020 | pmid = 31713623 | pmc = 7145519 | doi = 10.1093/nar/gkz1041 }}</ref> |
The ''TREM2'' gene lies on the [[Chromosome 6|sixth chromosome]] in humans, specifically in location 6p21.1. The gene has 5 coding [[exon]] regions.<ref name=":1">{{Cite web|title=TREM2 triggering receptor expressed on myeloid cells 2 [Homo sapiens (human)] - Gene - NCBI|url=https://www.ncbi.nlm.nih.gov/gene/54209|access-date=2021-11-02|website=www.ncbi.nlm.nih.gov}}</ref><ref name=":132">{{cite journal | vauthors = Natale G, Biagioni F, Busceti CL, Gambardella S, Limanaqi F, Fornai F | title = TREM Receptors Connecting Bowel Inflammation to Neurodegenerative Disorders | journal = Cells | volume = 8 | issue = 10 | pages = E1124 | date = September 2019 | pmid = 31546668 | pmc = 6829526 | doi = 10.3390/cells8101124 | doi-access = free }}</ref> [[Alternative splicing]] of the ''TREM2'' [[Messenger RNA|mRNA]] transcript leads to different [[Protein isoform|isoforms]] of the protein being produced upon translation.<ref name=":1" /> Specifically, ''TREM2'' mRNA has 3 different isoforms containing three consistent exons, and two that vary between the isoforms.<ref name=":84">{{cite journal | vauthors = Yang J, Fu Z, Zhang X, Xiong M, Meng L, Zhang Z | title = TREM2 ectodomain and its soluble form in Alzheimer's disease | journal = Journal of Neuroinflammation | volume = 17 | issue = 1 | pages = 204 | date = July 2020 | pmid = 32635934 | pmc = 7341574 | doi = 10.1186/s12974-020-01878-2 }}</ref> Encoding for receptors in many different cell types, ''TREM2'' mRNA is found in different organs across the body, but is most expressed in the brain, lungs, [[adrenal gland]]s, [[placenta]], [[Gallbladder|gall bladder]], and colon.<ref name=":1" /> The ''TREM2'' gene is present not only in humans, but in mice as well, which has allowed researchers to create a plethora of genetic models containing different mutations of the ''TREM2'' gene to study the effects of these mutations in disease states.<ref>{{Cite web|title=Jackson Laboratory Search- TREM2|url=https://www.jax.org/search?q=trem2&filter=Url%3A(%22%2Fjax-mice-and-services%22%20OR%20%22https%3A%2F%2Fresources.jax.org%22)%20OR%20Author%3A%22JMCRS%22 |website=Jackson Laboratory}}</ref> In addition to the mouse, the ''TREM2'' gene can be found in many animals along the evolutionary tree, including rats, dogs, monkeys and more.<ref>{{cite journal | vauthors = Smith JR, Hayman GT, Wang SJ, Laulederkind SJ, Hoffman MJ, Kaldunski ML, Tutaj M, Thota J, Nalabolu HS, Ellanki SL, Tutaj MA, De Pons JL, Kwitek AE, Dwinell MR, Shimoyama ME | display-authors = 6 | title = The Year of the Rat: The Rat Genome Database at 20: a multi-species knowledgebase and analysis platform | journal = Nucleic Acids Research | volume = 48 | issue = D1 | pages = D731–D742 | date = January 2020 | pmid = 31713623 | pmc = 7145519 | doi = 10.1093/nar/gkz1041 }}</ref> |
||
In the brain, TREM2 is expressed differentially between brain regions, with the highest levels of this protein being found in the [[hippocampus]], the [[white matter]], and the [[spinal cord]]. In humans and mice, the levels of TREM2 increase with age.<ref name=":172">{{cite journal | vauthors = Gratuze M, Leyns CE, Holtzman DM | title = New insights into the role of TREM2 in Alzheimer's disease | journal = Molecular Neurodegeneration | volume = 13 | issue = 1 | pages = 66 | date = December 2018 | pmid = 30572908 | pmc = 6302500 | doi = 10.1186/s13024-018-0298-9 }}</ref> |
In the brain, TREM2 is expressed differentially between brain regions, with the highest levels of this protein being found in the [[hippocampus]], the [[white matter]], and the [[spinal cord]]. In humans and mice, the levels of TREM2 increase with age.<ref name=":172">{{cite journal | vauthors = Gratuze M, Leyns CE, Holtzman DM | title = New insights into the role of TREM2 in Alzheimer's disease | journal = Molecular Neurodegeneration | volume = 13 | issue = 1 | pages = 66 | date = December 2018 | pmid = 30572908 | pmc = 6302500 | doi = 10.1186/s13024-018-0298-9 }}</ref> |
||
| Line 9: | Line 9: | ||
== Protein == |
== Protein == |
||
[[File:STREM2-2.jpg|thumb|The TREM2 receptor with the ADAM10 and ADAM17 enzymes that create the soluble TREM2 fragment. Created with BioRender.com ]] |
[[File:STREM2-2.jpg|thumb|The TREM2 receptor with the ADAM10 and ADAM17 enzymes that create the soluble TREM2 fragment. Created with BioRender.com ]] |
||
The TREM2 receptor is a [[transmembrane protein]] that is made up of an extracellular region (also referred to as the ectodomain), the membrane traversing segment, and an intracellular component.<ref name=":73">{{cite journal | vauthors = Kulkarni B, Kumar D, Cruz-Martins N, Sellamuthu S | title = Role of TREM2 in Alzheimer's Disease: A Long Road Ahead | journal = Molecular Neurobiology | volume = 58 | issue = 10 | pages = 5239–5252 | date = October 2021 | pmid = 34275100 | doi = 10.1007/s12035-021-02477-9 | s2cid = 236090999 }}</ref> The extracellular component of TREM2 can bind different anionic ligands, specifically [[glycoprotein]]s and lipids.<ref name=":92">{{cite journal | vauthors = Hamerman JA, Pottle J, Ni M, He Y, Zhang ZY, Buckner JH | title = Negative regulation of TLR signaling in myeloid cells--implications for autoimmune diseases | journal = Immunological Reviews | volume = 269 | issue = 1 | pages = 212–227 | date = January 2016 | pmid = 26683155 | pmc = 4703580 | doi = 10.1111/imr.12381 }}</ref><ref name=":34">{{cite journal | vauthors = Deczkowska A, Weiner A, Amit I | title = The Physiology, Pathology, and Potential Therapeutic Applications of the TREM2 Signaling Pathway | journal = Cell | volume = 181 | issue = 6 | pages = 1207–1217 | date = June 2020 | pmid = 32531244 | doi = 10.1016/j.cell.2020.05.003 | s2cid = 219572314 }}</ref> This ectodomain component includes an [[Ig-like V-type domain]] where ligands bind the receptor.<ref name=":102">{{cite journal | vauthors = Dardiotis E, Siokas V, Pantazi E, Dardioti M, Rikos D, Xiromerisiou G, Markou A, Papadimitriou D, Speletas M, Hadjigeorgiou GM | display-authors = 6 | title = A novel mutation in TREM2 gene causing Nasu-Hakola disease and review of the literature | journal = Neurobiology of Aging | volume = 53 | pages = 194.e13–194.e22 | date = May 2017 | pmid = 28214109 | doi = 10.1016/j.neurobiolaging.2017.01.015 | s2cid = 22618858 }}</ref> The TREM2 ectodomain is modified after the translation of the protein, which changes its affinity for |
The TREM2 receptor is a [[transmembrane protein]] that is made up of an extracellular region (also referred to as the ectodomain), the membrane traversing segment, and an intracellular component.<ref name=":73">{{cite journal | vauthors = Kulkarni B, Kumar D, Cruz-Martins N, Sellamuthu S | title = Role of TREM2 in Alzheimer's Disease: A Long Road Ahead | journal = Molecular Neurobiology | volume = 58 | issue = 10 | pages = 5239–5252 | date = October 2021 | pmid = 34275100 | doi = 10.1007/s12035-021-02477-9 | s2cid = 236090999 }}</ref> The extracellular component of TREM2 can bind different anionic ligands, specifically [[glycoprotein]]s and lipids.<ref name=":92">{{cite journal | vauthors = Hamerman JA, Pottle J, Ni M, He Y, Zhang ZY, Buckner JH | title = Negative regulation of TLR signaling in myeloid cells--implications for autoimmune diseases | journal = Immunological Reviews | volume = 269 | issue = 1 | pages = 212–227 | date = January 2016 | pmid = 26683155 | pmc = 4703580 | doi = 10.1111/imr.12381 }}</ref><ref name=":34">{{cite journal | vauthors = Deczkowska A, Weiner A, Amit I | title = The Physiology, Pathology, and Potential Therapeutic Applications of the TREM2 Signaling Pathway | journal = Cell | volume = 181 | issue = 6 | pages = 1207–1217 | date = June 2020 | pmid = 32531244 | doi = 10.1016/j.cell.2020.05.003 | s2cid = 219572314 }}</ref> This ectodomain component includes an [[Ig-like V-type domain]] where ligands bind the receptor.<ref name=":102">{{cite journal | vauthors = Dardiotis E, Siokas V, Pantazi E, Dardioti M, Rikos D, Xiromerisiou G, Markou A, Papadimitriou D, Speletas M, Hadjigeorgiou GM | display-authors = 6 | title = A novel mutation in TREM2 gene causing Nasu-Hakola disease and review of the literature | journal = Neurobiology of Aging | volume = 53 | pages = 194.e13–194.e22 | date = May 2017 | pmid = 28214109 | doi = 10.1016/j.neurobiolaging.2017.01.015 | s2cid = 22618858 }}</ref> The TREM2 ectodomain is modified after the translation of the protein, which changes its affinity for different ligands.<ref name=":84"/> The intracellular component of TREM2 does not have any signaling ability on its own; rather, it signals via the DNAX activator proteins 10 and 12 ([[DAP10]] and [[DAP12]]). A single TREM2 molecule can interact with DAP10 and DAP12 at the same time.<ref name=":34"/> |
||
Part of the ectodomain of TREM2 can be processed by enzymes a disintegrin and metalloprotease 10 and 17 ([[ADAM10]], [[ADAM17]]) and released as a soluble version |
Part of the ectodomain of TREM2 can be processed by enzymes a disintegrin and metalloprotease 10 and 17 ([[ADAM10]], [[ADAM17]]) and released as a soluble version, called soluble TREM2 ('''sTREM2''').<ref name=":84"/> This protein fragment is released into the sera and cerebral spinal fluid ([[Cerebrospinal fluid|CSF)]], and might serve as a biomarker for neurodegenerative and other disorders, but further studies are needed.<ref name=":84"/> |
||
== Function == |
== Function == |
||
[[File:5eli_assembly-1.jpg|thumb|TREM2 structure as identified with [[X-ray crystallography]]. Image available through RCSB PDB.<ref>{{cite journal | vauthors = Kober DL, Alexander-Brett JM, Karch CM, Cruchaga C, Colonna M, Holtzman MJ, Brett TJ | title = Neurodegenerative disease mutations in TREM2 reveal a functional surface and distinct loss-of-function mechanisms | journal = eLife | volume = 5 | pages = e20391 | date = December 2016 | pmid = 27995897 | pmc = 5173322 | doi = 10.7554/eLife.20391 }}</ref>]] |
[[File:5eli_assembly-1.jpg|thumb|TREM2 structure as identified with [[X-ray crystallography]]. Image available through RCSB PDB.<ref>{{cite journal | vauthors = Kober DL, Alexander-Brett JM, Karch CM, Cruchaga C, Colonna M, Holtzman MJ, Brett TJ | title = Neurodegenerative disease mutations in TREM2 reveal a functional surface and distinct loss-of-function mechanisms | journal = eLife | volume = 5 | pages = e20391 | date = December 2016 | pmid = 27995897 | pmc = 5173322 | doi = 10.7554/eLife.20391 }}</ref>]] |
||
The TREM2 protein is found in immune cells termed [[Myelocyte|myeloid cells]], a category which include cells such as [[macrophages]], [[granulocyte]]s, monocytes, and dendritic cells.<ref>{{cite journal | vauthors = De Kleer I, Willems F, Lambrecht B, Goriely S | title = Ontogeny of myeloid cells | journal = Frontiers in Immunology | volume = 5 | pages = 423 | date = 2014 | pmid = 25232355 | pmc = 4153297 | doi = 10.3389/fimmu.2014.00423 | doi-access = free }}</ref> In the brain, |
The TREM2 protein is found in immune cells termed [[Myelocyte|myeloid cells]], a category which include cells such as [[macrophages]], [[granulocyte]]s, monocytes, and dendritic cells.<ref>{{cite journal | vauthors = De Kleer I, Willems F, Lambrecht B, Goriely S | title = Ontogeny of myeloid cells | journal = Frontiers in Immunology | volume = 5 | pages = 423 | date = 2014 | pmid = 25232355 | pmc = 4153297 | doi = 10.3389/fimmu.2014.00423 | doi-access = free }}</ref> In the brain, TREM2 is expressed on microglial cells,<ref name=":172"/> which are analogous to the immune cells in other tissues and blood. Monocyte-, macrophage-, and neutrophil-mediated inflammatory responses can be stimulated through [[G protein]]-linked 7-transmembrane receptors (e.g., [[FPR1]]), [[Fc receptor]]s, [[CD14]] and [[Toll-like receptor]]s (e.g., [[TLR4]]), and cytokine receptors (e.g., [[IFNGR1]]).<ref name=":18">{{cite journal | vauthors = Futosi K, Fodor S, Mócsai A | title = Neutrophil cell surface receptors and their intracellular signal transduction pathways | journal = International Immunopharmacology | volume = 17 | issue = 3 | pages = 638–650 | date = November 2013 | pmid = 23994464 | pmc = 3827506 | doi = 10.1016/j.intimp.2013.06.034 }}</ref><ref>{{cite journal | vauthors = Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L | display-authors = 6 | title = Inflammatory responses and inflammation-associated diseases in organs | journal = Oncotarget | volume = 9 | issue = 6 | pages = 7204–7218 | date = January 2018 | pmid = 29467962 | pmc = 5805548 | doi = 10.18632/oncotarget.23208 }}</ref> Engagement of these receptors can also prime myeloid cells to respond to other stimuli. Myeloid cells express receptors belonging to the [[Immunoglobulin superfamily|immunoglobulin (Ig) superfamily]], such as TREM2, or to the [[C-type lectin]] superfamily.<ref name=":18" /><ref>{{cite journal | vauthors = Sancho D, Reis e Sousa C | title = Sensing of cell death by myeloid C-type lectin receptors | journal = Current Opinion in Immunology | volume = 25 | issue = 1 | pages = 46–52 | date = February 2013 | pmid = 23332826 | pmc = 4480265 | doi = 10.1016/j.coi.2012.12.007 }}</ref> |
||
On myeloid cells, TREM2 binds anionic molecules, free and bound to plasma membrane, including bacterial products, DNA, lipoproteins, phospholipids, glycoproteins, DNA, and bacterial fragments,<ref name=":132"/><ref name=":92"/><ref name=":34"/><ref name=":142">{{cite journal | vauthors = Kober DL, Brett TJ | title = TREM2-Ligand Interactions in Health and Disease | journal = Journal of Molecular Biology | volume = 429 | issue = 11 | pages = 1607–1629 | date = June 2017 | pmid = 28432014 | pmc = 5485854 | doi = 10.1016/j.jmb.2017.04.004 }}</ref> <ref>{{Cite journal |last=Kober |first=Daniel L. |last2=Brett |first2=Tom J. |date=2017-06 |title=TREM2-Ligand Interactions in Health and Disease |url=https://linkinghub.elsevier.com/retrieve/pii/S0022283617301791 |journal=Journal of Molecular Biology |language=en |volume=429 |issue=11 |pages=1607–1629 |doi=10.1016/j.jmb.2017.04.004 |pmc=PMC5485854 |pmid=28432014}}</ref>. TREM2 binding of ligand results in phosphorylation at 2 tyrosines in the [[immunoreceptor tyrosine-based activation motif]] (ITAM) of DAP12 by SRC tyrosine kinases.<ref name=":34"/> Spleen tyrosine kinase ([[Syk]]) interacts with these phosphorylation sites and activates the [[phosphatidylinositol-3 kinase]] ([[PI3K]]) signaling pathway, as well as other signaling molecules such as [[mTOR]], [[Mitogen-activated protein kinase|MAPK]], and [[Extracellular signal-regulated kinases|ERK]].<ref name=":34"/><ref name=":152">{{cite journal | vauthors = Xing J, Titus AR, Humphrey MB | title = The TREM2-DAP12 signaling pathway in Nasu-Hakola disease: a molecular genetics perspective | journal = Research and Reports in Biochemistry | volume = 5 | pages = 89–100 | date = 2015 | pmid = 26478868 | pmc = 4605443 | doi = 10.2147/RRBC.S58057 }}</ref> Association of TREM2 with DAP10 also activates the PI3K signaling pathway<ref name=":162">{{cite journal | vauthors = Qiu H, Shao Z, Wen X, Jiang J, Ma Q, Wang Y, Huang L, Ding X, Zhang L | display-authors = 6 | title = TREM2: Keeping Pace With Immune Checkpoint Inhibitors in Cancer Immunotherapy | journal = Frontiers in Immunology | volume = 12 | pages = 716710 | date = 2021 | pmid = 34539652 | pmc = 8446424 | doi = 10.3389/fimmu.2021.716710 | doi-access = free }}</ref>, leading to expression of transcription factors that include [[AP-1 transcription factor|AP1]], [[NF-κB]], and [[NFAT]].<ref name=":152"/> The PI3K signaling pathway also increases intracellular calcium content, which activates calcium-dependent kinases.<ref name=":152"/><ref name=":162"/> TREM2 activation also affects expression of [[Galectin-1|GAL1]], [[Galectin-3|GAL3]], [[Interleukin 1 receptor antagonist|IL1RN]], and progranulin, which modulate the immune response.<ref name=":34"/> |
|||
TREM2 is expressed by microglia and osteoclasts, and is involved in development and/or maintenance of brain and bone.<ref name=":34"/> In mice, TREM2 is involved in synaptic pruning, a process of shaping neuronal circuitry by microglia- and astrocyte-mediated removal of excessive synapses via phagocytosis.<ref name=":84"/><ref>{{cite journal | vauthors = Hong S, Dissing-Olesen L, Stevens B | title = New insights on the role of microglia in synaptic pruning in health and disease | journal = Current Opinion in Neurobiology | volume = 36 | pages = 128–134 | date = February 2016 | pmid = 26745839 | pmc = 5479435 | doi = 10.1016/j.conb.2015.12.004 }}</ref><ref>{{Cite journal |last=Filipello |first=Fabia |last2=Morini |first2=Raffaella |last3=Corradini |first3=Irene |last4=Zerbi |first4=Valerio |last5=Canzi |first5=Alice |last6=Michalski |first6=Bernadeta |last7=Erreni |first7=Marco |last8=Markicevic |first8=Marija |last9=Starvaggi-Cucuzza |first9=Chiara |last10=Otero |first10=Karel |last11=Piccio |first11=Laura |date=2018-05 |title=The Microglial Innate Immune Receptor TREM2 Is Required for Synapse Elimination and Normal Brain Connectivity |url=https://doi.org/10.1016/j.immuni.2018.04.016 |journal=Immunity |volume=48 |issue=5 |pages=979–991.e8 |doi=10.1016/j.immuni.2018.04.016 |issn=1074-7613}}</ref> TREM2 is also expressed by macrophages of adipose tissue, adrenal gland, and placenta<ref name=":34" />. |
|||
Immunosuppressive tumor-associated macrophages ([[Tumor-associated macrophage|TAMs]]) have been characterized by expression of TREM2 <ref>{{Cite journal |last=Molgora |first=Martina |last2=Colonna |first2=Marco |date=2021-06 |title=Turning enemies into allies—reprogramming tumor-associated macrophages for cancer therapy |url=https://linkinghub.elsevier.com/retrieve/pii/S2666634021001926 |journal=Med |language=en |volume=2 |issue=6 |pages=666–681 |doi=10.1016/j.medj.2021.05.001 |pmc=PMC8238417 |pmid=34189494}}</ref> TREM2 signaling leads to downregulated transcription of genes that promote inflammation (''Tnf, Il1b,'' and ''Nos2'') <ref>{{Cite journal |last=Takahashi |first=Kazuya |last2=Rochford |first2=Christian D.P. |last3=Neumann |first3=Harald |date=2005-02-21 |title=Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2 |url=https://rupress.org/jem/article/201/4/647/52887/Clearance-of-apoptotic-neurons-without |journal=Journal of Experimental Medicine |language=en |volume=201 |issue=4 |pages=647–657 |doi=10.1084/jem.20041611 |issn=1540-9538 |pmc=PMC2213053 |pmid=15728241}}</ref>, as well as release of cytokines that prevent activation of anti-tumor CD8+ T cells <ref>{{Cite journal |last=Molgora |first=Martina |last2=Esaulova |first2=Ekaterina |last3=Vermi |first3=William |last4=Hou |first4=Jinchao |last5=Chen |first5=Yun |last6=Luo |first6=Jingqin |last7=Brioschi |first7=Simone |last8=Bugatti |first8=Mattia |last9=Omodei |first9=Andrea Salvatore |last10=Ricci |first10=Biancamaria |last11=Fronick |first11=Catrina |date=2020-08 |title=TREM2 Modulation Remodels the Tumor Myeloid Landscape Enhancing Anti-PD-1 Immunotherapy |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867420308783 |journal=Cell |language=en |volume=182 |issue=4 |pages=886–900.e17 |doi=10.1016/j.cell.2020.07.013 |pmc=PMC7485282 |pmid=32783918}}</ref>. TREM2+ immunosuppressive TAMs correlate with the level of exhausted [[T cell|T cells]] in the human tumor microenvironment ([[Tumor microenvironment|TME]]) <ref>{{Cite journal |last=Binnewies |first=Mikhail |last2=Pollack |first2=Joshua L. |last3=Rudolph |first3=Joshua |last4=Dash |first4=Subhadra |last5=Abushawish |first5=Marwan |last6=Lee |first6=Tian |last7=Jahchan |first7=Nadine S. |last8=Canaday |first8=Pamela |last9=Lu |first9=Erick |last10=Norng |first10=Manith |last11=Mankikar |first11=Shilpa |date=2021-10 |title=Targeting TREM2 on tumor-associated macrophages enhances immunotherapy |url=https://linkinghub.elsevier.com/retrieve/pii/S2211124721013085 |journal=Cell Reports |language=en |volume=37 |issue=3 |pages=109844 |doi=10.1016/j.celrep.2021.109844}}</ref>. A TREM2+ TAM-rich TME therefore appears to be immunosuppressive and might promote resistance to cancer therapies, such as [[Checkpoint inhibitor|checkpoint inhibitors]]. |
|||
If TREM2 is cleaved and sTREM2 produced, the stereotypical TREM2 signaling cascade will not occur, even if the Ig like domain is bound by a ligand. sTREM2 is still found to have some functionality, and when an insult occurs, it may help myeloid cells avoid apoptosis. This truncated version of the receptor may also increase pro-inflammatory phenotypes.<ref name=":34"/> sTREM2 has been indicated in activating downstream pathways such as PI3K and ERK through an unidentified receptor.<ref>{{cite journal | vauthors = Konishi H, Kiyama H | title = Microglial TREM2/DAP12 Signaling: A Double-Edged Sword in Neural Diseases | journal = Frontiers in Cellular Neuroscience | volume = 12 | pages = 206 | date = 2018 | pmid = 30127720 | pmc = 6087757 | doi = 10.3389/fncel.2018.00206 | doi-access = free }}</ref> |
|||
TREM2 signaling can antagonize Toll-like receptor ([[Toll-like receptor|TLR]]) expression and signaling, resulting in reduced production of inflammatory cytokines by cultured mouse macrophages <ref name=":34" />. Conversely, TREM2 expression is reduced following inflammatory signaling induction by LPS (a TLR4 ligand) or interferon gamma (IFNγ) <ref>{{Cite journal |last=Gao |first=Xiaoling |last2=Dong |first2=Yanting |last3=Liu |first3=Zhuola |last4=Niu |first4=Bo |date=2013-03 |title=Silencing of triggering receptor expressed on myeloid cells-2 enhances the inflammatory responses of alveolar macrophages to lipopolysaccharide |url=https://www.spandidos-publications.com/10.3892/mmr.2013.1268 |journal=Molecular Medicine Reports |language=en |volume=7 |issue=3 |pages=921–926 |doi=10.3892/mmr.2013.1268 |issn=1791-2997}}</ref>. TREM2 exerts neuroprotective effects not only by producing anti-inflammatory cytokines, but also by promoting the clearance of abnormal proteins and phagocytosis of apoptotic neurons<ref name=":84" /><ref>{{Cite journal |last=Takahashi |first=Kazuya |last2=Rochford |first2=Christian D.P. |last3=Neumann |first3=Harald |date=2005-02-21 |title=Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2 |url=https://rupress.org/jem/article/201/4/647/52887/Clearance-of-apoptotic-neurons-without |journal=Journal of Experimental Medicine |language=en |volume=201 |issue=4 |pages=647–657 |doi=10.1084/jem.20041611 |issn=1540-9538 |pmc=PMC2213053 |pmid=15728241}}</ref>. |
|||
TREM2 signaling has been reported to have some proinflammatory effects, such as in [[Inflammatory bowel disease|inflammatory bowel diseases (IBD)]].<ref name=":03" /> sTREM2 is believed to negatively regulate TREM2 signaling by acting as decoy receptors <ref>{{Cite journal |last=Piccio |first=Laura |last2=Buonsanti |first2=Cecilia |last3=Cella |first3=Marina |last4=Tassi |first4=Ilaria |last5=Schmidt |first5=Robert E. |last6=Fenoglio |first6=Chiara |last7=Rinker |first7=John |last8=Naismith |first8=Robert T. |last9=Panina-Bordignon |first9=Paola |last10=Passini |first10=Nadia |last11=Galimberti |first11=Daniela |date=2008-11 |title=Identification of soluble TREM-2 in the cerebrospinal fluid and its association with multiple sclerosis and CNS inflammation |url=https://academic.oup.com/brain/article-lookup/doi/10.1093/brain/awn217 |journal=Brain |language=en |volume=131 |issue=11 |pages=3081–3091 |doi=10.1093/brain/awn217 |issn=1460-2156 |pmc=PMC2577803 |pmid=18790823}}</ref> sTREM might therefore have pro-inflammatory effects.<ref name=":34" /> sTREM2 has been indicated in activating signaling pathways such as PI3K and ERK through an unidentified receptor.<ref>{{cite journal | vauthors = Konishi H, Kiyama H | title = Microglial TREM2/DAP12 Signaling: A Double-Edged Sword in Neural Diseases | journal = Frontiers in Cellular Neuroscience | volume = 12 | pages = 206 | date = 2018 | pmid = 30127720 | pmc = 6087757 | doi = 10.3389/fncel.2018.00206 | doi-access = free }}</ref> Levels of sTREM2 are increased in cerebrospinal fluid (CSF) of patients with Alzheimer's disease (AD), and correlate with the CSF levels of AD biomarkers, namely t-tau and p-tau <ref>{{Cite journal |last=Yang |first=Jiaolong |last2=Fu |first2=Zhihui |last3=Zhang |first3=Xingyu |last4=Xiong |first4=Min |last5=Meng |first5=Lanxia |last6=Zhang |first6=Zhentao |date=2020-12 |title=TREM2 ectodomain and its soluble form in Alzheimer’s disease |url=https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-020-01878-2 |journal=Journal of Neuroinflammation |language=en |volume=17 |issue=1 |pages=204 |doi=10.1186/s12974-020-01878-2 |issn=1742-2094 |pmc=PMC7341574 |pmid=32635934}}</ref> |
|||
== Association with diseases == |
== Association with diseases == |
||
TREM2 signaling has been associated with pathogenesis of several diseases. Variants of in the ''DAP12 (TYROBP)'' or ''TREM2'' genes have been associated with [[polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy]] (PLOSL or Nasu–Hakola disease).<ref name=":112">{{cite journal | vauthors = Bianchin MM, Capella HM, Chaves DL, Steindel M, Grisard EC, Ganev GG, da Silva Júnior JP, Neto Evaldo S, Poffo MA, Walz R, Carlotti Júnior CG, Sakamoto AC | display-authors = 6 | title = Nasu-Hakola disease (polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy--PLOSL): a dementia associated with bone cystic lesions. From clinical to genetic and molecular aspects | journal = Cellular and Molecular Neurobiology | volume = 24 | issue = 1 | pages = 1–24 | date = February 2004 | pmid = 15049507 | doi = 10.1023/b:cemn.0000012721.08168.ee | s2cid = 7089775 }}</ref> |
|||
[[File:TREM2_Alzheimer's.jpg|thumb| |
[[File:TREM2_Alzheimer's.jpg|thumb|Mutations in ''TREM2'' associated with Alzheimer's disease lead to decreased binding affinity for ligands, resulting in reduced microglial responses to amyloid-beta plaques. Created with BioRender.com ]] |
||
=== Alzheimer's disease === |
=== Alzheimer's disease === |
||
Variants of ''TREM2'' have been associated with neurodegenerative disorders, including [[Alzheimer's disease]] (AD).<ref name=":5">{{cite journal | vauthors = Shi Y, Holtzman DM | title = Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight | journal = Nature Reviews. Immunology | volume = 18 | issue = 12 | pages = 759–772 | date = December 2018 | pmid = 30140051 | pmc = 6425488 | doi = 10.1038/s41577-018-0051-1 }}</ref> TREM2 is involved in the microglial response to the [[amyloid plaque]]s that are characteristic of AD. Loss of TREM2 function reduces the responses of microglia to plaques, which then appear to take on a more toxic state.<ref name=":5" /> Expression of TREM2 is closely tied to that of [[CD33]].<ref>{{cite journal | vauthors = Griciuc A, Patel S, Federico AN, Choi SH, Innes BJ, Oram MK, Cereghetti G, McGinty D, Anselmo A, Sadreyev RI, Hickman SE, El Khoury J, Colonna M, Tanzi RE | display-authors = 6 | title = TREM2 Acts Downstream of CD33 in Modulating Microglial Pathology in Alzheimer's Disease | journal = Neuron | volume = 103 | issue = 5 | pages = 820–835.e7 | date = September 2019 | pmid = 31301936 | pmc = 6728215 | doi = 10.1016/j.neuron.2019.06.010 }}</ref><ref>{{cite journal | vauthors = Chan G, White CC, Winn PA, Cimpean M, Replogle JM, Glick LR, Cuerdon NE, Ryan KJ, Johnson KA, Schneider JA, Bennett DA, Chibnik LB, Sperling RA, Bradshaw EM, De Jager PL | display-authors = 6 | title = CD33 modulates TREM2: convergence of Alzheimer loci | journal = Nature Neuroscience | volume = 18 | issue = 11 | pages = 1556–1558 | date = November 2015 | pmid = 26414614 | doi = 10.1038/nn.4126 | pmc = 4682915 }}</ref><ref>{{Cite news| vauthors = Stetka B |date=2022-01-30|title=How a hyperactive cell in the brain might trigger Alzheimer's disease |language=en |work=NPR |url= https://www.npr.org/sections/health-shots/2022/01/30/1076166807/how-a-hyperactive-cell-in-the-brain-might-trigger-alzheimers-disease|access-date=2022-02-17}}</ref> |
|||
Zhong et al reported that, in mice, stereotactic injection of sTREM2 or adeno-associated virus-mediated activation of sTREM2 reduced the amyloid plaque load and reduced functional memory deficits <ref>{{Cite journal |last=Zhong |first=Li |last2=Xu |first2=Ying |last3=Zhuo |first3=Rengong |last4=Wang |first4=Tingting |last5=Wang |first5=Kai |last6=Huang |first6=Ruizhi |last7=Wang |first7=Daxin |last8=Gao |first8=Yue |last9=Zhu |first9=Yifei |last10=Sheng |first10=Xuan |last11=Chen |first11=Kai |date=2019-12 |title=Soluble TREM2 ameliorates pathological phenotypes by modulating microglial functions in an Alzheimer’s disease model |url=http://www.nature.com/articles/s41467-019-09118-9 |journal=Nature Communications |language=en |volume=10 |issue=1 |pages=1365 |doi=10.1038/s41467-019-09118-9 |issn=2041-1723 |pmc=PMC6433910 |pmid=30911003}}</ref>. Moreover, sTREM2 stimulated microglial proliferation and homing toward amyloid plaques where amyloid-β uptake and degradation was increased. Interestingly, these effects were specifically mediated by microglia. Level of sTREM2 in the CSF might be a biomarker for AD and the associated inflammatory response <ref>{{Cite journal |last=Liu |first=Dan |last2=Cao |first2=Bing |last3=Zhao |first3=Yujia |last4=Huang |first4=Huanhuan |last5=McIntyre |first5=Roger S. |last6=Rosenblat |first6=Joshua D. |last7=Zhou |first7=Hui |date=2018-11 |title=Soluble TREM2 changes during the clinical course of Alzheimer’s disease: A meta-analysis |url=https://linkinghub.elsevier.com/retrieve/pii/S0304394018305834 |journal=Neuroscience Letters |language=en |volume=686 |pages=10–16 |doi=10.1016/j.neulet.2018.08.038}}</ref> <ref>{{Cite journal |last=Rauchmann |first=Boris-Stephan |last2=Schneider-Axmann |first2=Thomas |last3=Alexopoulos |first3=Panagiotis |last4=Perneczky |first4=Robert |date=2019-02 |title=CSF soluble TREM2 as a measure of immune response along the Alzheimer's disease continuum |url=https://linkinghub.elsevier.com/retrieve/pii/S0197458018303865 |journal=Neurobiology of Aging |language=en |volume=74 |pages=182–190 |doi=10.1016/j.neurobiolaging.2018.10.022 |pmc=PMC6331262 |pmid=30458365}}</ref> <ref>{{Cite journal |last=Piccio |first=Laura |last2=Deming |first2=Yuetiva |last3=Del-Águila |first3=Jorge L. |last4=Ghezzi |first4=Laura |last5=Holtzman |first5=David M. |last6=Fagan |first6=Anne M. |last7=Fenoglio |first7=Chiara |last8=Galimberti |first8=Daniela |last9=Borroni |first9=Barbara |last10=Cruchaga |first10=Carlos |date=2016-06 |title=Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status |url=http://link.springer.com/10.1007/s00401-016-1533-5 |journal=Acta Neuropathologica |language=en |volume=131 |issue=6 |pages=925–933 |doi=10.1007/s00401-016-1533-5 |issn=0001-6322 |pmc=PMC4867123 |pmid=26754641}}</ref>. |
|||
=== Cancer === |
=== Cancer === |
||
One feature of tumor growth and progression is an immune-suppressive TME, which contains and factors that prevent an anti-tumor immune response. Myeloid cells have been identified as important regulators (positive and negative) of anti-tumor immune responses. A high level of tumor-associated myeloid infiltrate correlates with shorter survival times of patients with solid tumors and could be a key driver of resistance to [[checkpoint inhibitor]] therapy. <ref>{{Cite journal |last=Awad |first=Robin Maximilian |last2=De Vlaeminck |first2=Yannick |last3=Maebe |first3=Johannes |last4=Goyvaerts |first4=Cleo |last5=Breckpot |first5=Karine |date=2018-08-31 |title=Turn Back the TIMe: Targeting Tumor Infiltrating Myeloid Cells to Revert Cancer Progression |url=https://www.frontiersin.org/article/10.3389/fimmu.2018.01977/full |journal=Frontiers in Immunology |volume=9 |pages=1977 |doi=10.3389/fimmu.2018.01977 |issn=1664-3224 |pmc=PMC6127274 |pmid=30233579}}</ref> <ref>{{Cite journal |last=Bingle |first=L. |last2=Brown |first2=N. J. |last3=Lewis |first3=C. E. |date=2002 |title=The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies |url=http://dx.doi.org/10.1002/path.1027 |journal=The Journal of Pathology |volume=196 |issue=3 |pages=254–265 |doi=10.1002/path.1027 |issn=0022-3417}}</ref> [[Myeloid cells]], including TAMs (M2-like TAMs), [[tumor-associated neutrophils]] (TANs), and monocytic myeloid-derived suppressor cells (mMDSCs), can have '''immune-suppressive''' functions that limit anti-tumor responses. Other myeloid cell populations, including M1-like TAMs and monocytes, can have '''stimulatory''' functions that promote antigen presentation and T-cell activation. |
|||
The immune system plays an intricate role in the development of [[cancer]]s, and can either be beneficial for a patient, or assist in the growth of a tumor. It has been found that TREM2 is important in the role myeloid cells play in cancer development. TREM2 is found to have an increased expression in macrophages that are responding to tumors, in both humans and in rodent models.<ref name=":34"/> TREM2 interacts with the tumor microenvironment in a multitude of ways, and has been found to be tumor suppressant through its down-regulation of the TLR4 pro-inflammatory signaling pathway.<ref name=":162"/> TREM2 has been found to have differential expression from healthy conditions in specific cancers, including lung cancer, gastric cancer, and perhaps gliomas and liver cancer as well.<ref name=":34"/> |
|||
Although TREM2 expression is low in most normal tissues, <ref name=":0">{{Cite journal |last=Molgora |first=Martina |last2=Esaulova |first2=Ekaterina |last3=Vermi |first3=William |last4=Hou |first4=Jinchao |last5=Chen |first5=Yun |last6=Luo |first6=Jingqin |last7=Brioschi |first7=Simone |last8=Bugatti |first8=Mattia |last9=Omodei |first9=Andrea Salvatore |last10=Ricci |first10=Biancamaria |last11=Fronick |first11=Catrina |date=2020-08 |title=TREM2 Modulation Remodels the Tumor Myeloid Landscape Enhancing Anti-PD-1 Immunotherapy |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867420308783 |journal=Cell |language=en |volume=182 |issue=4 |pages=886–900.e17 |doi=10.1016/j.cell.2020.07.013 |pmc=PMC7485282 |pmid=32783918}}</ref> <ref name=":3">{{Cite journal |last=Cheng |first=Xin |last2=Wang |first2=Xiaowei |last3=Nie |first3=Kechao |last4=Cheng |first4=Lin |last5=Zhang |first5=Zheyu |last6=Hu |first6=Yang |last7=Peng |first7=Weijun |date=2021 |title=Systematic Pan-Cancer Analysis Identifies TREM2 as an Immunological and Prognostic Biomarker |url=https://www.frontiersin.org/article/10.3389/fimmu.2021.646523 |journal=Frontiers in Immunology |volume=12 |doi=10.3389/fimmu.2021.646523 |issn=1664-3224 |pmc=PMC7925850 |pmid=33679809}}</ref> it is overexpressed in many human tumor types. TREM2+ macrophages were observed in 75% of the 126 samples in a multi-carcinoma tissue array, but not in peripheral tissues; the authors of this study concluded that TREM2 is a marker of tumor-infiltrating macrophages. <ref name=":0" /> TREM2 expression is increased on macrophages that infiltrate tumors in humans and mice.<ref name=":34" /> |
|||
In contrast to the evidence supporting TREM2's role as a tumor suppressant, it has also been found that increased activation and expression of TREM2 has deleterious effects on the disease.<ref name=":34"/> Specifically in gastric cancer, a greater expression of TREM2 is found to be correlated with a worse disease outcome, and in a model of esophageal adenocarcinoma, a reduction in TREM2 led to a more positive outcome.<ref name=":162" /> |
|||
Cheng et al compared levels of ''TREM2'' mRNA among 33 cancer tissues and matched normal tissues using datasets from [[The Cancer Genome Atlas]] (TCGA), and found higher levels of expression in tumor compared to normal tissues in 18 cancer types, including head and neck squamous cell carcinoma, colon adenocarcinoma, and glioblastoma, as well as gynecologic, liver, gastric, kidney, breast, bladder, and esophageal cancers. <ref name=":3" /> They also found the level of ''TREM2'' mRNA to be positively associated with tumor mutation burden and microsatellite instability in 12 cancer types and associated with level of DNA methylation in 20 tumor types. |
|||
Cheng et al reported that in invasive breast carcinoma, cervical squamous cell carcinoma and endocervical adenocarcinoma, kidney renal clear cell carcinoma, lung squamous cell carcinoma, skin cutaneous melanoma, and stomach adenocarcinoma, there is a negative correlation between expression of TREM2 and tumor infiltration by immune cells. <ref name=":3" /> To extend this analysis, researchers ''TREM2'' RNA expression in 9736 tumor and 8587 normal tissue samples from the TCGA and the GTEx projects and observed a consistent increase in ''TREM2'' levels in tumors. <ref name=":4">{{Cite journal |last=Binnewies |first=Mikhail |last2=Pollack |first2=Joshua L. |last3=Rudolph |first3=Joshua |last4=Dash |first4=Subhadra |last5=Abushawish |first5=Marwan |last6=Lee |first6=Tian |last7=Jahchan |first7=Nadine S. |last8=Canaday |first8=Pamela |last9=Lu |first9=Erick |last10=Norng |first10=Manith |last11=Mankikar |first11=Shilpa |date=2021-10 |title=Targeting TREM2 on tumor-associated macrophages enhances immunotherapy |url=https://linkinghub.elsevier.com/retrieve/pii/S2211124721013085 |journal=Cell Reports |language=en |volume=37 |issue=3 |pages=109844 |doi=10.1016/j.celrep.2021.109844}}</ref> These findings support the tumor-enriched expression of TREM2 and the importance of therapeutically targeting it. |
|||
High expression of TREM2 was associated with shorter survival times of patients with ovarian cancer, gastric cancer, lower-grade glioma, hepatocellular carcinoma, or renal clear cell carcinoma. <ref name=":3" /> <ref name=":4" /> In an analysis of the TGCA database, Molgora et al found an inverse correlation between TREM2 expression and overall survival and recurrence in patients with colorectal cancer and triple-negative breast cancer.<ref name=":0" /> |
|||
Research presented at the [https://www.pionyrtx.com/file.cfm/19/docs/2021-09-013_trem2%20poster-%20pathology%20visions%20revised_klp_nj.pdf 2021 Pathology Visions Conference (Abstract no. 10106]), reported the development and validation of the TREM2 immunohistochemical assay as a laboratory-developed test that can be used with clinical specimens to detect TREM2 in the TME. The assay detected TREM2<sup>+</sup> TAMs with high levels of sensitivity and specificity, across 6 prioritized tumor indications, confirming that TREM2<sup>+</sup> TAMs are highly enriched whereas TREM2 expression is absent from most normal tissues. [https://www.pionyrtx.com/file.cfm/19/docs/aacr%20py314%20poster-nj%20final%20after%20review.pdf Research presented at the 2021 AACR conference] reported that, in human ovarian and other tumor specimens, expression of TREM2 protein and mRNA was restricted to TAMs, with minimal expression by most other types of immune cells. Tumor infiltration by TREM2+, APOE+, C1Q+ macrophage is a biomarker for recurrence of clear-cell renal carcinoma and that these cells are also therapeutic targets. <ref name=":4" /> <ref>{{Cite journal |last=Obradovic |first=Aleksandar |last2=Chowdhury |first2=Nivedita |last3=Haake |first3=Scott M. |last4=Ager |first4=Casey |last5=Wang |first5=Vinson |last6=Vlahos |first6=Lukas |last7=Guo |first7=Xinzheng V. |last8=Aggen |first8=David H. |last9=Rathmell |first9=W. Kimryn |last10=Jonasch |first10=Eric |last11=Johnson |first11=Joyce E. |date=2021-05 |title=Single-cell protein activity analysis identifies recurrence-associated renal tumor macrophages |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867421005730 |journal=Cell |language=en |volume=184 |issue=11 |pages=2988–3005.e16 |doi=10.1016/j.cell.2021.04.038 |pmc=PMC8479759 |pmid=34019793}}</ref> TREM2+ macrophages from human tumors also express [[CD68]], [[CD163]], [[Colony stimulating factor 1 receptor|CSF1R]], and nuclear [[MAFB (gene)|MAFB]]. <ref name=":0" /> |
|||
=== Inflammatory bowel disease === |
=== Inflammatory bowel disease === |
||
| Line 39: | Line 53: | ||
=== Liver disease === |
=== Liver disease === |
||
TREM2 is expressed in a variety of liver cells, and is seen to play a role in multiple different inflammatory liver diseases.<ref name=":12">{{cite journal | vauthors = Coelho I, Duarte N, Macedo MP, Penha-Gonçalves C | title = Insights into Macrophage/Monocyte-Endothelial Cell Crosstalk in the Liver: A Role for Trem-2 | journal = Journal of Clinical Medicine | volume = 10 | issue = 6 | pages = 1248 | date = March 2021 | pmid = 33802948 | pmc = 8002813 | doi = 10.3390/jcm10061248 | doi-access = free }}</ref> It appears as though the expression of TREM2 in hepatic cells is related to a reduction in inflammation, with an increase in TREM2 expression in [[hepatic stellate cell]]s being related to decreased inflammatory response.<ref name=":42"/> TREM2 is also expressed in Kupffer cells, which are macrophages that are specific to the liver.<ref name=":12" /> |
|||
In liver diseases, it has been proposed that TREM2 expressing macrophages are able to interact with specific liver endothelial cells that had a certain expression profile. In this capacity, TREM2 may be allowing cell-to-cell communication that allows for liver recovery in the disease state.<ref name=":12" /> The TREM2/DAP12 complex leads to a decrease in inflammation in liver disease by inhibiting down-stream signaling molecules that activate pro-inflammatory cytokines and by inhibiting TLR4 signaling.<ref name=":42" /> In fatty liver disorders, the increase in lipids leads to a down-regulation of TREM2. This can be problematic in disease as proper functioning of TREM2 leads to lipid phagocytosis and a decrease in damage-causing entities, such as reactive oxygen species.<ref name=":42" /> |
In liver diseases, it has been proposed that TREM2 expressing macrophages are able to interact with specific liver endothelial cells that had a certain expression profile. In this capacity, TREM2 may be allowing cell-to-cell communication that allows for liver recovery in the disease state.<ref name=":12" /> The TREM2/DAP12 complex leads to a decrease in inflammation in liver disease by inhibiting down-stream signaling molecules that activate pro-inflammatory cytokines and by inhibiting TLR4 signaling.<ref name=":42" /> In fatty liver disorders, the increase in lipids leads to a down-regulation of TREM2. This can be problematic in disease as proper functioning of TREM2 leads to lipid phagocytosis and a decrease in damage-causing entities, such as reactive oxygen species.<ref name=":42" /> |
||
[[File:TREM2_NHD-2.jpg|thumb|Mutations in |
[[File:TREM2_NHD-2.jpg|thumb|Mutations in the TREM2 or TYROBP genes (encodes DAP12) can lead to development of PLOSL. This disease is characterized by dysfunctional microglia, bone cysts and fractures, frontal lobe syndrome, and dementia. Created with BioRender.com ]] |
||
=== |
=== PLOSL or Nasu–Hakola disease === |
||
[[ |
[[Polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy|PLOSL or Nasu–Hakola disease]] is a neurodegenerative disorder characterized by bone cysts, dementia, and early death and is associated with variants in the ''TYROBP'' gene (encodes DAP12 protein) and ''TREM2'' gene.<ref name=":112"/> Bone cysts in patients with PLOSL contain fat in lieu of bone marrow.<ref name=":152"/> In this disease, the main cell type in the brain that is affected is the microglia, where TREM2 is expressed.<ref name=":2">{{cite journal | vauthors = Mecca C, Giambanco I, Donato R, Arcuri C | title = Microglia and Aging: The Role of the TREM2-DAP12 and CX3CL1-CX3CR1 Axes | journal = International Journal of Molecular Sciences | volume = 19 | issue = 1 | pages = E318 | date = January 2018 | pmid = 29361745 | pmc = 5796261 | doi = 10.3390/ijms19010318 | doi-access = free }}</ref> Several recessive, inactivating mutations in ''TREM2'' and ''TYROBP'' (encodes DAP12 protein) have been identified that can cause PLOSL.<ref name=":102"/><ref>{{cite journal | vauthors = Paloneva J, Kestilä M, Wu J, Salminen A, Böhling T, Ruotsalainen V, Hakola P, Bakker AB, Phillips JH, Pekkarinen P, Lanier LL, Timonen T, Peltonen L | display-authors = 6 | title = Loss-of-function mutations in TYROBP (DAP12) result in a presenile dementia with bone cysts | journal = Nature Genetics | volume = 25 | issue = 3 | pages = 357–361 | date = July 2000 | pmid = 10888890 | doi = 10.1038/77153 | s2cid = 9243117 }}</ref><ref name=":20">{{cite journal | vauthors = Walter J | title = The Triggering Receptor Expressed on Myeloid Cells 2: A Molecular Link of Neuroinflammation and Neurodegenerative Diseases | journal = The Journal of Biological Chemistry | volume = 291 | issue = 9 | pages = 4334–4341 | date = February 2016 | pmid = 26694609 | pmc = 4813462 | doi = 10.1074/jbc.R115.704981 | doi-access = free }}</ref> The mutations prevent association between TREM2 and DAP12 or expression of shorter, non-functional forms of TREM2.<ref name=":152" /><ref name=":20" /> Loss of function of TREM2 signaling increases the inflammatory responses of microglia,<ref name=":2" /> reducing clearance of dead neurons and promoting inflammation and even formation of amyloid plaques.<ref name=":2" /> |
||
The mutations of TREM2 found in NHD generally lead to a receptor that cannot associate with the DAP12 signaling protein, the absence of the receptor, or the receptor is found to be a shorter, non-functional protein.<ref name=":152" /><ref name=":20" /> NHD microglia with mutated TREM2 or TYROBP are found to have reduced functionality in clearing dead neurons, induce a more pro-inflammatory phenotype, and even influences the formation of amyloid plaques.<ref name=":2" /> |
|||
=== Stroke === |
=== Stroke === |
||
[[Stroke|Ischemic stroke]], a leading cause of disability, has many pathways through which damage occurs |
[[Stroke|Ischemic stroke]], a leading cause of disability, has many pathways through which damage occurs. Microglia respond to the area of insult, and TREM2 appears to reduce the inflammatory phenotype caused by TLR signaling and microglial-mediated recovery.<ref name=":21">{{cite journal | vauthors = Gervois P, Lambrichts I | title = The Emerging Role of Triggering Receptor Expressed on Myeloid Cells 2 as a Target for Immunomodulation in Ischemic Stroke | journal = Frontiers in Immunology | volume = 10 | pages = 1668 | date = 2019 | pmid = 31379859 | pmc = 6650572 | doi = 10.3389/fimmu.2019.01668 | doi-access = free }}</ref> TREM2 signaling is activated by nucleotides and lipid mediators, which are secreted into the extracellular stroke environment by apoptotic neurons and cell/myelin debris. TREM2 signaling mediates microglial migration toward, and phagocytosis of, myelin debris and apoptotic cells. Microglial TREM2 appears to counteract the TLR-mediated response, decreasing the production of inflammatory cytokines. TREM2 is also involved in microglia migration and survival, and has been proposed to mediate their shift to a regenerative phenotype. TREM2-knockout mice have low microglial responses to a stroke, and have worse recovery after stroke. TREM2 therefore appears to activate the microglial response to damage.<ref>{{cite journal | vauthors = Ulrich JD, Holtzman DM | title = TREM2 Function in Alzheimer's Disease and Neurodegeneration | journal = ACS Chemical Neuroscience | volume = 7 | issue = 4 | pages = 420–427 | date = April 2016 | pmid = 26854967 | doi = 10.1021/acschemneuro.5b00313 }}</ref> One study reported that the expression of TREM2 on microglia associates with recovery from stroke, whereas TREM2 on macrophages is unrelated to the response.<ref name=":21" /> |
||
=== Other diseases === |
=== Other diseases === |
||
TREM2 has also been linked to additional disorders such as [[Amyotrophic lateral sclerosis|ALS]], [[Parkinson's disease]], and more dementia related conditions.<ref name=":102" /> |
TREM2 has also been linked to additional disorders such as [[Amyotrophic lateral sclerosis|ALS]], [[Parkinson's disease]], and more dementia related conditions.<ref name=":102" /> |
||
== Therapeutic |
== Therapeutic targeting of TREM2 == |
||
TREM2 has gained attention as a therapeutic target for a range of indications, including cancer, fibrosis, and neurodegenerative diseases; multiple companies are developing agents to target TREM2. However, TREM2 is likely to have distinct roles in the pathogenesis of these disorders, so therapeutic agents in development employ different approaches to modify TREM2 activity. |
|||
| ⚫ | |||
=== Cancer Immunotherapy === |
|||
[https://www.pionyrtx.com/pipeline/py314/ Pionyr Immunotherapeutics Inc] (Pionyr) has developed an anti-TREM2 afucosylated IgG1 monoclonal antibody, called [https://www.pionyrtx.com/file.cfm/19/docs/pionyrpy314_whitepaper_22june22_final.pdf PY314], which is designed to selectively deplete the TREM2-positive, immunosuppressive TAMs via antibody-dependent cell mediated cytotoxicity (ADCC) and/or antibody-dependent cell mediated phagocytosis (ADCP). |
|||
[https://www.pionyrtx.com/pipeline/py314/ Pionyr] researchers reported at the [https://www.pionyrtx.com/file.cfm/19/docs/aacr%20py314%20poster-nj%20final%20after%20review.pdf 2021 AACR conference (Abstract no. LB071]) and other conferences ([https://www.pionyrtx.com/file.cfm/19/docs/PY314_AACR-Nov19.pdf 2019 EORTC Abstract no. C104], [https://www.pionyrtx.com/file.cfm/19/docs/PY314_SITC-Nov19.pdf 2019 SITC abstract no. Abstract P800]) that administration of an antibody against mouse TREM2 (PY314m) to mice with syngeneic tumors reduced tumor growth and altered the immune composition in the TME. Depletion of TREM2-positive cells in tumors by PY314m led to recruitment of activated NK and CD8+ T cells and switched the TME to one in which the immune-activating (M1-like) macrophages predominate, thereby ‘tuning’ the myeloid infiltrate in the TME. |
|||
There is synergy between the checkpoint inhibitor [[Programmed cell death protein 1|anti-PD1]] and anti-TREM2. This synergy increases the abundance of intra-tumoral CD8+ T cells and inflammatory cytokines ([[Interferon gamma|IFNG]] and [[Tumor necrosis factor|TNF]]). Administration of mPY314 to tumor-bearing mice depletes TAMs and promotes anti-tumor immunity—as a single agent and in combination with anti–PD1. <ref name=":4" /> |
|||
A phase 1a/b trial is underway to characterize the safety and tolerability of PY314 as a single agent, and in combination with pembrolizumab (anti–PD1), in subjects with advanced refractory solid tumors, including those refractory to checkpoint inhibitors if approved for that indication ([https://clinicaltrials.gov/ct2/show/NCT04691375 NCT04691375]). The phase 1a portion of the study has evaluated PY314 (at 1, 3, 10, and 20 mg/kg) alone and in combination with 200 mg pembrolizumab in subjects with advanced solid tumors using a 3+3 dose escalation design, with subjects given intravenous doses once every 3 weeks. Pionyr researchers reported at [https://www.pionyrtx.com/file.cfm/19/docs/py314_poster_asco_2022.pdf ASCO 2022 (Abstract no. 2648]) that PY314 has been well tolerated, with an excellent safety profile as a single agent and in combination with pembrolizumab. A dose of 10 mg/kg has been selected as the recommended dose for an expansion study (phase 1b) in 6 tumor types. |
|||
Pionyr is currently the only company in clinical development with a TREM2-depleting monoclonal antibody for oncology. To date, PY314 appears to be well tolerated as a single agent and in combination with [[pembrolizumab]] (anti-PD1). |
|||
=== '''Neurodegenerative Diseases''' === |
|||
In the brain, TREM2 is expressed on microglia that regulate clearance of neuronal debris.<ref name=":34" /> Binding of apolipoproteins, such as ApoE, to TREM2 promotes phagocytosis of apoptotic neurons or the uptake of amyloid beta by microglia. <ref>{{Cite journal |last=Atagi |first=Yuka |last2=Liu |first2=Chia-Chen |last3=Painter |first3=Meghan M. |last4=Chen |first4=Xiao-Fen |last5=Verbeeck |first5=Christophe |last6=Zheng |first6=Honghua |last7=Li |first7=Xia |last8=Rademakers |first8=Rosa |last9=Kang |first9=Silvia S. |last10=Xu |first10=Huaxi |last11=Younkin |first11=Steven |date=2015-10 |title=Apolipoprotein E Is a Ligand for Triggering Receptor Expressed on Myeloid Cells 2 (TREM2) |url=https://linkinghub.elsevier.com/retrieve/pii/S0021925820495833 |journal=Journal of Biological Chemistry |language=en |volume=290 |issue=43 |pages=26043–26050 |doi=10.1074/jbc.M115.679043 |pmc=PMC4646257 |pmid=26374899}}</ref> Additionally, TREM2 interacts with pathological beta-amyloid oligomers,<ref>{{Cite journal |last=Zhong |first=Li |last2=Wang |first2=Zongqi |last3=Wang |first3=Daxin |last4=Wang |first4=Zhe |last5=Martens |first5=Yuka A. |last6=Wu |first6=Linbei |last7=Xu |first7=Ying |last8=Wang |first8=Kai |last9=Li |first9=Jianguo |last10=Huang |first10=Ruizhi |last11=Can |first11=Dan |date=2018-12 |title=Amyloid-beta modulates microglial responses by binding to the triggering receptor expressed on myeloid cells 2 (TREM2) |url=https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-018-0247-7 |journal=Molecular Neurodegeneration |language=en |volume=13 |issue=1 |pages=15 |doi=10.1186/s13024-018-0247-7 |issn=1750-1326 |pmc=PMC5870375 |pmid=29587871}}</ref> anionic and zwitterionic lipids, <ref name=":6">{{Cite journal |last=Wang |first=Yaming |last2=Cella |first2=Marina |last3=Mallinson |first3=Kaitlin |last4=Ulrich |first4=Jason D. |last5=Young |first5=Katherine L. |last6=Robinette |first6=Michelle L. |last7=Gilfillan |first7=Susan |last8=Krishnan |first8=Gokul M. |last9=Sudhakar |first9=Shwetha |last10=Zinselmeyer |first10=Bernd H. |last11=Holtzman |first11=David M. |date=2015-03 |title=TREM2 Lipid Sensing Sustains the Microglial Response in an Alzheimer’s Disease Model |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867415001270 |journal=Cell |language=en |volume=160 |issue=6 |pages=1061–1071 |doi=10.1016/j.cell.2015.01.049 |pmc=PMC4477963 |pmid=25728668}}</ref> and lipo- and apolipoproteins (APOE and CLU/APOJ),<ref>{{Cite journal |last=Yeh |first=Felix L. |last2=Wang |first2=Yuanyuan |last3=Tom |first3=Irene |last4=Gonzalez |first4=Lino C. |last5=Sheng |first5=Morgan |date=2016-07 |title=TREM2 Binds to Apolipoproteins, Including APOE and CLU/APOJ, and Thereby Facilitates Uptake of Amyloid-Beta by Microglia |url=https://linkinghub.elsevier.com/retrieve/pii/S0896627316302926 |journal=Neuron |language=en |volume=91 |issue=2 |pages=328–340 |doi=10.1016/j.neuron.2016.06.015}}</ref> which, together with amyloid-beta, form plaques characteristic of Alzheimer’s disease. Variants of ''TREM2'' that encode proteins with reduced affinity for ligands have been associated with Alzheimer’s disease. <ref>{{Cite journal |date=2013-10-17 |title=TREM2 and Neurodegenerative Disease |url=http://www.nejm.org/doi/10.1056/NEJMc1306509 |journal=New England Journal of Medicine |language=en |volume=369 |issue=16 |pages=1564–1570 |doi=10.1056/NEJMc1306509 |issn=0028-4793}}</ref> |
|||
TREM2 deficiency and haploinsufficiency promote accumulation of amyloid-beta due to dysfunctional responses of microglia, which become apoptotic and fail to cluster around amyloid-beta plaques. <ref name=":6" /> In mice, defective TREM2 function affects microglial responses to amyloid-beta plaques, exacerbating tissue damage, whereas TREM2 overexpression reduces pathology. <ref name=":7">{{Cite journal |last=Wang |first=Shoutang |last2=Mustafa |first2=Meer |last3=Yuede |first3=Carla M. |last4=Salazar |first4=Santiago Viveros |last5=Kong |first5=Philip |last6=Long |first6=Hua |last7=Ward |first7=Michael |last8=Siddiqui |first8=Omer |last9=Paul |first9=Robert |last10=Gilfillan |first10=Susan |last11=Ibrahim |first11=Adiljan |date=2020-09-07 |title=Anti-human TREM2 induces microglia proliferation and reduces pathology in an Alzheimer’s disease model |url=https://rupress.org/jem/article/doi/10.1084/jem.20200785/151887/Antihuman-TREM2-induces-microglia-proliferation |journal=Journal of Experimental Medicine |language=en |volume=217 |issue=9 |pages=e20200785 |doi=10.1084/jem.20200785 |issn=0022-1007 |pmc=PMC7478730 |pmid=32579671}}</ref> This study also found that an antibody agonist of TREM2 activates microglia and reduces amyloid beta plaques in mice. So, in the central nervous system,TREM2 deficiency results in impaired clearance of apoptotic neurons and inflammation that might contribute to brain degeneration. Patients with Alzheimer’s disease might therefore benefit from TREM2 activation to clear debris that promote neurodegeneration. <ref name=":7" /> |
|||
Given the links between loss of TREM2 function and neurodegenerative diseases, [[biotechnology]] companies are evaluating TREM2 agonists for treatment of neurodegenerative diseases. |
|||
AL002, an anti-TREM2 monoclonal antibody developed by [https://alector.com/pipeline/ Alector Therapeutics], is an agonists that stimulates TREM2 in microglia to activate metabolism and proliferation. AL002 is being tested in a phase 2 trial of patients with AD.<ref>{{ClinicalTrialsGov|NCT04592874|A Phase 2 Randomized, Double-Blind, Placebo-Controlled, Multicenter Study to Evaluate the Efficacy and Safety of AL002 in Participants With Early Alzheimer's Disease}}</ref> <ref>{{Cite web|title=Alector Moving Forward with AL002 Alzheimer Disease Trial|url=https://www.hcplive.com/view/alector-al002-alzheimer-disease-trial|access-date=2021-11-26|website=HCPLive}}</ref> Alector announced in a [https://investors.alector.com/news-releases/news-release-details/alector-reports-fourth-quarter-and-full-year-2021-financial press release] that a small number of serious adverse events occurred among subjects with 2 alleles of a specific ''APOE'' mutation in this trial ([https://clinicaltrials.gov/ct2/show/NCT04592874 NCT04592874]). Alector is amending their phase-2 trial protocol to exclude subjects with these mutations. |
|||
It is important to note that there are key differences between agents that target TREM2 for treatment of neurodegenerative diseases (such as AL002) vs [https://www.pionyrtx.com/pipeline/py314/ Pionyr’s PY314] for treatment of cancer. Whereas PY314 selectively depletes TREM2-expressing cells to activate an anti-tumor response, agents in development for neurodegenerative disorders, such as AL002, are agonists that stimulate TREM2 in microglia, to activate their metabolism and proliferation, and clearance of neuronal debris. |
|||
Currently, in humans, a [[phase II clinical trial]] of a compound called AL002 is ongoing, testing a treatment that is targeting TREM2 for efficacy.<ref>{{ClinicalTrialsGov|NCT04592874|A Phase 2 Randomized, Double-Blind, Placebo-Controlled, Multicenter Study to Evaluate the Efficacy and Safety of AL002 in Participants With Early Alzheimer's Disease}}</ref> Alector Inc. is testing a monoclonal antibody treatment that is being considered as a potential treatment for patients in earlier stages of Alzheimer's disease, with the goal of increasing TREM2 activity, and thus the brains immune response to the disease.<ref>{{Cite web|title=Alector Moving Forward with AL002 Alzheimer Disease Trial|url=https://www.hcplive.com/view/alector-al002-alzheimer-disease-trial|access-date=2021-11-26|website=HCPLive}}</ref> |
|||
=== Targeting sTREM2 === |
|||
Another clinical trial is in phase I for tolerability is assessing a therapeutic called PY314 for gastric cancer.<ref name=":6">{{Cite web|title=PY314 {{!}} TREM2 {{!}} Pionyr Immunotherapeutics|url=https://www.pionyrtx.com/pipeline/py314/|access-date=2021-11-26|website=www.pionyrtx.com}}</ref> The intended mechanism of this therapeutic is to reduce TREM2 expressing cells in the tumor microenvironment, and this would lead to an increase in an immune response to the tumor.<ref name=":6" /> |
|||
| ⚫ | A potential mechanism of intervention could be targeting the enzymes that cleave the ectodomain, adjusting the rate at which sTREM2 is released. In rodents, a potential therapeutic using this mechanism was used against AD pathology, and the rodents had smaller plaques than controls.<ref name=":34" /> |
||
== References == |
== References == |
||
Revision as of 23:36, 29 June 2022
Triggering receptor expressed on myeloid cells 2 (TREM2) is a protein that in humans is encoded by the TREM2 gene.[5][6][7] The TREM2 protein is expressed primarily in immune cells in different tissues. In the brain, TREM2 is expressed by microglia,[8] which are the central nervous system's immune response system.[9] In the liver, TREM2 is expressed by several cell types, including macrophages that respond to insults to the tissue.[10] In the bowel and intestine, TREM2 is found on dendritic cells.[11] TREM2 is overexpressed in many tumor types and is increasingly recognized as an important factor in development of inflammatory diseases and cancer. It therefore appears to be a good therapeutic target.
Gene
The TREM2 gene lies on the sixth chromosome in humans, specifically in location 6p21.1. The gene has 5 coding exon regions.[12][13] Alternative splicing of the TREM2 mRNA transcript leads to different isoforms of the protein being produced upon translation.[12] Specifically, TREM2 mRNA has 3 different isoforms containing three consistent exons, and two that vary between the isoforms.[14] Encoding for receptors in many different cell types, TREM2 mRNA is found in different organs across the body, but is most expressed in the brain, lungs, adrenal glands, placenta, gall bladder, and colon.[12] The TREM2 gene is present not only in humans, but in mice as well, which has allowed researchers to create a plethora of genetic models containing different mutations of the TREM2 gene to study the effects of these mutations in disease states.[15] In addition to the mouse, the TREM2 gene can be found in many animals along the evolutionary tree, including rats, dogs, monkeys and more.[16]
In the brain, TREM2 is expressed differentially between brain regions, with the highest levels of this protein being found in the hippocampus, the white matter, and the spinal cord. In humans and mice, the levels of TREM2 increase with age.[17]
Protein

The TREM2 receptor is a transmembrane protein that is made up of an extracellular region (also referred to as the ectodomain), the membrane traversing segment, and an intracellular component.[18] The extracellular component of TREM2 can bind different anionic ligands, specifically glycoproteins and lipids.[19][20] This ectodomain component includes an Ig-like V-type domain where ligands bind the receptor.[21] The TREM2 ectodomain is modified after the translation of the protein, which changes its affinity for different ligands.[14] The intracellular component of TREM2 does not have any signaling ability on its own; rather, it signals via the DNAX activator proteins 10 and 12 (DAP10 and DAP12). A single TREM2 molecule can interact with DAP10 and DAP12 at the same time.[20]
Part of the ectodomain of TREM2 can be processed by enzymes a disintegrin and metalloprotease 10 and 17 (ADAM10, ADAM17) and released as a soluble version, called soluble TREM2 (sTREM2).[14] This protein fragment is released into the sera and cerebral spinal fluid (CSF), and might serve as a biomarker for neurodegenerative and other disorders, but further studies are needed.[14]
Function

The TREM2 protein is found in immune cells termed myeloid cells, a category which include cells such as macrophages, granulocytes, monocytes, and dendritic cells.[23] In the brain, TREM2 is expressed on microglial cells,[17] which are analogous to the immune cells in other tissues and blood. Monocyte-, macrophage-, and neutrophil-mediated inflammatory responses can be stimulated through G protein-linked 7-transmembrane receptors (e.g., FPR1), Fc receptors, CD14 and Toll-like receptors (e.g., TLR4), and cytokine receptors (e.g., IFNGR1).[24][25] Engagement of these receptors can also prime myeloid cells to respond to other stimuli. Myeloid cells express receptors belonging to the immunoglobulin (Ig) superfamily, such as TREM2, or to the C-type lectin superfamily.[24][26]
On myeloid cells, TREM2 binds anionic molecules, free and bound to plasma membrane, including bacterial products, DNA, lipoproteins, phospholipids, glycoproteins, DNA, and bacterial fragments,[13][19][20][27] [28]. TREM2 binding of ligand results in phosphorylation at 2 tyrosines in the immunoreceptor tyrosine-based activation motif (ITAM) of DAP12 by SRC tyrosine kinases.[20] Spleen tyrosine kinase (Syk) interacts with these phosphorylation sites and activates the phosphatidylinositol-3 kinase (PI3K) signaling pathway, as well as other signaling molecules such as mTOR, MAPK, and ERK.[20][29] Association of TREM2 with DAP10 also activates the PI3K signaling pathway[30], leading to expression of transcription factors that include AP1, NF-κB, and NFAT.[29] The PI3K signaling pathway also increases intracellular calcium content, which activates calcium-dependent kinases.[29][30] TREM2 activation also affects expression of GAL1, GAL3, IL1RN, and progranulin, which modulate the immune response.[20]
TREM2 is expressed by microglia and osteoclasts, and is involved in development and/or maintenance of brain and bone.[20] In mice, TREM2 is involved in synaptic pruning, a process of shaping neuronal circuitry by microglia- and astrocyte-mediated removal of excessive synapses via phagocytosis.[14][31][32] TREM2 is also expressed by macrophages of adipose tissue, adrenal gland, and placenta[20].
Immunosuppressive tumor-associated macrophages (TAMs) have been characterized by expression of TREM2 [33] TREM2 signaling leads to downregulated transcription of genes that promote inflammation (Tnf, Il1b, and Nos2) [34], as well as release of cytokines that prevent activation of anti-tumor CD8+ T cells [35]. TREM2+ immunosuppressive TAMs correlate with the level of exhausted T cells in the human tumor microenvironment (TME) [36]. A TREM2+ TAM-rich TME therefore appears to be immunosuppressive and might promote resistance to cancer therapies, such as checkpoint inhibitors.
TREM2 signaling can antagonize Toll-like receptor (TLR) expression and signaling, resulting in reduced production of inflammatory cytokines by cultured mouse macrophages [20]. Conversely, TREM2 expression is reduced following inflammatory signaling induction by LPS (a TLR4 ligand) or interferon gamma (IFNγ) [37]. TREM2 exerts neuroprotective effects not only by producing anti-inflammatory cytokines, but also by promoting the clearance of abnormal proteins and phagocytosis of apoptotic neurons[14][38].
TREM2 signaling has been reported to have some proinflammatory effects, such as in inflammatory bowel diseases (IBD).[11] sTREM2 is believed to negatively regulate TREM2 signaling by acting as decoy receptors [39] sTREM might therefore have pro-inflammatory effects.[20] sTREM2 has been indicated in activating signaling pathways such as PI3K and ERK through an unidentified receptor.[40] Levels of sTREM2 are increased in cerebrospinal fluid (CSF) of patients with Alzheimer's disease (AD), and correlate with the CSF levels of AD biomarkers, namely t-tau and p-tau [41]
Association with diseases
TREM2 signaling has been associated with pathogenesis of several diseases. Variants of in the DAP12 (TYROBP) or TREM2 genes have been associated with polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (PLOSL or Nasu–Hakola disease).[42]

Alzheimer's disease
Variants of TREM2 have been associated with neurodegenerative disorders, including Alzheimer's disease (AD).[43] TREM2 is involved in the microglial response to the amyloid plaques that are characteristic of AD. Loss of TREM2 function reduces the responses of microglia to plaques, which then appear to take on a more toxic state.[43] Expression of TREM2 is closely tied to that of CD33.[44][45][46]
Zhong et al reported that, in mice, stereotactic injection of sTREM2 or adeno-associated virus-mediated activation of sTREM2 reduced the amyloid plaque load and reduced functional memory deficits [47]. Moreover, sTREM2 stimulated microglial proliferation and homing toward amyloid plaques where amyloid-β uptake and degradation was increased. Interestingly, these effects were specifically mediated by microglia. Level of sTREM2 in the CSF might be a biomarker for AD and the associated inflammatory response [48] [49] [50].
Cancer
One feature of tumor growth and progression is an immune-suppressive TME, which contains and factors that prevent an anti-tumor immune response. Myeloid cells have been identified as important regulators (positive and negative) of anti-tumor immune responses. A high level of tumor-associated myeloid infiltrate correlates with shorter survival times of patients with solid tumors and could be a key driver of resistance to checkpoint inhibitor therapy. [51] [52] Myeloid cells, including TAMs (M2-like TAMs), tumor-associated neutrophils (TANs), and monocytic myeloid-derived suppressor cells (mMDSCs), can have immune-suppressive functions that limit anti-tumor responses. Other myeloid cell populations, including M1-like TAMs and monocytes, can have stimulatory functions that promote antigen presentation and T-cell activation.
Although TREM2 expression is low in most normal tissues, [53] [54] it is overexpressed in many human tumor types. TREM2+ macrophages were observed in 75% of the 126 samples in a multi-carcinoma tissue array, but not in peripheral tissues; the authors of this study concluded that TREM2 is a marker of tumor-infiltrating macrophages. [53] TREM2 expression is increased on macrophages that infiltrate tumors in humans and mice.[20]
Cheng et al compared levels of TREM2 mRNA among 33 cancer tissues and matched normal tissues using datasets from The Cancer Genome Atlas (TCGA), and found higher levels of expression in tumor compared to normal tissues in 18 cancer types, including head and neck squamous cell carcinoma, colon adenocarcinoma, and glioblastoma, as well as gynecologic, liver, gastric, kidney, breast, bladder, and esophageal cancers. [54] They also found the level of TREM2 mRNA to be positively associated with tumor mutation burden and microsatellite instability in 12 cancer types and associated with level of DNA methylation in 20 tumor types.
Cheng et al reported that in invasive breast carcinoma, cervical squamous cell carcinoma and endocervical adenocarcinoma, kidney renal clear cell carcinoma, lung squamous cell carcinoma, skin cutaneous melanoma, and stomach adenocarcinoma, there is a negative correlation between expression of TREM2 and tumor infiltration by immune cells. [54] To extend this analysis, researchers TREM2 RNA expression in 9736 tumor and 8587 normal tissue samples from the TCGA and the GTEx projects and observed a consistent increase in TREM2 levels in tumors. [55] These findings support the tumor-enriched expression of TREM2 and the importance of therapeutically targeting it.
High expression of TREM2 was associated with shorter survival times of patients with ovarian cancer, gastric cancer, lower-grade glioma, hepatocellular carcinoma, or renal clear cell carcinoma. [54] [55] In an analysis of the TGCA database, Molgora et al found an inverse correlation between TREM2 expression and overall survival and recurrence in patients with colorectal cancer and triple-negative breast cancer.[53]
Research presented at the 2021 Pathology Visions Conference (Abstract no. 10106), reported the development and validation of the TREM2 immunohistochemical assay as a laboratory-developed test that can be used with clinical specimens to detect TREM2 in the TME. The assay detected TREM2+ TAMs with high levels of sensitivity and specificity, across 6 prioritized tumor indications, confirming that TREM2+ TAMs are highly enriched whereas TREM2 expression is absent from most normal tissues. Research presented at the 2021 AACR conference reported that, in human ovarian and other tumor specimens, expression of TREM2 protein and mRNA was restricted to TAMs, with minimal expression by most other types of immune cells. Tumor infiltration by TREM2+, APOE+, C1Q+ macrophage is a biomarker for recurrence of clear-cell renal carcinoma and that these cells are also therapeutic targets. [55] [56] TREM2+ macrophages from human tumors also express CD68, CD163, CSF1R, and nuclear MAFB. [53]
Inflammatory bowel disease
In inflammatory bowel disease (IBD), TREM2 expressed in human monocyte dendritic cells (DC),[11] the antigen presenting cells that are involved in the immune response in the intestine and bowel, appears to play a role in the disease.[57] For IBD, the expression of TREM2 is limited to inflamed sections of the bowel and has a pro-inflammatory effect as opposed to its role in other disease states.[11] TREM2 produces this inflammatory effect through increasing the release of pro-inflammatory cytokines, and may be involved in changes to the gut microbiome through DC mediated deaths of bacteria.[11]
Liver disease
TREM2 is expressed in a variety of liver cells, and is seen to play a role in multiple different inflammatory liver diseases.[58] It appears as though the expression of TREM2 in hepatic cells is related to a reduction in inflammation, with an increase in TREM2 expression in hepatic stellate cells being related to decreased inflammatory response.[10] TREM2 is also expressed in Kupffer cells, which are macrophages that are specific to the liver.[58]
In liver diseases, it has been proposed that TREM2 expressing macrophages are able to interact with specific liver endothelial cells that had a certain expression profile. In this capacity, TREM2 may be allowing cell-to-cell communication that allows for liver recovery in the disease state.[58] The TREM2/DAP12 complex leads to a decrease in inflammation in liver disease by inhibiting down-stream signaling molecules that activate pro-inflammatory cytokines and by inhibiting TLR4 signaling.[10] In fatty liver disorders, the increase in lipids leads to a down-regulation of TREM2. This can be problematic in disease as proper functioning of TREM2 leads to lipid phagocytosis and a decrease in damage-causing entities, such as reactive oxygen species.[10]

PLOSL or Nasu–Hakola disease
PLOSL or Nasu–Hakola disease is a neurodegenerative disorder characterized by bone cysts, dementia, and early death and is associated with variants in the TYROBP gene (encodes DAP12 protein) and TREM2 gene.[42] Bone cysts in patients with PLOSL contain fat in lieu of bone marrow.[29] In this disease, the main cell type in the brain that is affected is the microglia, where TREM2 is expressed.[59] Several recessive, inactivating mutations in TREM2 and TYROBP (encodes DAP12 protein) have been identified that can cause PLOSL.[21][60][61] The mutations prevent association between TREM2 and DAP12 or expression of shorter, non-functional forms of TREM2.[29][61] Loss of function of TREM2 signaling increases the inflammatory responses of microglia,[59] reducing clearance of dead neurons and promoting inflammation and even formation of amyloid plaques.[59]
Stroke
Ischemic stroke, a leading cause of disability, has many pathways through which damage occurs. Microglia respond to the area of insult, and TREM2 appears to reduce the inflammatory phenotype caused by TLR signaling and microglial-mediated recovery.[62] TREM2 signaling is activated by nucleotides and lipid mediators, which are secreted into the extracellular stroke environment by apoptotic neurons and cell/myelin debris. TREM2 signaling mediates microglial migration toward, and phagocytosis of, myelin debris and apoptotic cells. Microglial TREM2 appears to counteract the TLR-mediated response, decreasing the production of inflammatory cytokines. TREM2 is also involved in microglia migration and survival, and has been proposed to mediate their shift to a regenerative phenotype. TREM2-knockout mice have low microglial responses to a stroke, and have worse recovery after stroke. TREM2 therefore appears to activate the microglial response to damage.[63] One study reported that the expression of TREM2 on microglia associates with recovery from stroke, whereas TREM2 on macrophages is unrelated to the response.[62]
Other diseases
TREM2 has also been linked to additional disorders such as ALS, Parkinson's disease, and more dementia related conditions.[21]
Therapeutic targeting of TREM2
TREM2 has gained attention as a therapeutic target for a range of indications, including cancer, fibrosis, and neurodegenerative diseases; multiple companies are developing agents to target TREM2. However, TREM2 is likely to have distinct roles in the pathogenesis of these disorders, so therapeutic agents in development employ different approaches to modify TREM2 activity.
Cancer Immunotherapy
Pionyr Immunotherapeutics Inc (Pionyr) has developed an anti-TREM2 afucosylated IgG1 monoclonal antibody, called PY314, which is designed to selectively deplete the TREM2-positive, immunosuppressive TAMs via antibody-dependent cell mediated cytotoxicity (ADCC) and/or antibody-dependent cell mediated phagocytosis (ADCP).
Pionyr researchers reported at the 2021 AACR conference (Abstract no. LB071) and other conferences (2019 EORTC Abstract no. C104, 2019 SITC abstract no. Abstract P800) that administration of an antibody against mouse TREM2 (PY314m) to mice with syngeneic tumors reduced tumor growth and altered the immune composition in the TME. Depletion of TREM2-positive cells in tumors by PY314m led to recruitment of activated NK and CD8+ T cells and switched the TME to one in which the immune-activating (M1-like) macrophages predominate, thereby ‘tuning’ the myeloid infiltrate in the TME.
There is synergy between the checkpoint inhibitor anti-PD1 and anti-TREM2. This synergy increases the abundance of intra-tumoral CD8+ T cells and inflammatory cytokines (IFNG and TNF). Administration of mPY314 to tumor-bearing mice depletes TAMs and promotes anti-tumor immunity—as a single agent and in combination with anti–PD1. [55]
A phase 1a/b trial is underway to characterize the safety and tolerability of PY314 as a single agent, and in combination with pembrolizumab (anti–PD1), in subjects with advanced refractory solid tumors, including those refractory to checkpoint inhibitors if approved for that indication (NCT04691375). The phase 1a portion of the study has evaluated PY314 (at 1, 3, 10, and 20 mg/kg) alone and in combination with 200 mg pembrolizumab in subjects with advanced solid tumors using a 3+3 dose escalation design, with subjects given intravenous doses once every 3 weeks. Pionyr researchers reported at ASCO 2022 (Abstract no. 2648) that PY314 has been well tolerated, with an excellent safety profile as a single agent and in combination with pembrolizumab. A dose of 10 mg/kg has been selected as the recommended dose for an expansion study (phase 1b) in 6 tumor types.
Pionyr is currently the only company in clinical development with a TREM2-depleting monoclonal antibody for oncology. To date, PY314 appears to be well tolerated as a single agent and in combination with pembrolizumab (anti-PD1).
Neurodegenerative Diseases
In the brain, TREM2 is expressed on microglia that regulate clearance of neuronal debris.[20] Binding of apolipoproteins, such as ApoE, to TREM2 promotes phagocytosis of apoptotic neurons or the uptake of amyloid beta by microglia. [64] Additionally, TREM2 interacts with pathological beta-amyloid oligomers,[65] anionic and zwitterionic lipids, [66] and lipo- and apolipoproteins (APOE and CLU/APOJ),[67] which, together with amyloid-beta, form plaques characteristic of Alzheimer’s disease. Variants of TREM2 that encode proteins with reduced affinity for ligands have been associated with Alzheimer’s disease. [68]
TREM2 deficiency and haploinsufficiency promote accumulation of amyloid-beta due to dysfunctional responses of microglia, which become apoptotic and fail to cluster around amyloid-beta plaques. [66] In mice, defective TREM2 function affects microglial responses to amyloid-beta plaques, exacerbating tissue damage, whereas TREM2 overexpression reduces pathology. [69] This study also found that an antibody agonist of TREM2 activates microglia and reduces amyloid beta plaques in mice. So, in the central nervous system,TREM2 deficiency results in impaired clearance of apoptotic neurons and inflammation that might contribute to brain degeneration. Patients with Alzheimer’s disease might therefore benefit from TREM2 activation to clear debris that promote neurodegeneration. [69]
Given the links between loss of TREM2 function and neurodegenerative diseases, biotechnology companies are evaluating TREM2 agonists for treatment of neurodegenerative diseases.
AL002, an anti-TREM2 monoclonal antibody developed by Alector Therapeutics, is an agonists that stimulates TREM2 in microglia to activate metabolism and proliferation. AL002 is being tested in a phase 2 trial of patients with AD.[70] [71] Alector announced in a press release that a small number of serious adverse events occurred among subjects with 2 alleles of a specific APOE mutation in this trial (NCT04592874). Alector is amending their phase-2 trial protocol to exclude subjects with these mutations.
It is important to note that there are key differences between agents that target TREM2 for treatment of neurodegenerative diseases (such as AL002) vs Pionyr’s PY314 for treatment of cancer. Whereas PY314 selectively depletes TREM2-expressing cells to activate an anti-tumor response, agents in development for neurodegenerative disorders, such as AL002, are agonists that stimulate TREM2 in microglia, to activate their metabolism and proliferation, and clearance of neuronal debris.
Targeting sTREM2
A potential mechanism of intervention could be targeting the enzymes that cleave the ectodomain, adjusting the rate at which sTREM2 is released. In rodents, a potential therapeutic using this mechanism was used against AD pathology, and the rodents had smaller plaques than controls.[20]
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000095970 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000023992 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Bouchon A, Dietrich J, Colonna M (May 2000). "Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes". Journal of Immunology. 164 (10): 4991–4995. doi:10.4049/jimmunol.164.10.4991. PMID 10799849.
- ^ Paloneva J, Manninen T, Christman G, Hovanes K, Mandelin J, Adolfsson R, et al. (September 2002). "Mutations in two genes encoding different subunits of a receptor signaling complex result in an identical disease phenotype". American Journal of Human Genetics. 71 (3): 656–662. doi:10.1086/342259. PMC 379202. PMID 12080485.
- ^ "Entrez Gene: TREM2 triggering receptor expressed on myeloid cells 2".
- ^ Rodríguez-Gómez JA, Kavanagh E, Engskog-Vlachos P, Engskog MK, Herrera AJ, Espinosa-Oliva AM, et al. (July 2020). "Microglia: Agents of the CNS Pro-Inflammatory Response". Cells. 9 (7): E1717. doi:10.3390/cells9071717. PMC 7407646. PMID 32709045.
- ^ Masuda T, Sankowski R, Staszewski O, Prinz M (February 2020). "Microglia Heterogeneity in the Single-Cell Era". Cell Reports. 30 (5): 1271–1281. doi:10.1016/j.celrep.2020.01.010. PMID 32023447. S2CID 211047418.
- ^ a b c d Sun H, Feng J, Tang L (December 2020). "Function of TREM1 and TREM2 in Liver-Related Diseases". Cells. 9 (12): 2626. doi:10.3390/cells9122626. PMC 7762355. PMID 33297569.
- ^ a b c d e Genua M, Rutella S, Correale C, Danese S (October 2014). "The triggering receptor expressed on myeloid cells (TREM) in inflammatory bowel disease pathogenesis". Journal of Translational Medicine. 12: 293. doi:10.1186/s12967-014-0293-z. PMC 4231187. PMID 25347935.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c "TREM2 triggering receptor expressed on myeloid cells 2 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2021-11-02.
- ^ a b Natale G, Biagioni F, Busceti CL, Gambardella S, Limanaqi F, Fornai F (September 2019). "TREM Receptors Connecting Bowel Inflammation to Neurodegenerative Disorders". Cells. 8 (10): E1124. doi:10.3390/cells8101124. PMC 6829526. PMID 31546668.
- ^ a b c d e f Yang J, Fu Z, Zhang X, Xiong M, Meng L, Zhang Z (July 2020). "TREM2 ectodomain and its soluble form in Alzheimer's disease". Journal of Neuroinflammation. 17 (1): 204. doi:10.1186/s12974-020-01878-2. PMC 7341574. PMID 32635934.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Jackson Laboratory Search- TREM2". Jackson Laboratory.
- ^ Smith JR, Hayman GT, Wang SJ, Laulederkind SJ, Hoffman MJ, Kaldunski ML, et al. (January 2020). "The Year of the Rat: The Rat Genome Database at 20: a multi-species knowledgebase and analysis platform". Nucleic Acids Research. 48 (D1): D731–D742. doi:10.1093/nar/gkz1041. PMC 7145519. PMID 31713623.
- ^ a b Gratuze M, Leyns CE, Holtzman DM (December 2018). "New insights into the role of TREM2 in Alzheimer's disease". Molecular Neurodegeneration. 13 (1): 66. doi:10.1186/s13024-018-0298-9. PMC 6302500. PMID 30572908.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Kulkarni B, Kumar D, Cruz-Martins N, Sellamuthu S (October 2021). "Role of TREM2 in Alzheimer's Disease: A Long Road Ahead". Molecular Neurobiology. 58 (10): 5239–5252. doi:10.1007/s12035-021-02477-9. PMID 34275100. S2CID 236090999.
- ^ a b Hamerman JA, Pottle J, Ni M, He Y, Zhang ZY, Buckner JH (January 2016). "Negative regulation of TLR signaling in myeloid cells--implications for autoimmune diseases". Immunological Reviews. 269 (1): 212–227. doi:10.1111/imr.12381. PMC 4703580. PMID 26683155.
- ^ a b c d e f g h i j k l m Deczkowska A, Weiner A, Amit I (June 2020). "The Physiology, Pathology, and Potential Therapeutic Applications of the TREM2 Signaling Pathway". Cell. 181 (6): 1207–1217. doi:10.1016/j.cell.2020.05.003. PMID 32531244. S2CID 219572314.
- ^ a b c Dardiotis E, Siokas V, Pantazi E, Dardioti M, Rikos D, Xiromerisiou G, et al. (May 2017). "A novel mutation in TREM2 gene causing Nasu-Hakola disease and review of the literature". Neurobiology of Aging. 53: 194.e13–194.e22. doi:10.1016/j.neurobiolaging.2017.01.015. PMID 28214109. S2CID 22618858.
- ^ Kober DL, Alexander-Brett JM, Karch CM, Cruchaga C, Colonna M, Holtzman MJ, Brett TJ (December 2016). "Neurodegenerative disease mutations in TREM2 reveal a functional surface and distinct loss-of-function mechanisms". eLife. 5: e20391. doi:10.7554/eLife.20391. PMC 5173322. PMID 27995897.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ De Kleer I, Willems F, Lambrecht B, Goriely S (2014). "Ontogeny of myeloid cells". Frontiers in Immunology. 5: 423. doi:10.3389/fimmu.2014.00423. PMC 4153297. PMID 25232355.
- ^ a b Futosi K, Fodor S, Mócsai A (November 2013). "Neutrophil cell surface receptors and their intracellular signal transduction pathways". International Immunopharmacology. 17 (3): 638–650. doi:10.1016/j.intimp.2013.06.034. PMC 3827506. PMID 23994464.
- ^ Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. (January 2018). "Inflammatory responses and inflammation-associated diseases in organs". Oncotarget. 9 (6): 7204–7218. doi:10.18632/oncotarget.23208. PMC 5805548. PMID 29467962.
- ^ Sancho D, Reis e Sousa C (February 2013). "Sensing of cell death by myeloid C-type lectin receptors". Current Opinion in Immunology. 25 (1): 46–52. doi:10.1016/j.coi.2012.12.007. PMC 4480265. PMID 23332826.
- ^ Kober DL, Brett TJ (June 2017). "TREM2-Ligand Interactions in Health and Disease". Journal of Molecular Biology. 429 (11): 1607–1629. doi:10.1016/j.jmb.2017.04.004. PMC 5485854. PMID 28432014.
- ^ Kober, Daniel L.; Brett, Tom J. (2017-06). "TREM2-Ligand Interactions in Health and Disease". Journal of Molecular Biology. 429 (11): 1607–1629. doi:10.1016/j.jmb.2017.04.004. PMC 5485854. PMID 28432014.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b c d e Xing J, Titus AR, Humphrey MB (2015). "The TREM2-DAP12 signaling pathway in Nasu-Hakola disease: a molecular genetics perspective". Research and Reports in Biochemistry. 5: 89–100. doi:10.2147/RRBC.S58057. PMC 4605443. PMID 26478868.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Qiu H, Shao Z, Wen X, Jiang J, Ma Q, Wang Y, et al. (2021). "TREM2: Keeping Pace With Immune Checkpoint Inhibitors in Cancer Immunotherapy". Frontiers in Immunology. 12: 716710. doi:10.3389/fimmu.2021.716710. PMC 8446424. PMID 34539652.
- ^ Hong S, Dissing-Olesen L, Stevens B (February 2016). "New insights on the role of microglia in synaptic pruning in health and disease". Current Opinion in Neurobiology. 36: 128–134. doi:10.1016/j.conb.2015.12.004. PMC 5479435. PMID 26745839.
- ^ Filipello, Fabia; Morini, Raffaella; Corradini, Irene; Zerbi, Valerio; Canzi, Alice; Michalski, Bernadeta; Erreni, Marco; Markicevic, Marija; Starvaggi-Cucuzza, Chiara; Otero, Karel; Piccio, Laura (2018-05). "The Microglial Innate Immune Receptor TREM2 Is Required for Synapse Elimination and Normal Brain Connectivity". Immunity. 48 (5): 979–991.e8. doi:10.1016/j.immuni.2018.04.016. ISSN 1074-7613.
{{cite journal}}: Check date values in:|date=(help) - ^ Molgora, Martina; Colonna, Marco (2021-06). "Turning enemies into allies—reprogramming tumor-associated macrophages for cancer therapy". Med. 2 (6): 666–681. doi:10.1016/j.medj.2021.05.001. PMC 8238417. PMID 34189494.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Takahashi, Kazuya; Rochford, Christian D.P.; Neumann, Harald (2005-02-21). "Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2". Journal of Experimental Medicine. 201 (4): 647–657. doi:10.1084/jem.20041611. ISSN 1540-9538. PMC 2213053. PMID 15728241.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Molgora, Martina; Esaulova, Ekaterina; Vermi, William; Hou, Jinchao; Chen, Yun; Luo, Jingqin; Brioschi, Simone; Bugatti, Mattia; Omodei, Andrea Salvatore; Ricci, Biancamaria; Fronick, Catrina (2020-08). "TREM2 Modulation Remodels the Tumor Myeloid Landscape Enhancing Anti-PD-1 Immunotherapy". Cell. 182 (4): 886–900.e17. doi:10.1016/j.cell.2020.07.013. PMC 7485282. PMID 32783918.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Binnewies, Mikhail; Pollack, Joshua L.; Rudolph, Joshua; Dash, Subhadra; Abushawish, Marwan; Lee, Tian; Jahchan, Nadine S.; Canaday, Pamela; Lu, Erick; Norng, Manith; Mankikar, Shilpa (2021-10). "Targeting TREM2 on tumor-associated macrophages enhances immunotherapy". Cell Reports. 37 (3): 109844. doi:10.1016/j.celrep.2021.109844.
{{cite journal}}: Check date values in:|date=(help) - ^ Gao, Xiaoling; Dong, Yanting; Liu, Zhuola; Niu, Bo (2013-03). "Silencing of triggering receptor expressed on myeloid cells-2 enhances the inflammatory responses of alveolar macrophages to lipopolysaccharide". Molecular Medicine Reports. 7 (3): 921–926. doi:10.3892/mmr.2013.1268. ISSN 1791-2997.
{{cite journal}}: Check date values in:|date=(help) - ^ Takahashi, Kazuya; Rochford, Christian D.P.; Neumann, Harald (2005-02-21). "Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2". Journal of Experimental Medicine. 201 (4): 647–657. doi:10.1084/jem.20041611. ISSN 1540-9538. PMC 2213053. PMID 15728241.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Piccio, Laura; Buonsanti, Cecilia; Cella, Marina; Tassi, Ilaria; Schmidt, Robert E.; Fenoglio, Chiara; Rinker, John; Naismith, Robert T.; Panina-Bordignon, Paola; Passini, Nadia; Galimberti, Daniela (2008-11). "Identification of soluble TREM-2 in the cerebrospinal fluid and its association with multiple sclerosis and CNS inflammation". Brain. 131 (11): 3081–3091. doi:10.1093/brain/awn217. ISSN 1460-2156. PMC 2577803. PMID 18790823.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Konishi H, Kiyama H (2018). "Microglial TREM2/DAP12 Signaling: A Double-Edged Sword in Neural Diseases". Frontiers in Cellular Neuroscience. 12: 206. doi:10.3389/fncel.2018.00206. PMC 6087757. PMID 30127720.
- ^ Yang, Jiaolong; Fu, Zhihui; Zhang, Xingyu; Xiong, Min; Meng, Lanxia; Zhang, Zhentao (2020-12). "TREM2 ectodomain and its soluble form in Alzheimer's disease". Journal of Neuroinflammation. 17 (1): 204. doi:10.1186/s12974-020-01878-2. ISSN 1742-2094. PMC 7341574. PMID 32635934.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ a b Bianchin MM, Capella HM, Chaves DL, Steindel M, Grisard EC, Ganev GG, et al. (February 2004). "Nasu-Hakola disease (polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy--PLOSL): a dementia associated with bone cystic lesions. From clinical to genetic and molecular aspects". Cellular and Molecular Neurobiology. 24 (1): 1–24. doi:10.1023/b:cemn.0000012721.08168.ee. PMID 15049507. S2CID 7089775.
- ^ a b Shi Y, Holtzman DM (December 2018). "Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight". Nature Reviews. Immunology. 18 (12): 759–772. doi:10.1038/s41577-018-0051-1. PMC 6425488. PMID 30140051.
- ^ Griciuc A, Patel S, Federico AN, Choi SH, Innes BJ, Oram MK, et al. (September 2019). "TREM2 Acts Downstream of CD33 in Modulating Microglial Pathology in Alzheimer's Disease". Neuron. 103 (5): 820–835.e7. doi:10.1016/j.neuron.2019.06.010. PMC 6728215. PMID 31301936.
- ^ Chan G, White CC, Winn PA, Cimpean M, Replogle JM, Glick LR, et al. (November 2015). "CD33 modulates TREM2: convergence of Alzheimer loci". Nature Neuroscience. 18 (11): 1556–1558. doi:10.1038/nn.4126. PMC 4682915. PMID 26414614.
- ^ Stetka B (2022-01-30). "How a hyperactive cell in the brain might trigger Alzheimer's disease". NPR. Retrieved 2022-02-17.
- ^ Zhong, Li; Xu, Ying; Zhuo, Rengong; Wang, Tingting; Wang, Kai; Huang, Ruizhi; Wang, Daxin; Gao, Yue; Zhu, Yifei; Sheng, Xuan; Chen, Kai (2019-12). "Soluble TREM2 ameliorates pathological phenotypes by modulating microglial functions in an Alzheimer's disease model". Nature Communications. 10 (1): 1365. doi:10.1038/s41467-019-09118-9. ISSN 2041-1723. PMC 6433910. PMID 30911003.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Liu, Dan; Cao, Bing; Zhao, Yujia; Huang, Huanhuan; McIntyre, Roger S.; Rosenblat, Joshua D.; Zhou, Hui (2018-11). "Soluble TREM2 changes during the clinical course of Alzheimer's disease: A meta-analysis". Neuroscience Letters. 686: 10–16. doi:10.1016/j.neulet.2018.08.038.
{{cite journal}}: Check date values in:|date=(help) - ^ Rauchmann, Boris-Stephan; Schneider-Axmann, Thomas; Alexopoulos, Panagiotis; Perneczky, Robert (2019-02). "CSF soluble TREM2 as a measure of immune response along the Alzheimer's disease continuum". Neurobiology of Aging. 74: 182–190. doi:10.1016/j.neurobiolaging.2018.10.022. PMC 6331262. PMID 30458365.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Piccio, Laura; Deming, Yuetiva; Del-Águila, Jorge L.; Ghezzi, Laura; Holtzman, David M.; Fagan, Anne M.; Fenoglio, Chiara; Galimberti, Daniela; Borroni, Barbara; Cruchaga, Carlos (2016-06). "Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status". Acta Neuropathologica. 131 (6): 925–933. doi:10.1007/s00401-016-1533-5. ISSN 0001-6322. PMC 4867123. PMID 26754641.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Awad, Robin Maximilian; De Vlaeminck, Yannick; Maebe, Johannes; Goyvaerts, Cleo; Breckpot, Karine (2018-08-31). "Turn Back the TIMe: Targeting Tumor Infiltrating Myeloid Cells to Revert Cancer Progression". Frontiers in Immunology. 9: 1977. doi:10.3389/fimmu.2018.01977. ISSN 1664-3224. PMC 6127274. PMID 30233579.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Bingle, L.; Brown, N. J.; Lewis, C. E. (2002). "The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies". The Journal of Pathology. 196 (3): 254–265. doi:10.1002/path.1027. ISSN 0022-3417.
- ^ a b c d Molgora, Martina; Esaulova, Ekaterina; Vermi, William; Hou, Jinchao; Chen, Yun; Luo, Jingqin; Brioschi, Simone; Bugatti, Mattia; Omodei, Andrea Salvatore; Ricci, Biancamaria; Fronick, Catrina (2020-08). "TREM2 Modulation Remodels the Tumor Myeloid Landscape Enhancing Anti-PD-1 Immunotherapy". Cell. 182 (4): 886–900.e17. doi:10.1016/j.cell.2020.07.013. PMC 7485282. PMID 32783918.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b c d Cheng, Xin; Wang, Xiaowei; Nie, Kechao; Cheng, Lin; Zhang, Zheyu; Hu, Yang; Peng, Weijun (2021). "Systematic Pan-Cancer Analysis Identifies TREM2 as an Immunological and Prognostic Biomarker". Frontiers in Immunology. 12. doi:10.3389/fimmu.2021.646523. ISSN 1664-3224. PMC 7925850. PMID 33679809.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ a b c d Binnewies, Mikhail; Pollack, Joshua L.; Rudolph, Joshua; Dash, Subhadra; Abushawish, Marwan; Lee, Tian; Jahchan, Nadine S.; Canaday, Pamela; Lu, Erick; Norng, Manith; Mankikar, Shilpa (2021-10). "Targeting TREM2 on tumor-associated macrophages enhances immunotherapy". Cell Reports. 37 (3): 109844. doi:10.1016/j.celrep.2021.109844.
{{cite journal}}: Check date values in:|date=(help) - ^ Obradovic, Aleksandar; Chowdhury, Nivedita; Haake, Scott M.; Ager, Casey; Wang, Vinson; Vlahos, Lukas; Guo, Xinzheng V.; Aggen, David H.; Rathmell, W. Kimryn; Jonasch, Eric; Johnson, Joyce E. (2021-05). "Single-cell protein activity analysis identifies recurrence-associated renal tumor macrophages". Cell. 184 (11): 2988–3005.e16. doi:10.1016/j.cell.2021.04.038. PMC 8479759. PMID 34019793.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Stagg AJ (2018). "Intestinal Dendritic Cells in Health and Gut Inflammation". Frontiers in Immunology. 9: 2883. doi:10.3389/fimmu.2018.02883. PMC 6291504. PMID 30574151.
- ^ a b c Coelho I, Duarte N, Macedo MP, Penha-Gonçalves C (March 2021). "Insights into Macrophage/Monocyte-Endothelial Cell Crosstalk in the Liver: A Role for Trem-2". Journal of Clinical Medicine. 10 (6): 1248. doi:10.3390/jcm10061248. PMC 8002813. PMID 33802948.
- ^ a b c Mecca C, Giambanco I, Donato R, Arcuri C (January 2018). "Microglia and Aging: The Role of the TREM2-DAP12 and CX3CL1-CX3CR1 Axes". International Journal of Molecular Sciences. 19 (1): E318. doi:10.3390/ijms19010318. PMC 5796261. PMID 29361745.
- ^ Paloneva J, Kestilä M, Wu J, Salminen A, Böhling T, Ruotsalainen V, et al. (July 2000). "Loss-of-function mutations in TYROBP (DAP12) result in a presenile dementia with bone cysts". Nature Genetics. 25 (3): 357–361. doi:10.1038/77153. PMID 10888890. S2CID 9243117.
- ^ a b Walter J (February 2016). "The Triggering Receptor Expressed on Myeloid Cells 2: A Molecular Link of Neuroinflammation and Neurodegenerative Diseases". The Journal of Biological Chemistry. 291 (9): 4334–4341. doi:10.1074/jbc.R115.704981. PMC 4813462. PMID 26694609.
- ^ a b Gervois P, Lambrichts I (2019). "The Emerging Role of Triggering Receptor Expressed on Myeloid Cells 2 as a Target for Immunomodulation in Ischemic Stroke". Frontiers in Immunology. 10: 1668. doi:10.3389/fimmu.2019.01668. PMC 6650572. PMID 31379859.
- ^ Ulrich JD, Holtzman DM (April 2016). "TREM2 Function in Alzheimer's Disease and Neurodegeneration". ACS Chemical Neuroscience. 7 (4): 420–427. doi:10.1021/acschemneuro.5b00313. PMID 26854967.
- ^ Atagi, Yuka; Liu, Chia-Chen; Painter, Meghan M.; Chen, Xiao-Fen; Verbeeck, Christophe; Zheng, Honghua; Li, Xia; Rademakers, Rosa; Kang, Silvia S.; Xu, Huaxi; Younkin, Steven (2015-10). "Apolipoprotein E Is a Ligand for Triggering Receptor Expressed on Myeloid Cells 2 (TREM2)". Journal of Biological Chemistry. 290 (43): 26043–26050. doi:10.1074/jbc.M115.679043. PMC 4646257. PMID 26374899.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Zhong, Li; Wang, Zongqi; Wang, Daxin; Wang, Zhe; Martens, Yuka A.; Wu, Linbei; Xu, Ying; Wang, Kai; Li, Jianguo; Huang, Ruizhi; Can, Dan (2018-12). "Amyloid-beta modulates microglial responses by binding to the triggering receptor expressed on myeloid cells 2 (TREM2)". Molecular Neurodegeneration. 13 (1): 15. doi:10.1186/s13024-018-0247-7. ISSN 1750-1326. PMC 5870375. PMID 29587871.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ a b Wang, Yaming; Cella, Marina; Mallinson, Kaitlin; Ulrich, Jason D.; Young, Katherine L.; Robinette, Michelle L.; Gilfillan, Susan; Krishnan, Gokul M.; Sudhakar, Shwetha; Zinselmeyer, Bernd H.; Holtzman, David M. (2015-03). "TREM2 Lipid Sensing Sustains the Microglial Response in an Alzheimer's Disease Model". Cell. 160 (6): 1061–1071. doi:10.1016/j.cell.2015.01.049. PMC 4477963. PMID 25728668.
{{cite journal}}: Check date values in:|date=(help); no-break space character in|first10=at position 6 (help); no-break space character in|first11=at position 6 (help); no-break space character in|first4=at position 6 (help); no-break space character in|first5=at position 10 (help); no-break space character in|first6=at position 9 (help); no-break space character in|first8=at position 6 (help)CS1 maint: PMC format (link) - ^ Yeh, Felix L.; Wang, Yuanyuan; Tom, Irene; Gonzalez, Lino C.; Sheng, Morgan (2016-07). "TREM2 Binds to Apolipoproteins, Including APOE and CLU/APOJ, and Thereby Facilitates Uptake of Amyloid-Beta by Microglia". Neuron. 91 (2): 328–340. doi:10.1016/j.neuron.2016.06.015.
{{cite journal}}: Check date values in:|date=(help) - ^ "TREM2 and Neurodegenerative Disease". New England Journal of Medicine. 369 (16): 1564–1570. 2013-10-17. doi:10.1056/NEJMc1306509. ISSN 0028-4793.
- ^ a b Wang, Shoutang; Mustafa, Meer; Yuede, Carla M.; Salazar, Santiago Viveros; Kong, Philip; Long, Hua; Ward, Michael; Siddiqui, Omer; Paul, Robert; Gilfillan, Susan; Ibrahim, Adiljan (2020-09-07). "Anti-human TREM2 induces microglia proliferation and reduces pathology in an Alzheimer's disease model". Journal of Experimental Medicine. 217 (9): e20200785. doi:10.1084/jem.20200785. ISSN 0022-1007. PMC 7478730. PMID 32579671.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Clinical trial number NCT04592874 for "A Phase 2 Randomized, Double-Blind, Placebo-Controlled, Multicenter Study to Evaluate the Efficacy and Safety of AL002 in Participants With Early Alzheimer's Disease" at ClinicalTrials.gov
- ^ "Alector Moving Forward with AL002 Alzheimer Disease Trial". HCPLive. Retrieved 2021-11-26.