Unicompartmental knee arthroplasty: Difference between revisions
Cymru.lass (talk | contribs) tighten more |
copyedit; trim redundant older refs per WP:OVERCITE; rv content per WP:NOTGUIDE; add review using Citation bot |
||
| Line 11: | Line 11: | ||
HCPCSlevel2 = |
HCPCSlevel2 = |
||
}} |
}} |
||
'''Unicompartmental knee arthroplasty''' is a [[surgical procedure]] used to relieve [[arthritis]] in one of the [[knee]] compartments in which the damaged parts of the knee are replaced. UKA surgery may reduce post-operative pain and have a shorter recovery period than a [[total knee replacement]] procedure.<ref name="pmid18180388">{{cite journal |vauthors=Borus T, Thornhill T |title=Unicompartmental knee arthroplasty |journal=J Am Acad Orthop Surg |volume=16 |issue=1 |pages=9–18 |date=January 2008 |pmid=18180388 |doi= |url=http://www.jaaos.org/cgi/pmidlookup?view=long&pmid=18180388}}</ref> Moreover, UKAs may |
'''Unicompartmental knee arthroplasty''' (UKA) is a [[surgical procedure]] used to relieve [[arthritis]] in one of the [[knee]] compartments in which the damaged parts of the knee are replaced. UKA surgery may reduce post-operative pain and have a shorter recovery period than a [[total knee replacement]] procedure,<ref name="wu">{{cite journal|pmc=5371236|year=2017|last1=Santoso|first1=M. B|title=Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review|journal=Journal of Orthopaedic Surgery and Research|volume=12|issue=1|pages=50|last2=Wu|first2=L|doi=10.1186/s13018-017-0552-9|pmid=28351371}}</ref><ref name="pmid18180388">{{cite journal |vauthors=Borus T, Thornhill T |title=Unicompartmental knee arthroplasty |journal=J Am Acad Orthop Surg |volume=16 |issue=1 |pages=9–18 |date=January 2008 |pmid=18180388 |doi= |url=http://www.jaaos.org/cgi/pmidlookup?view=long&pmid=18180388}}</ref> particularly in people over 75 years of age.<ref name="siman">{{cite journal|pmid=28215968|year=2017|last1=Siman|first1=H|title=Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates|journal=The Journal of Arthroplasty|volume=32|issue=6|pages=1792–1797|last2=Kamath|first2=A. F|last3=Carrillo|first3=N|last4=Harmsen|first4=W. S|last5=Pagnano|first5=M. W|last6=Sierra|first6=R. J|doi=10.1016/j.arth.2017.01.020}}</ref> Moreover, UKAs may require a smaller [[Surgical incision|incision]], less tissue damage, and faster recovery times.<ref name="pmid18180388"/> |
||
In the United States, the procedure constitutes approximately 8% of [[knee arthroplasty|knee arthroplasties]].<ref>{{cite journal |vauthors=Riddle DL, Jiranek WA, McGlynn FJ |title=Yearly incidence of unicompartmental knee arthroplasty in the United States |journal=J Arthroplasty |volume=23 |issue=3 |pages=408–12 |date=April 2008 |pmid=18358380 |doi=10.1016/j.arth.2007.04.012 |url=}}</ref> |
In the United States, the procedure constitutes approximately 8% of [[knee arthroplasty|knee arthroplasties]].<ref>{{cite journal |vauthors=Riddle DL, Jiranek WA, McGlynn FJ |title=Yearly incidence of unicompartmental knee arthroplasty in the United States |journal=J Arthroplasty |volume=23 |issue=3 |pages=408–12 |date=April 2008 |pmid=18358380 |doi=10.1016/j.arth.2007.04.012 |url=}}</ref> In comparisons with a more extensive surgical procedure called [[high tibial osteotomy]], UKA has equal or better outcomes.<ref name=wu/><ref name="han">{{cite journal|pmc=5815788|year=2017|last1=Han|first1=S. B|title=Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy|journal=Medicine|volume=96|issue=50|pages=e9268|last2=Kyung|first2=H. S|last3=Seo|first3=I. W|last4=Shin|first4=Y. S|doi=10.1097/MD.0000000000009268|pmid=29390376}}</ref> |
||
==Background== |
==Background== |
||
In the early 1950s, Duncan C. McKeever theorized that osteoarthritis could be isolated to only one compartment of the knee joint,<ref name="pmid18180388"/> and that replacement of the entire knee might not be necessary if only one |
In the early 1950s, Duncan C. McKeever theorized that osteoarthritis could be isolated to only one compartment of the knee joint,<ref name="pmid18180388"/> and that replacement of the entire knee might not be necessary if only one knee compartment were affected.<ref name="pmid18180388"/><ref>{{cite web|last=Gibbon|first=Tony|title=Partial Knee Replacement|url=http://tony-gibbon.co.uk/treatment/knee-treatment/treatments/partial-knee-replacement|publisher=North Yorkshire Orthopaedic Specialists|accessdate=1 February 2013}}</ref> The UKA concept was designed to cause less trauma or damage than traditional total knee replacement by removing less bone and trying to maintain most of the person’s bone and anatomy.<ref name="pmid18180388"/> The concept was also designed to use smaller implants and thereby keep most of the person’s bone, helping them return to normal function faster.<ref name=siman/><ref name="pmid18180388"/> |
||
Initially, UKAs were not always successful, because the implants were poorly designed, |
Initially, UKAs were not always successful, because the implants were poorly designed, people needing the surgery were not thoroughly screened for suitability, and optimal surgical techniques were not developed.<ref name="pmid15466754">{{cite journal |vauthors=Swienckowski JJ, Pennington DW |title=Unicompartmental knee arthroplasty in patients sixty years of age or younger |journal=J Bone Joint Surg Am |volume=86-A Suppl 1 |issue=Pt 2 |pages=131–42 |date=September 2004 |pmid=15466754 |doi= |url=http://www.ejbjs.org/cgi/pmidlookup?view=long&pmid=15466754}}</ref> Advancements have been made to improve the design of the implants.<ref name=wu/><ref name="pmid15466754"/><ref>{{cite journal |author=Fitzsimmons SE, Vazquez EA, [[Michael J. Bronson|Bronson MJ]] |title=How to Treat the Stiff Total Knee Arthroplasty?: A Systematic Review |journal=Clin. Orthop. Relat. Res. |volume=468 |issue=4 |pages=1096–106 |date=April 2010 |pmid=20087698 |doi=10.1007/s11999-010-1230-y |url= |pmc=2835585}}</ref> Also, choosing the best-suited people was emphasized to ensure that surgeons followed the indications and contraindications for partial replacement. Proper selection,<ref name="pmid18300665">{{cite journal |vauthors=Geller JA, Yoon RS, Macaulay W |title=Unicompartmental knee arthroplasty: a controversial history and a rationale for contemporary resurgence |journal=J Knee Surg |volume=21 |issue=1 |pages=7–14 |date=January 2008 |pmid=18300665 |doi= |url=}}</ref> following the indications/contraindications, and performing the surgery well are key factors for the success of UKA.<ref name=wu/><ref name="pmid18180388"/> |
||
==Indications and contraindications== |
==Indications and contraindications== |
||
UKA may be suitable for |
UKA may be suitable for people with moderate joint disease caused by painful [[osteoarthritis]] or traumatic injury, a history of unsuccessful surgical procedures or poor [[bone]] density that precludes other types of [[knee]] surgery.<ref name=wu/> People who may not be eligible for a UKA include those with an active or suspected infection in or about the knee joint, may have a known sensitivity to device materials, have bone infections or disease that result in an inability to support or fixate the new implant to the bone, have inflammatory arthritis, have major deformities that can affect the knee mechanical axis, have neuromuscular disorders that may compromise motor control and/or stability, have any mental neuromuscular disorder, are obese,<ref name="pmid16164956">{{cite journal |author=Bert JM |title=Unicompartmental knee replacement |journal=Orthop. Clin. North Am. |volume=36 |issue=4 |pages=513–22 |date=October 2005 |pmid=16164956 |doi=10.1016/j.ocl.2005.05.001 |url=}}</ref> have lost a severe amount of bone from the shin ([[tibia]]) or have severe tibial deformities, have recurring [[subluxation]] of the knee joint, have untreated damage to the knee cap and thigh bone joint (patellofemoral joint), have untreated damage to the opposite compartment or the same side of the knee not being replaced by a device, and/or have instability of the knee ligaments such that the postoperative stability the UKA would be compromised.<ref name=wu/> |
||
The [[anterior cruciate ligament]] (ACL) should be intact,<ref>{{cite web|title=Partial Knee Replacement|url=http://www.dartmouth-hitchcock.org/ortho/partial_knee_replacement.html|date=2017|publisher=Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA}}</ref> although this is debated by clinicians for |
The [[anterior cruciate ligament]] (ACL) should be intact,<ref>{{cite web|title=Partial Knee Replacement|url=http://www.dartmouth-hitchcock.org/ortho/partial_knee_replacement.html|date=2017|publisher=Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA}}</ref> although this is debated by clinicians for people who need a medial compartment replacement.<ref name="pmid18180388"/> For people needing a lateral compartment replacement, the ACL should be intact and is contraindicated for people with ACL-deficient knees because the lateral component has more motion than the medial compartment.<ref name="pmid18180388"/> |
||
==History and physical examination== |
==History and physical examination== |
||
A physical examination and getting the |
A physical examination and getting the subject’s history is performed before getting surgery.<ref name="pmid18180388"/> A person with pain in one area of the knee may be a candidate for UKA.<ref name="pmid18180388"/> However, a person with pain in multiple areas of the knee may not be a good candidate for UKA.<ref name="pmid18180388"/> The doctor may take some radiographs (e.g., x-rays) to check for degeneration of the other knee compartments and evaluate the knee.<ref name="pmid18180388"/> The physical exam may also include special tests designed to test the ligaments of the knee and other anatomical structures.<ref name="pmid18300665"/> Most likely, the surgeon will decide to do a UKA during surgery where he/she can directly see the status of the other compartments.<ref name="pmid18180388"/> |
||
==Surgical information== |
==Surgical information== |
||
The surgeon may choose which type of incision and implant to use for the |
The surgeon may choose which type of incision and implant to use for the subject’s knee. During the surgery, the surgeon may align the instruments to determine the amount of bone to remove.<ref name="pmid15466754"/> The surgeon removes bone from the ([[tibia]]) and thigh bone ([[femur]]).<ref name=wu/><ref name="pmid15466754"/> The surgeon may decide to check if the appropriate amount of bone was removed during the surgery.<ref name="pmid15466754"/> In order to make sure that the proper size implant is used, a surgeon may choose to use a temporary trial. After making sure the proper size implant is selected, the surgeon will put the implant on the ends of the bone and secure it with pegs. Finally, the surgeon will close the wound with sutures.<ref name="pmid15466754"/><ref>{{cite web|title=Partial Knee Replacement|url=http://tony-gibbon.co.uk/treatment/knee-treatment/treatments/partial-knee-replacement|publisher=North Yorkshire Orthopaedic Specialists|accessdate=5 February 2013}}</ref> |
||
[[File:pkrvstotalknee.jpg]] <ref>http://www.aboutstryker.com/knee/procedures/knee-resurfacing.php</ref> |
|||
The |
The unicompartmental replacement is a minimally invasive option for people whose arthritis is isolated to either the medial or the lateral compartment. The procedure offers several benefits for patients with a moderately active lifestyle, who have arthritis in just one knee compartment, and who are within normal weight ranges. The surgeon uses an incision of just 3-4 inches; a total knee replacement typically requires an incision of 8-12 inches. The partial replacement does not disrupt the knee cap, which makes for a shorter rehabilitation period. A partial replacement also causes minimal blood loss during the procedure, and results in considerably less post-operative pain. The hospitalization time compared with a total knee replacement is also greatly reduced.<ref name=wu/><ref name=siman/><ref name=han/> |
||
==Benefits== |
==Benefits== |
||
The potential benefits of UKA include a smaller incision because the UKA implants are smaller than the total knee replacements, and the surgeon may make a smaller incision.<ref name="pmid18180388"/> This may lead to a smaller scar.<ref name="pmid18180388"/> Another potential benefit is less post-operative [[pain]] because less bone is removed. Also, a quicker operation and shorter recovery period may be a result of less bone being removed during the operation and the soft tissue may sustain less trauma.<ref>{{cite journal |vauthors=Mullaji AB, Sharma A, Marawar S |title=Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique |journal=J Arthroplasty |volume=22 |issue=4 Suppl 1 |pages=7–11 |date=June 2007 |pmid=17570269 |doi=10.1016/j.arth.2006.12.109 |url=}}</ref> Also, the rehabilitation process may be more progressive.<ref>{{cite journal |author=Newman JH |title=Unicompartmental knee replacement |journal=Knee |volume=7 |issue=2 |pages=63–70 |date=April 2000 |pmid=10788767 |doi=10.1016/S0968-0160(99)00032-0 |url=}}</ref> More specific benefits of UKA are it may improve range of motion, reduce blood loss during surgery, reduce the |
The potential benefits of UKA include a smaller incision because the UKA implants are smaller than the total knee replacements, and the surgeon may make a smaller incision.<ref name="pmid18180388"/> This may lead to a smaller scar.<ref name="pmid18180388"/> Another potential benefit is less post-operative [[pain]] because less bone is removed.<ref name=wu/> Also, a quicker operation and shorter recovery period may be a result of less bone being removed during the operation and the soft tissue may sustain less trauma.<ref name=wu/><ref>{{cite journal |vauthors=Mullaji AB, Sharma A, Marawar S |title=Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique |journal=J Arthroplasty |volume=22 |issue=4 Suppl 1 |pages=7–11 |date=June 2007 |pmid=17570269 |doi=10.1016/j.arth.2006.12.109 |url=}}</ref> Also, the rehabilitation process may be more progressive.<ref>{{cite journal |author=Newman JH |title=Unicompartmental knee replacement |journal=Knee |volume=7 |issue=2 |pages=63–70 |date=April 2000 |pmid=10788767 |doi=10.1016/S0968-0160(99)00032-0 |url=}}</ref> More specific benefits of UKA are that it may improve range of motion, reduce blood loss during surgery, reduce the person’s time spent in the hospital, and decrease costs.<ref name=wu/><ref name="pmid16164956"/> |
||
In 2018, two of the most significant benefits of UKA or partial knee replacements are: |
|||
1. Partial knee replacement |
1. Partial knee replacement subjects report that their replaced knee feels more like their original non-replaced knee as compared to a total knee replacement |
||
2, Partial knee replacements leave other options open to further advances. By not replacing the rest of the knee with metal and plastic, if other options exist in years to come for arthritis in these areas then a partial knee replacement does not burn that bridge. |
2, Partial knee replacements leave other options open to further advances. By not replacing the rest of the knee with metal and plastic, if other options exist in years to come for arthritis in these areas then a partial knee replacement does not burn that bridge. |
||
==Risks== |
==Risks== |
||
[[Blood clots]] (also known as deep vein thrombosis) are a common complication after surgery.<ref name="pmid17948162">{{cite journal |author=Colwell CW |title=Rationale for thromboprophylaxis in lower joint arthroplasty |journal=Am J. Orthop. |volume=36 |issue=9 Suppl |pages=11–3 |date=September 2007 |pmid=17948162 |doi= |url=}}</ref><ref name="pmid17613508">{{cite journal |author=Warwick D |title=Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry |journal=J Bone Joint Surg Br |volume=89 |issue=6 |pages=799–807 |date=June 2007 |pmid=17613508 |doi=10.1302/0301-620X.89B6.18844 |url= |name-list-format=vanc|author2=Friedman RJ |author3=Agnelli G |display-authors=3 |last4=Gil-Garay |first4=E. |last5=Johnson |first5=K. |last6=Fitzgerald |first6=G. |last7=Turibio |first7=F. M.}}</ref> However, a doctor may prescribe certain medications to help prevent blood clots.<ref name="pmid17948162"/><ref name="pmid17613508"/> Infection may occur after surgery.<ref>{{cite journal |vauthors=Ritter MA, Olberding EM, Malinzak RA |title=Ultraviolet lighting during orthopaedic surgery and the rate of infection |journal=J Bone Joint Surg Am |volume=89 |issue=9 |pages=1935–40 |date=September 2007 |pmid=17768189 |doi=10.2106/JBJS.F.01037 |url=}}</ref> However, antibiotics may be prescribed by a doctor to help prevent infections.<ref name="pmid17613508"/> Individual |
[[Blood clots]] (also known as [[deep vein thrombosis]]) are a common complication after surgery.<ref name="pmid17948162">{{cite journal |author=Colwell CW |title=Rationale for thromboprophylaxis in lower joint arthroplasty |journal=Am J. Orthop. |volume=36 |issue=9 Suppl |pages=11–3 |date=September 2007 |pmid=17948162 |doi= |url=}}</ref><ref name="pmid17613508">{{cite journal |author=Warwick D |title=Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry |journal=J Bone Joint Surg Br |volume=89 |issue=6 |pages=799–807 |date=June 2007 |pmid=17613508 |doi=10.1302/0301-620X.89B6.18844 |url= |name-list-format=vanc|author2=Friedman RJ |author3=Agnelli G |display-authors=3 |last4=Gil-Garay |first4=E. |last5=Johnson |first5=K. |last6=Fitzgerald |first6=G. |last7=Turibio |first7=F. M.}}</ref> However, a doctor may prescribe certain medications to help prevent blood clots.<ref name="pmid17948162"/><ref name="pmid17613508"/> Infection may occur after surgery.<ref>{{cite journal |vauthors=Ritter MA, Olberding EM, Malinzak RA |title=Ultraviolet lighting during orthopaedic surgery and the rate of infection |journal=J Bone Joint Surg Am |volume=89 |issue=9 |pages=1935–40 |date=September 2007 |pmid=17768189 |doi=10.2106/JBJS.F.01037 |url=}}</ref> However, antibiotics may be prescribed by a doctor to help prevent infections.<ref name="pmid17613508"/> Individual factors (e.g., anatomy, weight, prior medical history, prior joint surgeries) should be addressed with the surgery subject. The causes of long-term failure of UKAs include [[polyethylene]] wear, loosening of the implant, and degeneration of the adjacent knee compartment.<ref name="pmid18180388"/> |
||
==Long-term results== |
==Long-term results== |
||
Long |
Long term studies reported excellent outcomes for UKA, partly due to subject screening,<ref name="pmid15866962">{{cite journal |author=Berger RA |title=Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up |journal=J Bone Joint Surg Am |volume=87 |issue=5 |pages=999–1006 |date=May 2005 |pmid=15866962 |doi=10.2106/JBJS.C.00568 |url= |name-list-format=vanc|author2=Meneghini RM |author3=Jacobs JJ |display-authors=3 |last4=Sheinkop |first4=MB |last5=Della Valle |first5=CJ |last6=Rosenberg |first6=AG |last7=Galante |first7=JO}}</ref> minimizing the amount of bone that is removed,<ref name="pmid15930935">{{cite journal |vauthors=Price AJ, Waite JC, Svard U |title=Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty |journal=Clin. Orthop. Relat. Res. |volume= &na;|issue=435 |pages=171–80 |date=June 2005 |pmid=15930935 |doi= 10.1097/00003086-200506000-00024|url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?an=00003086-200506000-00024}}</ref> and using the proper surgical technique.<ref name="pmid15866962"/> One study found that at a minimum of 10 years follow up time after the initial surgery, the overall survival rate of the implant was 96%.<ref name="pmid15866962"/> Also, 92% of the people in this study had excellent or good outcome.<ref name="pmid15866962"/> Another study, reported that at 15 years follow up time after the initial surgery, the overall rate of the implant was 93% and 91% of these people reported good or excellent outcomes.<ref name="pmid15930935"/> |
||
==References== |
==References== |
||
{{Reflist| |
{{Reflist|30em}} |
||
==External links== |
==External links== |
||
Revision as of 18:53, 3 August 2018
| Unicompartmental knee arthroplasty | |
|---|---|
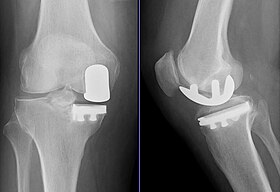 Radiographs of a knee arthroplasty of the medial compartment | |
| ICD-9-CM | 81.54 |
Unicompartmental knee arthroplasty (UKA) is a surgical procedure used to relieve arthritis in one of the knee compartments in which the damaged parts of the knee are replaced. UKA surgery may reduce post-operative pain and have a shorter recovery period than a total knee replacement procedure,[1][2] particularly in people over 75 years of age.[3] Moreover, UKAs may require a smaller incision, less tissue damage, and faster recovery times.[2]
In the United States, the procedure constitutes approximately 8% of knee arthroplasties.[4] In comparisons with a more extensive surgical procedure called high tibial osteotomy, UKA has equal or better outcomes.[1][5]
Background
In the early 1950s, Duncan C. McKeever theorized that osteoarthritis could be isolated to only one compartment of the knee joint,[2] and that replacement of the entire knee might not be necessary if only one knee compartment were affected.[2][6] The UKA concept was designed to cause less trauma or damage than traditional total knee replacement by removing less bone and trying to maintain most of the person’s bone and anatomy.[2] The concept was also designed to use smaller implants and thereby keep most of the person’s bone, helping them return to normal function faster.[3][2]
Initially, UKAs were not always successful, because the implants were poorly designed, people needing the surgery were not thoroughly screened for suitability, and optimal surgical techniques were not developed.[7] Advancements have been made to improve the design of the implants.[1][7][8] Also, choosing the best-suited people was emphasized to ensure that surgeons followed the indications and contraindications for partial replacement. Proper selection,[9] following the indications/contraindications, and performing the surgery well are key factors for the success of UKA.[1][2]
Indications and contraindications
UKA may be suitable for people with moderate joint disease caused by painful osteoarthritis or traumatic injury, a history of unsuccessful surgical procedures or poor bone density that precludes other types of knee surgery.[1] People who may not be eligible for a UKA include those with an active or suspected infection in or about the knee joint, may have a known sensitivity to device materials, have bone infections or disease that result in an inability to support or fixate the new implant to the bone, have inflammatory arthritis, have major deformities that can affect the knee mechanical axis, have neuromuscular disorders that may compromise motor control and/or stability, have any mental neuromuscular disorder, are obese,[10] have lost a severe amount of bone from the shin (tibia) or have severe tibial deformities, have recurring subluxation of the knee joint, have untreated damage to the knee cap and thigh bone joint (patellofemoral joint), have untreated damage to the opposite compartment or the same side of the knee not being replaced by a device, and/or have instability of the knee ligaments such that the postoperative stability the UKA would be compromised.[1]
The anterior cruciate ligament (ACL) should be intact,[11] although this is debated by clinicians for people who need a medial compartment replacement.[2] For people needing a lateral compartment replacement, the ACL should be intact and is contraindicated for people with ACL-deficient knees because the lateral component has more motion than the medial compartment.[2]
History and physical examination
A physical examination and getting the subject’s history is performed before getting surgery.[2] A person with pain in one area of the knee may be a candidate for UKA.[2] However, a person with pain in multiple areas of the knee may not be a good candidate for UKA.[2] The doctor may take some radiographs (e.g., x-rays) to check for degeneration of the other knee compartments and evaluate the knee.[2] The physical exam may also include special tests designed to test the ligaments of the knee and other anatomical structures.[9] Most likely, the surgeon will decide to do a UKA during surgery where he/she can directly see the status of the other compartments.[2]
Surgical information
The surgeon may choose which type of incision and implant to use for the subject’s knee. During the surgery, the surgeon may align the instruments to determine the amount of bone to remove.[7] The surgeon removes bone from the (tibia) and thigh bone (femur).[1][7] The surgeon may decide to check if the appropriate amount of bone was removed during the surgery.[7] In order to make sure that the proper size implant is used, a surgeon may choose to use a temporary trial. After making sure the proper size implant is selected, the surgeon will put the implant on the ends of the bone and secure it with pegs. Finally, the surgeon will close the wound with sutures.[7][12]
The unicompartmental replacement is a minimally invasive option for people whose arthritis is isolated to either the medial or the lateral compartment. The procedure offers several benefits for patients with a moderately active lifestyle, who have arthritis in just one knee compartment, and who are within normal weight ranges. The surgeon uses an incision of just 3-4 inches; a total knee replacement typically requires an incision of 8-12 inches. The partial replacement does not disrupt the knee cap, which makes for a shorter rehabilitation period. A partial replacement also causes minimal blood loss during the procedure, and results in considerably less post-operative pain. The hospitalization time compared with a total knee replacement is also greatly reduced.[1][3][5]
Benefits
The potential benefits of UKA include a smaller incision because the UKA implants are smaller than the total knee replacements, and the surgeon may make a smaller incision.[2] This may lead to a smaller scar.[2] Another potential benefit is less post-operative pain because less bone is removed.[1] Also, a quicker operation and shorter recovery period may be a result of less bone being removed during the operation and the soft tissue may sustain less trauma.[1][13] Also, the rehabilitation process may be more progressive.[14] More specific benefits of UKA are that it may improve range of motion, reduce blood loss during surgery, reduce the person’s time spent in the hospital, and decrease costs.[1][10]
In 2018, two of the most significant benefits of UKA or partial knee replacements are: 1. Partial knee replacement subjects report that their replaced knee feels more like their original non-replaced knee as compared to a total knee replacement 2, Partial knee replacements leave other options open to further advances. By not replacing the rest of the knee with metal and plastic, if other options exist in years to come for arthritis in these areas then a partial knee replacement does not burn that bridge.
Risks
Blood clots (also known as deep vein thrombosis) are a common complication after surgery.[15][16] However, a doctor may prescribe certain medications to help prevent blood clots.[15][16] Infection may occur after surgery.[17] However, antibiotics may be prescribed by a doctor to help prevent infections.[16] Individual factors (e.g., anatomy, weight, prior medical history, prior joint surgeries) should be addressed with the surgery subject. The causes of long-term failure of UKAs include polyethylene wear, loosening of the implant, and degeneration of the adjacent knee compartment.[2]
Long-term results
Long term studies reported excellent outcomes for UKA, partly due to subject screening,[18] minimizing the amount of bone that is removed,[19] and using the proper surgical technique.[18] One study found that at a minimum of 10 years follow up time after the initial surgery, the overall survival rate of the implant was 96%.[18] Also, 92% of the people in this study had excellent or good outcome.[18] Another study, reported that at 15 years follow up time after the initial surgery, the overall rate of the implant was 93% and 91% of these people reported good or excellent outcomes.[19]
References
- ^ a b c d e f g h i j k Santoso, M. B; Wu, L (2017). "Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review". Journal of Orthopaedic Surgery and Research. 12 (1): 50. doi:10.1186/s13018-017-0552-9. PMC 5371236. PMID 28351371.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i j k l m n o p q Borus T, Thornhill T (January 2008). "Unicompartmental knee arthroplasty". J Am Acad Orthop Surg. 16 (1): 9–18. PMID 18180388.
- ^ a b c Siman, H; Kamath, A. F; Carrillo, N; Harmsen, W. S; Pagnano, M. W; Sierra, R. J (2017). "Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates". The Journal of Arthroplasty. 32 (6): 1792–1797. doi:10.1016/j.arth.2017.01.020. PMID 28215968.
- ^ Riddle DL, Jiranek WA, McGlynn FJ (April 2008). "Yearly incidence of unicompartmental knee arthroplasty in the United States". J Arthroplasty. 23 (3): 408–12. doi:10.1016/j.arth.2007.04.012. PMID 18358380.
- ^ a b Han, S. B; Kyung, H. S; Seo, I. W; Shin, Y. S (2017). "Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy". Medicine. 96 (50): e9268. doi:10.1097/MD.0000000000009268. PMC 5815788. PMID 29390376.
- ^ Gibbon, Tony. "Partial Knee Replacement". North Yorkshire Orthopaedic Specialists. Retrieved 1 February 2013.
- ^ a b c d e f Swienckowski JJ, Pennington DW (September 2004). "Unicompartmental knee arthroplasty in patients sixty years of age or younger". J Bone Joint Surg Am. 86-A Suppl 1 (Pt 2): 131–42. PMID 15466754.
- ^ Fitzsimmons SE, Vazquez EA, Bronson MJ (April 2010). "How to Treat the Stiff Total Knee Arthroplasty?: A Systematic Review". Clin. Orthop. Relat. Res. 468 (4): 1096–106. doi:10.1007/s11999-010-1230-y. PMC 2835585. PMID 20087698.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Geller JA, Yoon RS, Macaulay W (January 2008). "Unicompartmental knee arthroplasty: a controversial history and a rationale for contemporary resurgence". J Knee Surg. 21 (1): 7–14. PMID 18300665.
- ^ a b Bert JM (October 2005). "Unicompartmental knee replacement". Orthop. Clin. North Am. 36 (4): 513–22. doi:10.1016/j.ocl.2005.05.001. PMID 16164956.
- ^ "Partial Knee Replacement". Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA. 2017.
- ^ "Partial Knee Replacement". North Yorkshire Orthopaedic Specialists. Retrieved 5 February 2013.
- ^ Mullaji AB, Sharma A, Marawar S (June 2007). "Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique". J Arthroplasty. 22 (4 Suppl 1): 7–11. doi:10.1016/j.arth.2006.12.109. PMID 17570269.
- ^ Newman JH (April 2000). "Unicompartmental knee replacement". Knee. 7 (2): 63–70. doi:10.1016/S0968-0160(99)00032-0. PMID 10788767.
- ^ a b Colwell CW (September 2007). "Rationale for thromboprophylaxis in lower joint arthroplasty". Am J. Orthop. 36 (9 Suppl): 11–3. PMID 17948162.
- ^ a b c Warwick D; Friedman RJ; Agnelli G; et al. (June 2007). "Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry". J Bone Joint Surg Br. 89 (6): 799–807. doi:10.1302/0301-620X.89B6.18844. PMID 17613508.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Ritter MA, Olberding EM, Malinzak RA (September 2007). "Ultraviolet lighting during orthopaedic surgery and the rate of infection". J Bone Joint Surg Am. 89 (9): 1935–40. doi:10.2106/JBJS.F.01037. PMID 17768189.
- ^ a b c d Berger RA; Meneghini RM; Jacobs JJ; et al. (May 2005). "Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up". J Bone Joint Surg Am. 87 (5): 999–1006. doi:10.2106/JBJS.C.00568. PMID 15866962.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Price AJ, Waite JC, Svard U (June 2005). "Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty". Clin. Orthop. Relat. Res. &na, (435): 171–80. doi:10.1097/00003086-200506000-00024. PMID 15930935.
{{cite journal}}: CS1 maint: extra punctuation (link)
External links
- University of Washington’s Orthopaedics and Sports Medicine, School of Medicine
- About.com
- Knee Society [1]
- American Academy of Orthopaedic Surgeon's Your Orthopaedic Connection [2]
- Medline Plus [3]
- [4]
- About Partial Knee Replacements [5]
- Partial Knee Replacement : Stryker Orthopaedics
