Sleep deprivation: Difference between revisions
No edit summary |
|||
| Line 10: | Line 10: | ||
Generally, lack of sleep may result in:<ref name="SleepDep">{{cite journal |title=http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Sleep_deprivation?OpenDocument}}</ref><ref name="SleepDep2">{{cite journal |title=http://www.apa.org/ed/topss/bryanread.html}}</ref> |
Generally, lack of sleep may result in:<ref name="SleepDep">{{cite journal |title=http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Sleep_deprivation?OpenDocument}}</ref><ref name="SleepDep2">{{cite journal |title=http://www.apa.org/ed/topss/bryanread.html}}</ref> |
||
* aching muscles<ref>{{cite book |last=Morin |first=Charles M. |title=Insomnia |page=28 |isbn=0306477505 |year=2003 |publisher=Kluwer Academic/Plenum Publ. |location=New York}}</ref> |
* aching muscles<ref>{{cite book |last=Morin |first=Charles M. |title=Insomnia |page=28 |isbn=0306477505 |year=2003 |publisher=Kluwer Academic/Plenum Publ. |location=New York}}</ref> |
||
* Massive Boner |
|||
* dizziness and nausea |
* dizziness and nausea |
||
* dry mouth{{Citation needed|date=October 2009}} |
* dry mouth{{Citation needed|date=October 2009}} |
||
Revision as of 06:19, 27 September 2010
The examples and perspective in this article may not represent a worldwide view of the subject. (July 2010) |
Sleep deprivation is characterized by having too little sleep; it can be either chronic or acute. Long-term sleep deprivation causes death in lab animals.[1] A chronic sleep-restricted state can cause fatigue, daytime sleepiness, clumsiness and weight loss or weight gain.[2]
Complete absence of sleep over long periods is impossible for humans to achieve (unless they suffer from fatal familial insomnia); brief microsleeps cannot be avoided.[3]
Physiological effects
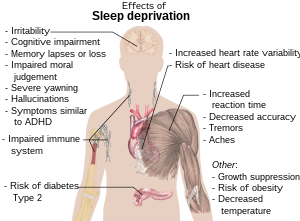

Generally, lack of sleep may result in:[5][6]
- aching muscles[7]
- Massive Boner
- dizziness and nausea
- dry mouth[citation needed]
- hallucinations[8]
- hand tremors[9]
- headaches
- increased blood pressure[10]
- increased risk of diabetes[11]
- increased risk of fibromyalgia[12]
- irritability[5]
- memory lapses or loss[13]
- nystagmus (rapid involuntary rhythmic eye movement)[14]
- obesity[11]
- slowed word recall[citation needed]
- temper tantrums in children[5]
- yawning[5]
- symptoms similar to:
Diabetes
In 2005, a study of over 1400 participants showed that participants who habitually slept few hours were more likely to have associations with Diabetes Type 2.[16] However, because this study was merely correlational, the direction of cause and effect between little sleep and diabetes is uncertain. The authors point to an earlier study which showed that experimental rather than habitual restriction of sleep resulted in impaired glucose tolerance (IGT).[17]
Effects on the brain
This section needs additional citations for verification. (September 2009) |
Sleep deprivation can adversely affect the brain and cognitive function.[18] A 2000 study, by the UCSD School of Medicine and the Veterans Affairs Healthcare System in San Diego, used functional magnetic resonance imaging technology to monitor activity in the brains of sleep-deprived subjects performing simple verbal learning tasks.[19] The study showed that regions of the brain's prefrontal cortex displayed more activity in sleepier subjects. Depending on the task at hand, the brain would sometimes attempt to compensate for the adverse effects caused by lack of sleep.
The temporal lobe, which is a brain region involved in language processing, was activated during verbal learning in rested subjects but not in sleep deprived subjects. The parietal lobe, not activated in rested subjects during the verbal exercise, was more active when the subjects were deprived of sleep. Although memory performance was less efficient with sleep deprivation, greater activity in the parietal region was associated with better memory.
A 2001 study at Chicago Medical Institute suggested that sleep deprivation may be linked to serious diseases, such as heart disease and mental illnesses including psychosis and bipolar disorder.[20] The link between sleep deprivation and psychosis was further documented in 2007 through a study at Harvard Medical School and the University of California at Berkeley. The study revealed, using MRI scans, that lack of sleep causes the brain to become incapable of putting an emotional event into the proper perspective and incapable of making a controlled, suitable response to the event.
A noted 2002 University of California animal study indicated that non-rapid eye movement sleep is necessary for turning off neurotransmitters and allowing their receptors to "rest" and regain sensitivity which allows monoamines (norepinephrine, serotonin and histamine) to be effective at naturally produced levels. This leads to improved regulation of mood and increased learning ability. The study also found that REM sleep deprivation may alleviate clinical depression because it mimics selective serotonin reuptake inhibitors (SSRIs). This is because the natural decrease in monoamines during REM is not allowed to occur, which causes the concentration of neurotransmitters in the brain, that are depleted in clinically depressed persons, to increase. Sleep outside of the REM phase may allow enzymes to repair brain cell damage caused by free radicals. High metabolic activity while awake damages the enzymes themselves preventing efficient repair. This study observed the first evidence of brain damage in rats as a direct result of sleep deprivation.[21]
Animal studies suggest that sleep deprivation increases stress hormones, which may reduce new cell production in adult brains.[22]
Effects on growth
A 1999 study[23] found that sleep deprivation resulted in reduced cortisol secretion the next day, driven by increased subsequent slow-wave sleep. Sleep deprivation was found to enhance activity on the hypothalamic-pituitary-adrenal axis (which controls reactions to stress and regulates body functions such as digestion, the immune system, mood, sex, or energy usage) while suppressing growth hormones. The results supported previous studies, which observed adrenal insufficiency in idiopathic hypersomnia.
Effects on the healing process
A study conducted in 2005 showed that a group of rats which were deprived of REM (Rapid Eye Movement) sleep for five days had no significant effect on their ability to heal wounds, compared to a group of rats not deprived of "dream" sleep.[24] The rats were allowed deep (NREM) sleep. However, another study conducted by Gumustekin et al.[25] in 2004 showed sleep deprivation hindering the healing of burns on rats.
Attention
Among the numerous physical consequences of sleep deprivation, attention deficits are perhaps the most important; attentional lapses in mundane routines can lead to unfortunate results, from forgetting ingredients while cooking to missing a sentence while taking notes. The attentional lapses also extend into more critical domains in which the consequences can be literally life-or-death; traffic accidents and industrial disasters can result from inattentiveness attributable to sleep deprivation.
To empirically measure the magnitude of these attention deficits, researchers typically employ the psychomotor vigilance task (PVT) which requires the subject to press a button in response to a light at pseudo-random intervals. Failure to press the button in response to the stimulus (light) is recorded as an error, attributable to the microsleeps that occur as a product of sleep deprivation.
Crucially, individuals' subjective evaluations of their fatigue often do not predict actual performance on the PVT. While totally sleep-deprived individuals are usually aware of the degree of their impairment, lapses from chronic (lesser) sleep deprivation can build up over time so that they are equal in number and severity to the lapses occurring from total (acute) sleep deprivation. Chronically sleep-deprived people, however, continue to rate themselves considerably less impaired than totally sleep-deprived participants.[26] Since people usually evaluate their capability on tasks like driving subjectively, their evaluations may lead them to the false conclusion that they are able to perform tasks that require constant attention when their abilities are in fact impaired.
Impairment of ability
The dangers of sleep deprivation are apparent on the road; the American Academy of Sleep Medicine reports that one in every five serious motor vehicle injuries is related to driver fatigue, with 80,000 drivers falling asleep behind the wheel every day and 250,000 accidents every year related to sleep,[27] though the National Highway Traffic Safety Administration suggests the figure for traffic accidents may be closer to 100,000.[28] The AASM recommends pulling off the road and taking a 15- or 20-minute nap to alleviate drowsiness.[27]
According to a 2000 study published in the British Medical Journal, researchers in Australia and New Zealand reported that sleep deprivation can have some of the same hazardous effects as being drunk.[29] People who drove after being awake for 17–19 hours performed worse than those with a blood alcohol level of .05 percent, which is the legal limit for drunk driving in most western European countries and Australia. Another study suggested that performance begins to degrade after 16 hours awake, and 21 hours awake was equivalent to a blood alcohol content of .08 percent, which is the blood alcohol limit for drunk driving in Canada, the U.S., and the U.K.[30]
In addition, as a result of continuous muscular activity without proper rest time, effects such as cramping are much more frequent in sleep-deprived individuals. Extreme cases of sleep deprivation have been reported to be associated with hernias, muscle fascia tears, and other such problems commonly associated with physical overexertion. Beyond impaired motor skills, people who get too little sleep may have higher levels of stress, anxiety and depression, and may take unnecessary risks.[citation needed]
A 2006 study has shown that while total sleep deprivation for one night caused many errors, the errors were not significant until after the second night of total sleep deprivation.[31] However, combining alcohol with acute sleep deprivation results in a trebled rate of driving off the road when using a simulator.[32]
The National Sleep Foundation identifies several warning signs that a driver is dangerously fatigued, including rolling down the window, turning up the radio, trouble keeping eyes open, head-nodding, drifting out of the lane, and daydreaming. At particular risk are lone drivers between midnight and 6 a.m.[33]
Sleep deprivation can negatively impact performance in professional fields as well, potentially jeopardizing lives. Due largely to the February 2009 crash of a regional jet in Buffalo, NY, which killed 50 people and was partially attributed to pilot fatigue, the FAA is reviewing its procedures to ensure pilots are sufficiently rested.[34] A 2004 study also found medical residents with less than four hours of sleep a night made more than twice as many errors as residents who slept for more than seven hours a night, an especially alarming trend given that less than 11% of surveyed residents were sleeping more than seven hours a night.[35]
Great sleep deprivation mimics psychosis: distorted perceptions can lead to inappropriate emotional and behavioral responses.[36]
Microsleeps
Microsleeps occur when a person has a significant sleep deprivation. The brain automatically shuts down, falling into a sleep state for a period that can last from a second to half a minute. The person falls asleep no matter what activity he or she is engaged in. Microsleeps are similar to blackouts and a person experiencing them is not consciously aware that they are occurring.
Weight gain/loss
In rats, prolonged, complete sleep deprivation increases both food intake and energy expenditure, however a hormone imbalance is observed, leading to weight gain and ultimately death.[2]
Several large studies using nationally representative samples suggest that the obesity problem in the United States might have as one of its causes a corresponding decrease in the average number of hours that people are sleeping.[37][38][39] The findings suggest that this might be happening because sleep deprivation could be disrupting hormones that regulate glucose metabolism and appetite.[40]
The association between sleep deprivation and obesity appears to be strongest in young and middle-age adults. Other scientists hold that the physical discomfort of obesity and related problems, such as sleep apnea, reduce an individual's chances of getting a good night's sleep.
Uses
Scientific study of laboratory animals
In science, sleep deprivation (of rodents, e.g.) is used in order to study the function(s) of sleep and the biological mechanisms underlying the effects of sleep deprivation. Sleep deprivation can result in psychological symptoms resembling those of psychosis if sleep is withheld for more than 5 days.[citation needed]
Some sleep deprivation techniques are as follows:
- Gentle handling (often requires polysomnography): during the sleep deprivation period, the animal and its polygraph record are continuously observed; when the animal displays sleep electrophysiological signals or assumes a sleep posture, it is given objects to play with and activated by acoustic and if necessary tactile stimuli.[41] Although subjective,[42] this technique is used for total sleep deprivation as well as REM or NREM sleep deprivation.

- Single platform: probably one of the first scientific methods (see Jouvet, 1964[43] for cats[44] and for rodents). During the sleep deprivation period, the animal is placed on an inverted flower pot whose bottom diameter is small relative to the animal size (usually 7 cm for adult rats); the pot is placed in a large tub filled with water to within 1 cm of the flower pot bottom. The animal is able to rest on the pot and is even able to get NREM sleep. But at the onset of REM sleep, with its ensuing muscular relaxation, it would either fall into the water and clamber back to its pot or would get its nose wet enough to waken it. So this technique is used only for REM sleep deprivation.
- Multiple platform: in order to reduce the elevated stress response induced by the single platform method,[45] developed this technique in which the animal is placed into a large tank containing multiple platforms, thus eliminating the movement restriction experienced in the single platform. This technique is also used only for REM sleep deprivation.
- Modified multiple platform: modification of the multiple platform method where several animals together get the sleep deprivation (Nunes and Tufik, 1994).
- Pendulum: animals are prevented from entering into PS by allowing them to sleep for only brief periods of time. This is accomplished by an apparatus which moves the animals' cages backwards and forwards like a pendulum. At the extremes of the motion postural imbalance is produced in the animals forcing them to walk downwards to the other side of their cages.[46]
Interrogation
Sleep deprivation can be used as a means of interrogation, which has resulted in court trials over whether or not the technique is a form of torture.[47]
Under one interrogation technique, a subject might be kept awake for several days and when finally allowed to fall asleep, suddenly awakened and questioned. Menachem Begin, the Prime Minister of Israel from 1977–83, described his experience of sleep deprivation when a prisoner of the NKVD in Russia as follows:
In the head of the interrogated prisoner, a haze begins to form. His spirit is wearied to death, his legs are unsteady, and he has one sole desire: to sleep... Anyone who has experienced this desire knows that not even hunger and thirst are comparable with it.[48]
Sleep deprivation was one of the five techniques used by the British government in the 1970s. The European Court of Human Rights ruled that the five techniques "did not occasion suffering of the particular intensity and cruelty implied by the word torture ... [but] amounted to a practice of inhuman and degrading treatment", in breach of the European Convention on Human Rights.[49]
The question of extreme use of sleep deprivation as torture has advocates on both sides of the issue. In 2006, Australian Federal Attorney-General Philip Ruddock argued that sleep deprivation does not constitute torture.[50] Nicole Bieske, a spokeswoman for Amnesty International Australia, has stated, "At the very least, sleep deprivation is cruel, inhumane and degrading. If used for prolonged periods of time it is torture."[51]
Treatment for depression
Recent studies show sleep deprivation has some potential in the treatment of depression, About 60% of patients, when sleep-deprived, show immediate recovery, with most relapsing the following night. The effect has been shown to link to increases in brain-derived neurotrophic factor (BDNF).[52] It has been shown that chronotype is related to the effect of sleep deprivation on mood in normal people; those with morningness circadian preference show an increase in depression-dejection scores while those with eveningness preference show a significant decrease.[53]
The incidence of relapse can be decreased by combining sleep deprivation with medication.[54] Many tricyclic antidepressants happen to suppress REM sleep, providing additional evidence for a link between mood and sleep.[55] Similarly, tranylcypromine has been shown to completely suppress REM sleep at adequate doses.
Voluntary
Sleep deprivation has sometimes been self-imposed to achieve personal notoriety in the context of record-breaking stunts.
Causes
Psychostimulant drugs
Psychostimulant drugs, predominantly methamphetamine,[56] are capable of keeping users awake for 3–15 days at a time with repeated dosing, a.k.a. "binging".[57]
Mental illness
The specific causal relationships between sleep loss and effects on psychiatric disorders have been most extensively studied in patients with mood disorders. Shifts into mania in bipolar patients are often preceded by periods of insomnia, and sleep deprivation has been shown to induce a manic state in susceptible individuals. Sleep deprivation may represent a final common pathway in the genesis of mania, and sleep loss is both a precipitating and reinforcing factor for the manic state.[58]
School
A National Sleep Foundation survey found that college/university-aged students get an average of 6.8 hours of sleep each night.[59] Sleep deprivation is common in college freshmen as they adjust to the stress and social activities of college life. A study performed by the Department of Psychology at the National Chung Cheng University in Taiwan concluded that freshmen received the shortest amount of sleep during the week.[60] In 1997 the University of Minnesota did research that compared students who went to school at 7:15 a.m. and those who went to school at 8:40 a.m. They found that students who went to school at 8:40 got higher grades and more sleep on weekday nights.[28] One in four U.S. high school students admits to falling asleep in class at least once a week.[61] It is known that during human adolescence, circadian rhythms and therefore sleep patterns typically undergo marked changes. Electroencephalogram (EEG) studies indicate a 50% reduction of deep (stage 4) sleep and a 75% reduction in the peak amplitude of delta waves during nonrapid-eye movement sleep in adolescence. School schedules are often incompatible with a corresponding delay in sleep offset, leading to a less than optimal amount of sleep for the majority of adolescents.[62]
Counteracting the effects of sleep deprivation
Several strategies are common in attempting to increase alertness and counteract the effects of sleep deprivation. Caffeine is often used over short periods to boost wakefulness when acute sleep deprivation is experienced; however, caffeine is less effective if taken routinely. Other strategies recommended by the American Academy of Sleep Medicine include prophylactic sleep before deprivation, naps, other stimulants, and combinations thereof. However, the only sure and safe way to combat sleep deprivation is to increase nightly sleep time.[63]
Longest period without sleep
Randy Gardner holds the scientifically documented record for the longest period of time a human being has intentionally gone without sleep not using stimulants of any kind. Gardner stayed awake for 264 hours (eleven days), breaking the previous record of 260 hours held by Tom Rounds of Honolulu.[64] Lt. Cmdr. John J. Ross of the U.S. Navy Medical Neuropsychiatric Research Unit later published an account of this event, which became well known among sleep-deprivation researchers.[citation needed]
Other sources claim that the Guinness World Records record stands at 449 hours (18 days, 17 hours), held by Maureen Weston, of Peterborough, Cambridgeshire in April, 1977, in a rocking-chair marathon.[65]
Claims of not having slept in years have been made at times, for certain individuals, but either without scientific verification, or contradicted in independent verification:
- Never scientifically verified: Thai Ngoc, born 1942, claimed in 2006 to have been awake for 33 years or 11,700 nights, according to Vietnamese news organization Thanh Nien. It was said that Ngoc acquired the ability to go without sleep after a bout of fever in 1973,[66] but other reports indicate he stopped sleeping in 1976 with no known trigger.[67] At the time of the Thanh Nien report, Ngoc suffered from no apparent ill effect (other than a minor decline in liver function), was mentally sound and could carry 100 kg of pig feed down a 4 km road,[66] but another report indicates that he was healthy before the sleepless episode but that now he was not feeling well because of the lack of sleep.[67]
- Contradicted by claimant himself: In January 2005, the RIA Novosti published an article about Fyodor Nesterchuk from the Ukrainian town of Kamen-Kashirsky who claimed to have not slept in more than 20 years. Local doctor Fyodor Koshel, chief of the Lutsk city health department, claimed to have examined him extensively and failed to make him sleep. Koshel also said however that Nesterchuck did not suffer any of the normally deleterious effects of sleep deprivation.[68] However, when a reporter from The Guardian followed up on this report, Nesterchuk said he was getting 2–3 hours of sleep per night, and that "[h]e did not appear to notice the marked difference between never getting to sleep once in 240 months, and getting fewer than the recommended number of hours each week."[69]
- Contradicted in more accurate reporting: Rhett Lamb[70] of St. Petersburg, Florida, was initially reported to not sleep at all, but actually has a rare condition permitting him to sleep only one to two hours per day in the first three years of his life. He has a rare abnormality called an Arnold-Chiari malformation where brain tissue protrudes into the spinal canal; the skull puts pressure on the protruding part of the brain. The boy was operated on at All Children's Hospital in St. Petersburg in May 2008. Two days after surgery he slept through the night.[71][72]
- Pathological condition: French sleep expert, Michel Jouvet and his team reported the case of a patient who was quasi sleep deprived for 4 months, as confirmed by repeated polygraphic recordings showing less than 30 min (of stage I sleep) per night, a condition they named “agrypnia”. The 27 year-old man was suffering from Morvan’s fibrillary chorea, a rare disease that leads to involuntary movements, and in this particular case extreme insomnia. The researchers found that treatment with 5-HTP restored almost normal sleep stages, however some months after this recovery the patient died during a relapse which was unresponsive to 5-HTP. Despite the extreme insomnia, psychological investigation showed no sign of cognitive deficits, except for some hallucinations[73].
See also
- Effects of sleep deprivation on cognitive performance
- Narcolepsy
- Polyphasic sleep
- Sleep debt
- Sleep medicine
- Sleep onset latency
- Wake therapy
References
- ^ Rechtschaffen,A Bergmann, B, "Sleep deprivation in the rat by the disk-over-water method" Behavioural Brain Research Volume 69, Issues 1-2, July-August 1995, Pages 55-63 The Function of Sleep doi:10.1016/0166-4328(95)00020-T
- ^ a b Taheri S, Lin L, Austin D, Young T, Mignot E (2004). "Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index". PLoS Med. 1 (3): e62. doi:10.1371/journal.pmed.0010062. PMC 535701. PMID 15602591.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Kushida, Clete Anthony (2005). Sleep deprivation. Informa Health Care. pp. 1–2. ISBN 0824759494.
- ^ Reference list is found on image page in Commons: Commons:File:Effects of sleep deprivation.svg#References
- ^ a b c d e "http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Sleep_deprivation?OpenDocument".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ "http://www.apa.org/ed/topss/bryanread.html".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ Morin, Charles M. (2003). Insomnia. New York: Kluwer Academic/Plenum Publ. p. 28. ISBN 0306477505.
- ^ National Institute of Neurological Disorders and Stroke — Brain Basics: Understanding Sleep
- ^ Smith, Andrew P. (1992). Handbook of Human Performance. London: Acad. Press. p. 240. ISBN 0126503524.
- ^ http://www.fi.edu/learn/brain/sleep.html
- ^ a b http://www.health.harvard.edu/press_releases/sleep_deprivation_problem.htm
- ^ http://web.mit.edu/london/www/magnesium.html
- ^ Teachers of Psychology in Secondary Schools
- ^ http://www.decp.org/pdfs/nystagmus.pdf
- ^ Neural Link Between Sleep Loss And Psychiatric Disorders
- ^ Gottlieb DJ, Punjabi NM, Newman AB; et al. (2005). "Association of sleep time with diabetes mellitus and impaired glucose tolerance". Arch. Intern. Med. 165 (8): 863–7. doi:10.1001/archinte.165.8.863. PMID 15851636.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Spiegel, K. (1999-10-23). "Impact of sleep debt on metabolic and endocrine function". The Lancet. 354 (9188): 1435–9. doi:10.1016/S0140-6736(99)01376-8. PMID 10543671.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "http://www.fi.edu/brain/sleep.htm".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ "http://health.ucsd.edu/news/2000_02_09_Sleep.html".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ Goes FS, Zandi PP, Miao K; et al. (2007). "Mood-incongruent psychotic features in bipolar disorder: familial aggregation and suggestive linkage to 2p11-q14 and 13q21-33". Am J Psychiatry. 164 (2): 236–47. doi:10.1176/appi.ajp.164.2.236. PMID 17267786.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Siegel, Jerome M. (November 2003). "Why We Sleep" (PDF). Scientific American. Retrieved 2008-04-03.
- ^ No sleep means no new brain cells
- ^ Vgontzas AN, Mastorakos G, Bixler EO, Kales A, Gold PW, Chrousos GP (1999). "Sleep deprivation effects on the activity of the hypothalamic-pituitary-adrenal and growth axes: potential clinical implications". Clin. Endocrinol. 51 (2): 205–15. doi:10.1046/j.1365-2265.1999.00763.x. PMID 10468992.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mostaghimi, L.; Obermeyer, WH; Ballamudi, B; Martinez-Gonzalez, D; Benca, RM (2005). "Effects of sleep deprivation on wound healing". Journal of Sleep Research. 14 (3): 213. doi:10.1111/j.1365-2869.2005.00455.x. PMID 16120095.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gümüştekín K, Seven B, Karabulut N; et al. (2004). "Effects of sleep deprivation, nicotine, and selenium on wound healing in rats". Int. J. Neurosci. 114 (11): 1433–42. doi:10.1080/00207450490509168. PMID 15636354.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Van Dongen HA; et al. (2002). "The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation" (PDF). Sleep. 26 (2): 117–26. PMID 12683469.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ a b "Drowsy Driving Fact Sheet" (PDF). 2 December 2009.
{{cite web}}: Unknown parameter|site=ignored (help) - ^ a b Siri Carpenter (2001). "Sleep deprivation may be undermining teen health". 32 (9).
{{cite journal}}: Cite journal requires|journal=(help) Cite error: The named reference "SleepDepReport" was defined multiple times with different content (see the help page). - ^ Williamson AM, Feyer AM (2000). "Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication". Occup Environ Med. 57 (10): 649–55. doi:10.1136/oem.57.10.649. PMC 1739867. PMID 10984335.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Dawson, Drew and Kathryn Reid (1997). "Fatigue, alcohol and performance impairment". Nature. 388 (6639): 235. doi:10.1038/40775. PMID 9230429.
- ^ Drummond, SEAN P.A.; Paulus, MP; Tapert, SF (2006). "Effects of two nights sleep deprivation and two nights recovery sleep on response inhibition". Journal of Sleep Research. 15 (3): 261. doi:10.1111/j.1365-2869.2006.00535.x. PMID 16911028.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Timothy Roehrs; et al. (1994). "Sleepiness and ethanol effects on simulated driving". Alcoholism:clinical and experimental research. 18 (1): 154–158. doi:10.1111/j.1530-0277.1994.tb00896.x.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ^ "Drowsy Driving:Key Messages and Talking Points" (PDF). 2 December 2009.
{{cite web}}: Unknown parameter|site=ignored (help) - ^ Dave Michaels (2December 2009). "FAA Won't Allow Cockpit Naps as Part of Plan to Reduce Pilot Fatigue".
{{cite web}}: Check date values in:|date=(help) - ^ Baldwinn, DeWitt C. Jr. and Steven R. Daugherty (2004). "Sleep Deprivation and Fatigue in Residency Training: Results of a National Survey of First- and Second-Year Residents". Sleep. 27 (2): 217–223. PMID 15124713.
- ^ Coren, Stanley (01 March 1998). "Sleep Deprivation, Psychosis and Mental Efficiency". Psychiatric Times. 15 (3). Retrieved 2009-11-25.
{{cite journal}}: Check date values in:|date=(help) - ^ Does the lack of sleep make you fat?, Bristol University Press Release, December 7, 2004
- ^ Hasler G, Buysse DJ, Klaghofer R; et al. (2004). "The association between short sleep duration and obesity in young adults: a 13-year prospective study". Sleep. 27 (4): 661–6. PMID 15283000.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB (2005). "Inadequate sleep as a risk factor for obesity: analyses of the NHANES I". Sleep. 28 (10): 1289–96. PMID 16295214.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Van Cauter E, Spiegel K (1999). "Sleep as a mediator of the relationship between socioeconomic status and health: a hypothesis". Ann. N. Y. Acad. Sci. 896: 254–61. doi:10.1111/j.1749-6632.1999.tb08120.x. PMID 10681902.
- ^ P. Franken, D.J. Dijk, I. Tobler and A.A. Borbely (1991). "Sleep deprivation in rats: effects on EEG power spectra, vigilance states, and cortical temperature". Am J Physiol Regul Integr Comp Physiol. 261 (1 Pt 2): R198–R208. PMID 1858947.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rechtschaffen A, Bergmann BM, Gilliland MA, Bauer K (1999). "Effects of method, duration, and sleep stage on rebounds from sleep deprivation in the rat". Sleep. 22 (1): 11–31. PMID 9989363.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jouvet D, Vimont P, Delorme F, Jouvet M (1964). "[Study of selective deprivation of the paradoxal sleep phase in the cat.]". C. R. Seances Soc. Biol. Fil. (in French). 158: 756–9. PMID 14186938.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Harry B. Cohen and William C. Dement (1965). "Sleep: Changes in Threshold to Electroconvulsive Shock in Rats after Deprivation of "Paradoxical" Phase". Science. 150 (3701): 1318–9. doi:10.1126/science.150.3701.1318. PMID 5857002.
- ^ van Hulzen ZJ, Coenen AM (1981). "Paradoxical sleep deprivation and locomotor activity in rats". Physiol. Behav. 27 (4): 741–4. doi:10.1016/0031-9384(81)90250-X. PMID 7323178.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Van Hulzen ZJ, Coenen AM (1980). "The pendulum technique for paradoxical sleep deprivation in rats". Physiol. Behav. 25 (6): 807–11. doi:10.1016/0031-9384(80)90298-X. PMID 7220622.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Binyam Mohamed torture appeal lost by UK government". BBC News. 2009-10-02.
- ^ Begin, Menachem (1979). White nights: the story of a prisoner in Russia. San Francisco: Harper & Row. ISBN 0-06-010289-6.
- ^ Ireland v. the United Kingdom paragraph 102
- ^ Hassan T (2006-10-03). "Sleep deprivation remains red-hot question". PM. abc.net.au.
- ^ "Sleep deprivation is torture: Amnesty". The Sydney Morning Herald. AAP. 2006-10-03.
- ^ Gorgulu Y, Caliyurt O. (2009). Rapid antidepressant effects of sleep deprivation therapy correlates with serum BDNF changes in major depression. Brain Res Bull. 80(3):158-62. PMID 19576267
- ^ Selvi, Yavuz (17 Aug 2007). "Mood changes after sleep deprivation in morningness–eveningness chronotypes in healthy individuals" (Abstract). Journal of Sleep Research. 16 (3). European Sleep Research Society: 241–4. doi:10.1111/j.1365-2869.2007.00596.x. PMID 17716271. Retrieved 2009-06-17.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wirz-Justice A, Van den Hoofdakker RH (1999). "Sleep deprivation in depression: what do we know, where do we go?". Biol. Psychiatry. 46 (4): 445–53. doi:10.1016/S0006-3223(99)00125-0. PMID 10459393.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sleep Disorder Treatments
- ^ msnbc.com | Amid recession, meth menace evolves
- ^ Morris Police Department | Methamphetamines
- ^ WebSciences.org | Psychiatric Co-morbidity
- ^ "http://sleepdisorders.about.com/cs/sleepdeprivation/a/depstudents.htm".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ Tsai LL, Li SP (2004). "Sleep patterns in college students; Gender and grade differences". J Psychosom Res. 56 (2): 231–7. doi:10.1016/S0022-3999(03)00507-5. PMID 15016583.
- ^ "http://abcnews.go.com/US/wireStory?id=1775003".
{{cite journal}}: Cite journal requires|journal=(help); External link in|title= - ^ Giedd, Jay N., Brain Imaging Unit, Child Psychiatry Branch, National Institute of Mental Health, Bethesda, MD, US Journal of Adolescent Health, Vol 45(4), Oct, 2009. pp. 319-320.
- ^ "Sleep Deprivation Fact Sheet" (PDF). 2 December 2009.
{{cite web}}: Unknown parameter|site=ignored (help) - ^ Coren S (1998). "Sleep Deprivation, Psychosis and Mental Efficiency". Psychiatric Time. 15 (3).
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Thangham CV (2007). "What happens when you stay awake for eleven days?". Digital Journal.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Vu Phuong Thao (2006-02-14). "Vietnam man handles three decades without sleep". Translated by Thu Thuy. Thanh Nien.
- ^ a b Thanh Hai (2007-04-16). "My kingdom for a snooze". Vietnam Investment Review.
- ^ Xenophilia - News Archives: Biology (2005)
- ^ "Matters of dispute - Sleepless in Ukraine", Shortcuts, The Guardian, 10 Feb 2005 [1] Accessed 11 May 2010
- ^ Childs, Dan (March 30, 2009). "The Boy Who Couldn't Sleep". ABC News. Retrieved March 31, 2009.
- ^ http://www.wtsp.com/news/local/story.aspx?storyid=80326# Toddler finally gets a good night sleep
- ^ http://abcnews.go.com/GMA/OnCall/story?id=6711810&page=1 Mystery of Sleepless Boy Solved : Boy Who Couldn't Sleep Undergoes Risky, Life-Changing Operation
- ^ One case of agrypnia (4 months without sleep) in a morvan disease, favourable action of 5-hydroxytryptophane. C. Fischer-Perroudon, J. Mouret et M. Jouvet. Electroencephalography and Clinical Neurophysiology, 1974, 36: 1-18
