User:Mr. Ibrahem/Acute lymphoblastic leukemia
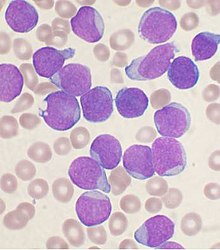
Acute lymphoblastic leukemia (ALL) is a cancer of the lymphoid line of blood cells characterized by the development of large numbers of immature lymphocytes.[1] Symptoms may include feeling tired, pale skin color, fever, easy bleeding or bruising, enlarged lymph nodes, or bone pain.[1] As an acute leukemia, ALL progresses rapidly and is typically fatal within weeks or months if left untreated.[10]
In most cases, the cause is unknown.[2] Genetic risk factors may include Down syndrome, Li-Fraumeni syndrome, or neurofibromatosis type 1.[1] Environmental risk factors may include significant radiation exposure or prior chemotherapy.[1] Evidence regarding electromagnetic fields or pesticides is unclear.[4][6] Some hypothesize that an abnormal immune response to a common infection may be a trigger.[4] The underlying mechanism involves multiple genetic mutations that results in rapid cell division.[2] The excessive immature lymphocytes in the bone marrow interfere with the production of new red blood cells, white blood cells, and platelets.[1] Diagnosis is typically based on blood tests and bone marrow examination.[3]
ALL is typically treated initially with chemotherapy aimed at bringing about remission.[2] This is then followed by further chemotherapy typically over a number of years.[2] Additional treatments may include intrathecal chemotherapy or radiation therapy if spread to the brain has occurred.[2] Stem cell transplantation may be used if the disease recurs following standard treatment.[2] Additional treatments such as immunotherapy are being studied.[2]
ALL affected about 876,000 people globally in 2015 and resulted in about 111,000 deaths.[11][9] It occurs most commonly in children, particularly those between the ages of two and five.[12][4] In the United States it is the most common cause of cancer and death from cancer among children.[2] ALL is notable for being the first disseminated cancer to be cured.[13] Survival for children increased from under 10% in the 1960s to 90% in 2015.[2] Survival rates remain lower for babies (50%)[14] and adults (35%).[7]
References[edit]
- ^ a b c d e f g h "Childhood Acute Lymphoblastic Leukemia Treatment". National Cancer Institute. 8 December 2017. Retrieved 20 December 2017.
- ^ a b c d e f g h i j k l Hunger, Stephen P.; Mullighan, Charles G. (14 October 2015). "Acute Lymphoblastic Leukemia in Children". New England Journal of Medicine. 373 (16): 1541–1552. doi:10.1056/nejmra1400972. PMID 26465987. S2CID 609394.
- ^ a b c d Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 743. ISBN 9780323529570.
- ^ a b c d e Inaba H, Greaves M, Mullighan CG (June 2013). "Acute lymphoblastic leukaemia". Lancet. 381 (9881): 1943–55. doi:10.1016/S0140-6736(12)62187-4. PMC 3816716. PMID 23523389.
- ^ a b Baljevic, Muhamed; Jabbour, Elias; O'Brien, Susan; Kantarjian, Hagop M (2016). "Acute Lymphoblastic Leukemia". In Kantarjian, HM; Wolff, RA (eds.). The MD Anderson Manual of Medical Oncology (3 ed.). New York: McGraw-Hill Education. Retrieved 22 November 2017.
- ^ a b Childhood acute lymphoblastic leukemia. Vora, Ajay (editor). Cham, Switzerland: Springer International Publishing. 2017. pp. 1–44, 61–86. ISBN 9783319397078. OCLC 984342596.
{{cite book}}: CS1 maint: others (link) - ^ a b Paul, Shilpa; Kantarjian, Hagop; Jabbour, Elias J. (November 2016). "Adult Acute Lymphoblastic Leukemia". Mayo Clinic Proceedings. 91 (11): 1645–1666. doi:10.1016/j.mayocp.2016.09.010. PMID 27814839.
- ^ Boer, JM; den Boer, ML (11 July 2017). "BCR-ABL1-like acute lymphoblastic leukaemia: From bench to bedside". European Journal of Cancer. 82: 203–218. doi:10.1016/j.ejca.2017.06.012. PMID 28709134.
- ^ a b GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ Marino, Bradley S.; Fine, Katie S. (2013). Blueprints Pediatrics. Lippincott Williams & Wilkins. p. 205. ISBN 9781451116045.
- ^ GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ "Acute Lymphocytic Leukemia - Cancer Stat Facts". SEER. Retrieved 20 December 2017.
- ^ Tubergen, DG; Bleyer, A; Ritchey, AK (2011). "Acute Lymphoblastic Leukemia". In Kliegman, RM; Stanton, BMD; St Geme, J; Schor, NF; Behrman, RE (eds.). Nelson Textbook of Pediatrics (19th ed.). Philadelphia, PA: Elsevier/Saunders. pp. 1732–1737. ISBN 978-1437707557. OCLC 706780860.
- ^ Brown, Patrick (6 December 2013). "Treatment of infant leukemias: challenge and promise". Hematology. 2013 (1): 596–600. doi:10.1182/asheducation-2013.1.596. PMC 4729208. PMID 24319237.