Diffuse midline glioma: Difference between revisions
Improved writing style, updated nomenclature in intro, removed the definitions of brainstem |
consistent citation formatting; templated cites |
||
| Line 2: | Line 2: | ||
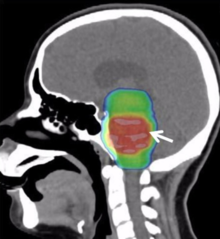
[[File:Palliative Care Options for a Young Adult Patient with a Diffuse Intrinsic Pontine Glioma - Fig. 1 (cropped).png|thumb|[[Magnetic resonance imaging]] of a diffuse intrinsic pontine glioma.]] |
[[File:Palliative Care Options for a Young Adult Patient with a Diffuse Intrinsic Pontine Glioma - Fig. 1 (cropped).png|thumb|[[Magnetic resonance imaging]] of a diffuse intrinsic pontine glioma.]] |
||
'''Diffuse midline glioma (DMG),''' previously called '''Diffuse Intrinsic Pontine Glioma (DIPG)''' is a fatal [[tumour]] that arises in the brainstem; most commonly in the pons or thalamus. DMG is believed to be caused by genetic mutations that cause epigenetic changes in cells of the developing nervous system, resulting in a failure of the cells to properly differentiate<ref>{{ |
'''Diffuse midline glioma (DMG),''' previously called '''Diffuse Intrinsic Pontine Glioma (DIPG)''' is a fatal [[tumour]] that arises in the brainstem; most commonly in the pons or thalamus. DMG is believed to be caused by genetic mutations that cause epigenetic changes in cells of the developing nervous system, resulting in a failure of the cells to properly differentiate<ref>{{cite journal | vauthors = Vanan MI, Eisenstat DD | title = DIPG in Children - What Can We Learn from the Past? | journal = Frontiers in Oncology | volume = 5 | pages = 237 | date = 2015 | doi = 10.3389/fonc.2015.00237/full }}</ref><ref>{{cite journal | vauthors = Baker SJ, Ellison DW, Gutmann DH | title = Pediatric gliomas as neurodevelopmental disorders | journal = Glia | volume = 64 | issue = 6 | pages = 879–895 | date = June 2016 | pmid = 26638183 | pmc = 4833573 | doi = 10.1002/glia.22945 }}</ref>. Currently, the standard of care is fractionated external beam radiotherapy, as the tumour location precludes surgery, and chemotherapy has shown to be ineffective<ref>{{cite journal | vauthors = Williams JR, Young CC, Vitanza NA, McGrath M, Feroze AH, Browd SR, Hauptman JS | title = Progress in diffuse intrinsic pontine glioma: advocating for stereotactic biopsy in the standard of care | language = en-US | journal = Neurosurgical Focus | volume = 48 | issue = 1 | pages = E4 | date = January 2020 | doi = 10.3171/2019.9.FOCUS19745 }}</ref><ref>{{cite journal | vauthors = Bailey CP, Figueroa M, Mohiuddin S, Zaky W, Chandra J | title = Cutting Edge Therapeutic Insights Derived from Molecular Biology of Pediatric High-Grade Glioma and Diffuse Intrinsic Pontine Glioma (DIPG) | journal = Bioengineering | volume = 5 | issue = 4 | pages = 88 | date = October 2018 | doi = 10.3390/bioengineering5040088 }}</ref>, however the estimated survival post-diagnosis remains only 9-15 months. |
||
==Diagnosis== |
==Diagnosis== |
||
| Line 13: | Line 13: | ||
==Treatment== |
==Treatment== |
||
The standard treatment for DIPG is 6 weeks of [[radiation therapy]], which often dramatically improves symptoms. However, symptoms usually recur after 6 to 9 months and progress rapidly.<ref>St Jude Children's Research Hospital |
The standard treatment for DIPG is 6 weeks of [[radiation therapy]], which often dramatically improves symptoms. However, symptoms usually recur after 6 to 9 months and progress rapidly.<ref>{{cite web | work = St Jude Children's Research Hospital | title = Diffuse Intrinsic Pontine Glioma (DIPG) | url = https://www.stjude.org/disease/diffuse-intrinsic-pontine-glioma.html }}</ref> |
||
===Neurosurgery=== |
===Neurosurgery=== |
||
| Line 28: | Line 28: | ||
===Chemotherapy and other drug therapies=== |
===Chemotherapy and other drug therapies=== |
||
The role of chemotherapy in DIPG remains unclear. Studies have shown little improvement in survival, although efforts (see below) through the Children's Oncology Group (COG), Paediatric Brain Tumour Consortium (PBTC), and others are underway to explore further the use of chemotherapy and other drugs. Drugs that increase the effect of radiotherapy ([[radiosensitizer]]s) have shown no added benefit, but promising new agents are under investigation. [[Cancer immunotherapy|Immunotherapy]] with [[Interferon type I|beta-interferon]] and other drugs has also had little effect in trials. Intensive or high-dose chemotherapy with [[Hematopoietic stem cell transplantation|autologous bone marrow transplantation]] or peripheral blood stem cell rescue has not demonstrated any effectiveness in brain stem gliomas. Future clinical trials may involve medicines designed to interfere with cellular pathways (signal transfer inhibitors), or other approaches that alter the tumor or its environment.<ref> |
The role of chemotherapy in DIPG remains unclear. Studies have shown little improvement in survival, although efforts (see below) through the Children's Oncology Group (COG), Paediatric Brain Tumour Consortium (PBTC), and others are underway to explore further the use of chemotherapy and other drugs. Drugs that increase the effect of radiotherapy ([[radiosensitizer]]s) have shown no added benefit, but promising new agents are under investigation. [[Cancer immunotherapy|Immunotherapy]] with [[Interferon type I|beta-interferon]] and other drugs has also had little effect in trials. Intensive or high-dose chemotherapy with [[Hematopoietic stem cell transplantation|autologous bone marrow transplantation]] or peripheral blood stem cell rescue has not demonstrated any effectiveness in brain stem gliomas. Future clinical trials may involve medicines designed to interfere with cellular pathways (signal transfer inhibitors), or other approaches that alter the tumor or its environment.<ref>{{cite web | vauthors = Fisher PG, Monje M | title = Brain Stem Gliomas in Childhood | url = https://childhoodbraintumor.org/brain-stem-gliomas-in-childhood/ | publisher = Childhood Brain Tumor Foundation | location = Germantown, Maryland | date = 10 May 2010 }}</ref><ref name="pmid11013373">{{cite journal | vauthors = Fisher PG, Breiter SN, Carson BS, Wharam MD, Williams JA, Weingart JD, Foer DR, Goldthwaite PT, Tihan T, Burger PC | display-authors = 6 | title = A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as distinct entities | journal = Cancer | volume = 89 | issue = 7 | pages = 1569–1576 | date = October 2000 | pmid = 11013373 | doi = 10.1002/1097-0142(20001001)89:7<1569::aid-cncr22>3.0.co;2-0 }}</ref><ref name="pmid16525181">{{cite journal | vauthors = Donaldson SS, Laningham F, Fisher PG | title = Advances toward an understanding of brainstem gliomas | journal = Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology | volume = 24 | issue = 8 | pages = 1266–72 | date = March 2006 | pmid = 16525181 | doi = 10.1200/JCO.2005.04.6599 }}</ref> |
||
==Prognosis== |
==Prognosis== |
||
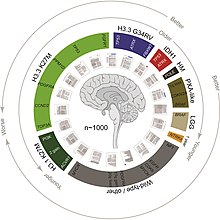
[[File:Integrated Molecular Meta-Analysis of 1,000 Pediatric High-Grade and Diffuse Intrinsic Pontine Glioma - graphical abstract.jpg|thumb|Summary of a [[meta analysis]] of over 1,000 cases of DIPG and [[Grading (tumors)|high-grade]] pediatric gliomas, highlighting the mutations involved as well as generic outcome information.]] |
[[File:Integrated Molecular Meta-Analysis of 1,000 Pediatric High-Grade and Diffuse Intrinsic Pontine Glioma - graphical abstract.jpg|thumb|Summary of a [[meta analysis]] of over 1,000 cases of DIPG and [[Grading (tumors)|high-grade]] pediatric gliomas, highlighting the mutations involved as well as generic outcome information.]] |
||
DIPG is a [[terminal illness]], since it has a 5-year survival rate of <1%. The median overall survival of children diagnosed with DIPG is approximately 9 months. The 1- and 2-year survival rates are approximately 30% and less than 10%, respectively. These statistics make DIPG one of the most devastating pediatric [[cancer]]s.<ref>Treatment of newly diagnosed diffuse brain stem gliomas in children |
DIPG is a [[terminal illness]], since it has a 5-year survival rate of <1%. The median overall survival of children diagnosed with DIPG is approximately 9 months. The 1- and 2-year survival rates are approximately 30% and less than 10%, respectively. These statistics make DIPG one of the most devastating pediatric [[cancer]]s.<ref name="pmid17492930">{{cite journal | vauthors = Korones DN | title = Treatment of newly diagnosed diffuse brain stem gliomas in children: in search of the holy grail | journal = Expert Review of Anticancer Therapy | volume = 7 | issue = 5 | pages = 663–74 | date = May 2007 | pmid = 17492930 | doi = 10.1586/14737140.7.5.663 }}</ref> Although 75–85% of patients show some improvement in their symptoms after [[radiation therapy]], DIPGs almost always begin to grow again (called recurrence, relapse, or progression). [[Clinical trial]]s have reported that the median time between radiation therapy and progression is 5–8.8 months.<ref name="dipgregistry.org">{{cite web|url=http://www.dipgregistry.org/patients-families/recurrence-relapse/|title=Recurrence/Relapse – DIPG Registry<!-- Bot generated title -->|publisher=|access-date=20 December 2018|archive-url=https://web.archive.org/web/20150409031200/http://www.dipgregistry.org/patients-families/recurrence-relapse/|archive-date=9 April 2015|url-status=dead}}</ref> Patients whose tumors begin to grow again may be eligible for experimental treatment through clinical trials to try to slow or stop the growth of the tumor. However, clinical trials have not shown any significant benefit from experimental DIPG therapies so far.<ref name="dipgregistry.org"/> |
||
DIPGs that progress usually grow quickly and affect important parts of the brain. The median time from tumor progression to death is usually very short, between 1 and 4.5 months. During this time, doctors focus on [[palliative care]]: controlling symptoms and making the patient as comfortable as possible.<ref name="dipgregistry.org" /> |
DIPGs that progress usually grow quickly and affect important parts of the brain. The median time from tumor progression to death is usually very short, between 1 and 4.5 months. During this time, doctors focus on [[palliative care]]: controlling symptoms and making the patient as comfortable as possible.<ref name="dipgregistry.org" /> |
||
| Line 39: | Line 39: | ||
[[File:Mutations in diffuse intrinsic pontine glioma samples from several anatomical locations - Ncomms11185-f1.jpg|thumb|Mutations in diffuse intrinsic pontine glioma samples from several anatomical locations.]] |
[[File:Mutations in diffuse intrinsic pontine glioma samples from several anatomical locations - Ncomms11185-f1.jpg|thumb|Mutations in diffuse intrinsic pontine glioma samples from several anatomical locations.]] |
||
[[File:Drug delivery to diffuse intrinsic pontine glioma (DIPG) - Fphar-08-00495-g004.jpg|thumb|Schematic of a currently experimental approach to DIPG drug delivery involving [[nanoparticle]]s and [[stem cell]]s.]] |
[[File:Drug delivery to diffuse intrinsic pontine glioma (DIPG) - Fphar-08-00495-g004.jpg|thumb|Schematic of a currently experimental approach to DIPG drug delivery involving [[nanoparticle]]s and [[stem cell]]s.]] |
||
As is the case with most brain tumors, a major difficulty in treating DIPG is overcoming the [[blood–brain barrier]].<ref> |
As is the case with most brain tumors, a major difficulty in treating DIPG is overcoming the [[blood–brain barrier]].<ref>{{cite web | url = http://www.justonemoreday.org/Research/HurdlesforDIPGResearch.html | archive-url = https://web.archive.org/web/20120701111050/http://www.justonemoreday.org/Research/HurdlesforDIPGResearch.html | archive-date = 1 July 2012 | title = Getting into the brain: approaches to enhance brain drug delivery | work = Just One More Day }}</ref><ref name="Patel_2009">{{cite journal | vauthors = Patel MM, Goyal BR, Bhadada SV, Bhatt JS, Amin AF | title = Getting into the brain: approaches to enhance brain drug delivery | journal = CNS Drugs | volume = 23 | issue = 1 | pages = 35–58 | date = 2009 | pmid = 19062774 | doi = 10.2165/0023210-200923010-00003 }}</ref> |
||
In the brain – unlike in other areas of the body, where substances can pass freely from the blood into the tissue – there is very little space between the cells lining the blood vessels. Thus, the movement of substances into the brain is significantly limited. This barrier is formed by the lining cells of the vessels as well as by projections from nearby [[astrocyte]]s. These two types of cells are knitted together by proteins to form what are called "tight junctions". The entire structure is called the blood–brain barrier (BBB). It prevents chemicals, toxins, bacteria, and other substances from getting into the brain, and thus serves a continuous protective function. However, with diseases such as brain tumors, the BBB can also prevent diagnostic and therapeutic agents from reaching their target. |
In the brain – unlike in other areas of the body, where substances can pass freely from the blood into the tissue – there is very little space between the cells lining the blood vessels. Thus, the movement of substances into the brain is significantly limited. This barrier is formed by the lining cells of the vessels as well as by projections from nearby [[astrocyte]]s. These two types of cells are knitted together by proteins to form what are called "tight junctions". The entire structure is called the blood–brain barrier (BBB). It prevents chemicals, toxins, bacteria, and other substances from getting into the brain, and thus serves a continuous protective function. However, with diseases such as brain tumors, the BBB can also prevent diagnostic and therapeutic agents from reaching their target. |
||
| Line 46: | Line 46: | ||
* '''Intrathecal/intraventricular administration''': Chemotherapy is injected directly into the [[cerebrospinal fluid]], either through a [[lumbar puncture]] or a surgically implanted [[catheter]]. |
* '''Intrathecal/intraventricular administration''': Chemotherapy is injected directly into the [[cerebrospinal fluid]], either through a [[lumbar puncture]] or a surgically implanted [[catheter]]. |
||
* '''Intracerebral implants''': A neurosurgeon creates a cavity within a tumor to allow the placement of dime-sized chemotherapy wafers, such as Gliadel wafers. Several of these wafers can be placed at the time of surgery and will release the chemotherapy agent [[carmustine]] slowly over time. This provides a much higher concentration of chemotherapy in the brain than can be obtained with intravenous administration, and it causes fewer systemic [[side effect]]s. However, it is an option only for patients with surgically resectable tumours; it cannot be used to treat DIPG.<ref>{{Cite web |url=http://www.gliadel.com/consumer/about/moa_video.aspx |title=MOA Video |access-date=2015-04-13 |archive-url=https://web.archive.org/web/20100505213653/http://www.gliadel.com/consumer/about/moa_video.aspx |archive-date=2010-05-05 |url-status=dead }}</ref> |
* '''Intracerebral implants''': A neurosurgeon creates a cavity within a tumor to allow the placement of dime-sized chemotherapy wafers, such as Gliadel wafers. Several of these wafers can be placed at the time of surgery and will release the chemotherapy agent [[carmustine]] slowly over time. This provides a much higher concentration of chemotherapy in the brain than can be obtained with intravenous administration, and it causes fewer systemic [[side effect]]s. However, it is an option only for patients with surgically resectable tumours; it cannot be used to treat DIPG.<ref>{{Cite web |url=http://www.gliadel.com/consumer/about/moa_video.aspx |title=MOA Video |access-date=2015-04-13 |archive-url=https://web.archive.org/web/20100505213653/http://www.gliadel.com/consumer/about/moa_video.aspx |archive-date=2010-05-05 |url-status=dead }}</ref> |
||
* '''Osmotic blood–brain barrier disruption (BBBD):''' The cells of the blood–brain barrier are shrunk by a concentrated sugar solution ([[mannitol]]). This opens the barrier and allows 10 to 100 times more chemotherapy to enter the brain. A catheter is placed into a large artery (usually the one in the groin called the [[femoral artery]]) and threaded up to the [[Common carotid artery|carotid]] or [[vertebral artery]]. The hypertonic mannitol is injected, followed by a chemotherapeutic agent. Patients spend a few days in the hospital for each administration. This has been attempted with DIPG tumours.<ref>Osmotic blood-brain barrier |
* '''Osmotic blood–brain barrier disruption (BBBD):''' The cells of the blood–brain barrier are shrunk by a concentrated sugar solution ([[mannitol]]). This opens the barrier and allows 10 to 100 times more chemotherapy to enter the brain. A catheter is placed into a large artery (usually the one in the groin called the [[femoral artery]]) and threaded up to the [[Common carotid artery|carotid]] or [[vertebral artery]]. The hypertonic mannitol is injected, followed by a chemotherapeutic agent. Patients spend a few days in the hospital for each administration. This has been attempted with DIPG tumours.<ref name="pmid16314949">{{cite journal | vauthors = Hall WA, Doolittle ND, Daman M, Bruns PK, Muldoon L, Fortin D, Neuwelt EA | title = Osmotic blood-brain barrier disruption chemotherapy for diffuse pontine gliomas | journal = Journal of Neuro-oncology | volume = 77 | issue = 3 | pages = 279–84 | date = May 2006 | pmid = 16314949 | doi = 10.1007/s11060-005-9038-4 }}</ref> |
||
* '''Convection-enhanced delivery:''' Chemotherapy is delivered to the tumour by a surgically implanted catheter under a pressure gradient to achieve more distribution than with diffusion alone. Limited experiments have been conducted with brain tumors, including one with a DIPG.<ref>Real-time image-guided direct |
* '''Convection-enhanced delivery:''' Chemotherapy is delivered to the tumour by a surgically implanted catheter under a pressure gradient to achieve more distribution than with diffusion alone. Limited experiments have been conducted with brain tumors, including one with a DIPG.<ref name="pmid17639894">{{cite journal | vauthors = Lonser RR, Warren KE, Butman JA, Quezado Z, Robison RA, Walbridge S, Schiffman R, Merrill M, Walker ML, Park DM, Croteau D, Brady RO, Oldfield EH | display-authors = 6 | title = Real-time image-guided direct convective perfusion of intrinsic brainstem lesions. Technical note | journal = Journal of Neurosurgery | volume = 107 | issue = 1 | pages = 190–197 | date = July 2007 | pmid = 17639894 | doi = 10.3171/JNS-07/07/0190 }}</ref> |
||
* '''Drug carriers:''' Carriers such as "Trojan horse" molecules, [[liposome]]s, and [[nanoparticle]]s might theoretically allow a therapeutic drug to enter the brain. Such tactics are mostly in the investigatory stages and are not yet clinically relevant to brain tumour treatment.<ref name=" |
* '''Drug carriers:''' Carriers such as "Trojan horse" molecules, [[liposome]]s, and [[nanoparticle]]s might theoretically allow a therapeutic drug to enter the brain. Such tactics are mostly in the investigatory stages and are not yet clinically relevant to brain tumour treatment.<ref name="Patel_2009" /> |
||
== Prominent patients == |
== Prominent patients == |
||
* Karen Armstrong (1959–1962), daughter of American astronaut [[Neil Armstrong]] and his first wife, Janet Elizabeth Shearon.<ref>{{cite book | |
* Karen Armstrong (1959–1962), daughter of American astronaut [[Neil Armstrong]] and his first wife, Janet Elizabeth Shearon.<ref>{{cite book | vauthors = Hansen JR |title=First Man: The Life of Neil A. Armstrong |location=New York |publisher=Simon & Schuster |year=2005 |isbn=978-0-7432-5631-5 |oclc=937302502 |title-link=First Man: The Life of Neil A. Armstrong|pages=161–164}}</ref> |
||
* Elena Desserich (2000–2007), daughter of Brooke and Keith Desserich. After her passing her parents founded The Cure Starts Now Foundation,<ref>{{cite web |url=https://www.thecurestartsnow.org/ |title=Home |website=thecurestartsnow.org}}</ref> the first international DIPG/DMG charity that today has funded over $12 million in research at 114 hospitals. Her story was also chronicled in ''[[Notes Left Behind]]'' and became a New York Times bestselling book on November 12, 2009.<ref>{{cite web |url=http://www.notesleftbehind.com/ |title=Home |website=notesleftbehind.com}}</ref> |
* Elena Desserich (2000–2007), daughter of Brooke and Keith Desserich. After her passing her parents founded The Cure Starts Now Foundation,<ref>{{cite web |url=https://www.thecurestartsnow.org/ |title=Home |website=thecurestartsnow.org}}</ref> the first international DIPG/DMG charity that today has funded over $12 million in research at 114 hospitals. Her story was also chronicled in ''[[Notes Left Behind]]'' and became a New York Times bestselling book on November 12, 2009.<ref>{{cite web |url=http://www.notesleftbehind.com/ |title=Home |website=notesleftbehind.com}}</ref> |
||
* Gabriella Miller (2003–2013), American childhood cancer awareness advocate who raised thousands of dollars for childhood cancer charities and founded Smashing Walnuts Foundation.<ref>{{cite news | |
* Gabriella Miller (2003–2013), American childhood cancer awareness advocate who raised thousands of dollars for childhood cancer charities and founded Smashing Walnuts Foundation.<ref>{{cite news | vauthors = Gibson C |title=Federal pediatric medical research act named for Gabriella Miller |url=https://www.washingtonpost.com/local/federal-pediatric-medical-research-act-named-for-gabriella-miller/2013/11/14/f87b42e0-4d72-11e3-be6b-d3d28122e6d4_story.html |access-date=3 February 2021 |newspaper=The Washington Post |date=14 November 2013}}</ref><ref>{{cite web |title=Our Story |url=https://smashingwalnuts.org/our-story/ |publisher=Smashing Walnuts Foundation |access-date=3 February 2021}}</ref> The [[Gabriella Miller Kids First Research Act]], signed into US law in 2014, was named after her. |
||
* [[Lauren Hill (basketball)|Lauren Hill]] (1995–2015), American freshman basketball player of [[Mount St. Joseph University]], Cincinnati. To fulfil her wish of playing basketball for the college team for one game, the [[2014 Hiram vs. Mount St. Joseph women's basketball game]] was scheduled 13 days earlier than the initially planned date and carried a brain cancer awareness message. Her efforts resulted in over $2.2 million raised for DIPG research through The Cure Starts Now Foundation.<ref>{{cite web|url=https://local12.com/news/local/cure-starts-now-reaches-22m-goal-in-honor-of-lauren-hill|publisher=Local 12|access-date=2021-05-03|title=Cure Starts Now reaches $2.2M goal in honor of Lauren Hill|date=January 2016}}</ref> |
* [[Lauren Hill (basketball)|Lauren Hill]] (1995–2015), American freshman basketball player of [[Mount St. Joseph University]], Cincinnati. To fulfil her wish of playing basketball for the college team for one game, the [[2014 Hiram vs. Mount St. Joseph women's basketball game]] was scheduled 13 days earlier than the initially planned date and carried a brain cancer awareness message. Her efforts resulted in over $2.2 million raised for DIPG research through The Cure Starts Now Foundation.<ref>{{cite web|url=https://local12.com/news/local/cure-starts-now-reaches-22m-goal-in-honor-of-lauren-hill|publisher=Local 12|access-date=2021-05-03|title=Cure Starts Now reaches $2.2M goal in honor of Lauren Hill|date=January 2016}}</ref> |
||
* Nathaniel Kayne Finley (1999-2017), born to Curtis Lee, a former member of the U.S. Armed Forces and Kirsten Darlene Finley. Finley was a member of [[USA Swimming]] through Northern Kentucky Clippers and Daytona Beach Speed swimming clubs. Despite being diagnosed with DIPG in late 2016, Finley choose to attend [[LSU]] as a [[freshman#United States|freshman]] in fall 2017, majoring in the College of Agriculture, Animal Sciences with aspirations of becoming a [[veterinarian]]. Prior to his death, Finley signed an [[advance directive]], ensuring that his tumor could be donated for scientific research, the same year, he established Cannonballs for Kayne, a DIPG research foundation, committed to families, education and funding research for a cure.<ref>Cannonballs For Kayne Foundation. Support Research. A DIPG Research Foundation</ref> |
* Nathaniel Kayne Finley (1999-2017), born to Curtis Lee, a former member of the U.S. Armed Forces and Kirsten Darlene Finley. Finley was a member of [[USA Swimming]] through Northern Kentucky Clippers and Daytona Beach Speed swimming clubs. Despite being diagnosed with DIPG in late 2016, Finley choose to attend [[LSU]] as a [[freshman#United States|freshman]] in fall 2017, majoring in the College of Agriculture, Animal Sciences with aspirations of becoming a [[veterinarian]]. Prior to his death, Finley signed an [[advance directive]], ensuring that his tumor could be donated for scientific research, the same year, he established Cannonballs for Kayne, a DIPG research foundation, committed to families, education and funding research for a cure.<ref>Cannonballs For Kayne Foundation. Support Research. A DIPG Research Foundation</ref> |
||
Revision as of 09:04, 4 December 2022
This article needs more reliable medical references for verification or relies too heavily on primary sources. (May 2017) |  |

Diffuse midline glioma (DMG), previously called Diffuse Intrinsic Pontine Glioma (DIPG) is a fatal tumour that arises in the brainstem; most commonly in the pons or thalamus. DMG is believed to be caused by genetic mutations that cause epigenetic changes in cells of the developing nervous system, resulting in a failure of the cells to properly differentiate[1][2]. Currently, the standard of care is fractionated external beam radiotherapy, as the tumour location precludes surgery, and chemotherapy has shown to be ineffective[3][4], however the estimated survival post-diagnosis remains only 9-15 months.
Diagnosis


Like most brainstem tumors, diagnosing diffuse intrinsic pontine glioma usually involves non-invasive brain imaging like MRI, in addition to neurologic physical exam. Biopsies and other procedures are very uncommon. Similar to DIPG, diffuse midline gliomas (DMG) often fall into similar categories for both diagnosis and treatment as DIPG and are often categorized together.[5] More recently, biopsies are performed so that the best option for clinical trials can be chosen.[citation needed]
In studies resulting from the DIPG/DMG Registry and in connection with the DIPG/DMG Collaborative, statistics reveal that approximately 150–300 patients are diagnosed with DIPG in the USA per year, the median age of patients with DIPG is approximately 6–7 years old and the male/female ratio of DIPG patients is 1:1.[6]
Treatment
The standard treatment for DIPG is 6 weeks of radiation therapy, which often dramatically improves symptoms. However, symptoms usually recur after 6 to 9 months and progress rapidly.[7]
Neurosurgery
Surgery to attempt tumour removal is usually not possible or advisable for DIPG. By nature, these tumors invade diffusely throughout the brain stem, growing between normal nerve cells. Aggressive surgery would cause severe damage to neural structures vital for arm and leg movement, eye movement, swallowing, breathing, and even consciousness.
A neurosurgically performed brain-stem biopsy for immunotyping of diffuse intrinsic pontine glioma has served a limited recent role in experimental clinical studies and treatment trials. This, however, is not the current standard of care, as it presents considerable risk given the biopsy location, and thus is appropriately performed only in the context of participation in an ongoing clinical treatment trial.
Pontine biopsy is in no way a therapeutic or curative surgery, and the risks (potentially catastrophic and fatal) are only outweighed when the diagnosis is uncertain (extremely unusual) or the patient is enrolled in an approved clinical trial.
Radiotherapy
Conventional radiotherapy, limited to the involved area of tumour, is the mainstay of treatment for DIPG. A total radiation dosage ranging from 5400 to 6000 cGy, administered in daily fractions of 150 to 200 cGy over 6 weeks, is standard. Hyperfractionated (twice-daily) radiotherapy was used previously to deliver higher radiation dosages, but did not lead to improved survival. Radiosurgery (e.g., gamma knife or cyberknife) has a role in the treatment of DIPG and may be considered in selected cases.
Chemotherapy and other drug therapies
The role of chemotherapy in DIPG remains unclear. Studies have shown little improvement in survival, although efforts (see below) through the Children's Oncology Group (COG), Paediatric Brain Tumour Consortium (PBTC), and others are underway to explore further the use of chemotherapy and other drugs. Drugs that increase the effect of radiotherapy (radiosensitizers) have shown no added benefit, but promising new agents are under investigation. Immunotherapy with beta-interferon and other drugs has also had little effect in trials. Intensive or high-dose chemotherapy with autologous bone marrow transplantation or peripheral blood stem cell rescue has not demonstrated any effectiveness in brain stem gliomas. Future clinical trials may involve medicines designed to interfere with cellular pathways (signal transfer inhibitors), or other approaches that alter the tumor or its environment.[8][9][10]
Prognosis
DIPG is a terminal illness, since it has a 5-year survival rate of <1%. The median overall survival of children diagnosed with DIPG is approximately 9 months. The 1- and 2-year survival rates are approximately 30% and less than 10%, respectively. These statistics make DIPG one of the most devastating pediatric cancers.[11] Although 75–85% of patients show some improvement in their symptoms after radiation therapy, DIPGs almost always begin to grow again (called recurrence, relapse, or progression). Clinical trials have reported that the median time between radiation therapy and progression is 5–8.8 months.[12] Patients whose tumors begin to grow again may be eligible for experimental treatment through clinical trials to try to slow or stop the growth of the tumor. However, clinical trials have not shown any significant benefit from experimental DIPG therapies so far.[12]
DIPGs that progress usually grow quickly and affect important parts of the brain. The median time from tumor progression to death is usually very short, between 1 and 4.5 months. During this time, doctors focus on palliative care: controlling symptoms and making the patient as comfortable as possible.[12]
Research


As is the case with most brain tumors, a major difficulty in treating DIPG is overcoming the blood–brain barrier.[13][14]
In the brain – unlike in other areas of the body, where substances can pass freely from the blood into the tissue – there is very little space between the cells lining the blood vessels. Thus, the movement of substances into the brain is significantly limited. This barrier is formed by the lining cells of the vessels as well as by projections from nearby astrocytes. These two types of cells are knitted together by proteins to form what are called "tight junctions". The entire structure is called the blood–brain barrier (BBB). It prevents chemicals, toxins, bacteria, and other substances from getting into the brain, and thus serves a continuous protective function. However, with diseases such as brain tumors, the BBB can also prevent diagnostic and therapeutic agents from reaching their target.
Researchers and clinicians have tried several methods to overcome the blood–brain barrier:
- Intrathecal/intraventricular administration: Chemotherapy is injected directly into the cerebrospinal fluid, either through a lumbar puncture or a surgically implanted catheter.
- Intracerebral implants: A neurosurgeon creates a cavity within a tumor to allow the placement of dime-sized chemotherapy wafers, such as Gliadel wafers. Several of these wafers can be placed at the time of surgery and will release the chemotherapy agent carmustine slowly over time. This provides a much higher concentration of chemotherapy in the brain than can be obtained with intravenous administration, and it causes fewer systemic side effects. However, it is an option only for patients with surgically resectable tumours; it cannot be used to treat DIPG.[15]
- Osmotic blood–brain barrier disruption (BBBD): The cells of the blood–brain barrier are shrunk by a concentrated sugar solution (mannitol). This opens the barrier and allows 10 to 100 times more chemotherapy to enter the brain. A catheter is placed into a large artery (usually the one in the groin called the femoral artery) and threaded up to the carotid or vertebral artery. The hypertonic mannitol is injected, followed by a chemotherapeutic agent. Patients spend a few days in the hospital for each administration. This has been attempted with DIPG tumours.[16]
- Convection-enhanced delivery: Chemotherapy is delivered to the tumour by a surgically implanted catheter under a pressure gradient to achieve more distribution than with diffusion alone. Limited experiments have been conducted with brain tumors, including one with a DIPG.[17]
- Drug carriers: Carriers such as "Trojan horse" molecules, liposomes, and nanoparticles might theoretically allow a therapeutic drug to enter the brain. Such tactics are mostly in the investigatory stages and are not yet clinically relevant to brain tumour treatment.[14]
Prominent patients
- Karen Armstrong (1959–1962), daughter of American astronaut Neil Armstrong and his first wife, Janet Elizabeth Shearon.[18]
- Elena Desserich (2000–2007), daughter of Brooke and Keith Desserich. After her passing her parents founded The Cure Starts Now Foundation,[19] the first international DIPG/DMG charity that today has funded over $12 million in research at 114 hospitals. Her story was also chronicled in Notes Left Behind and became a New York Times bestselling book on November 12, 2009.[20]
- Gabriella Miller (2003–2013), American childhood cancer awareness advocate who raised thousands of dollars for childhood cancer charities and founded Smashing Walnuts Foundation.[21][22] The Gabriella Miller Kids First Research Act, signed into US law in 2014, was named after her.
- Lauren Hill (1995–2015), American freshman basketball player of Mount St. Joseph University, Cincinnati. To fulfil her wish of playing basketball for the college team for one game, the 2014 Hiram vs. Mount St. Joseph women's basketball game was scheduled 13 days earlier than the initially planned date and carried a brain cancer awareness message. Her efforts resulted in over $2.2 million raised for DIPG research through The Cure Starts Now Foundation.[23]
- Nathaniel Kayne Finley (1999-2017), born to Curtis Lee, a former member of the U.S. Armed Forces and Kirsten Darlene Finley. Finley was a member of USA Swimming through Northern Kentucky Clippers and Daytona Beach Speed swimming clubs. Despite being diagnosed with DIPG in late 2016, Finley choose to attend LSU as a freshman in fall 2017, majoring in the College of Agriculture, Animal Sciences with aspirations of becoming a veterinarian. Prior to his death, Finley signed an advance directive, ensuring that his tumor could be donated for scientific research, the same year, he established Cannonballs for Kayne, a DIPG research foundation, committed to families, education and funding research for a cure.[24]
In popular culture
Notes Left Behind, a non-fictional book published in 2009, is about a girl named Elena Desserich who left hundreds of notes to her family before she died of DIPG at age 6.
References
- ^ Vanan MI, Eisenstat DD (2015). "DIPG in Children - What Can We Learn from the Past?". Frontiers in Oncology. 5: 237. doi:10.3389/fonc.2015.00237/full.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Baker SJ, Ellison DW, Gutmann DH (June 2016). "Pediatric gliomas as neurodevelopmental disorders". Glia. 64 (6): 879–895. doi:10.1002/glia.22945. PMC 4833573. PMID 26638183.
- ^ Williams JR, Young CC, Vitanza NA, McGrath M, Feroze AH, Browd SR, Hauptman JS (January 2020). "Progress in diffuse intrinsic pontine glioma: advocating for stereotactic biopsy in the standard of care". Neurosurgical Focus. 48 (1): E4. doi:10.3171/2019.9.FOCUS19745.
- ^ Bailey CP, Figueroa M, Mohiuddin S, Zaky W, Chandra J (October 2018). "Cutting Edge Therapeutic Insights Derived from Molecular Biology of Pediatric High-Grade Glioma and Diffuse Intrinsic Pontine Glioma (DIPG)". Bioengineering. 5 (4): 88. doi:10.3390/bioengineering5040088.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Diffuse Midline Gliomas". National Cancer Institute. n.d. Archived from the original on 8 October 2019. Retrieved 24 November 2019.
- ^ "DIPG Statistics".
- ^ "Diffuse Intrinsic Pontine Glioma (DIPG)". St Jude Children's Research Hospital.
- ^ Fisher PG, Monje M (10 May 2010). "Brain Stem Gliomas in Childhood". Germantown, Maryland: Childhood Brain Tumor Foundation.
- ^ Fisher PG, Breiter SN, Carson BS, Wharam MD, Williams JA, Weingart JD, et al. (October 2000). "A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as distinct entities". Cancer. 89 (7): 1569–1576. doi:10.1002/1097-0142(20001001)89:7<1569::aid-cncr22>3.0.co;2-0. PMID 11013373.
- ^ Donaldson SS, Laningham F, Fisher PG (March 2006). "Advances toward an understanding of brainstem gliomas". Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 24 (8): 1266–72. doi:10.1200/JCO.2005.04.6599. PMID 16525181.
- ^ Korones DN (May 2007). "Treatment of newly diagnosed diffuse brain stem gliomas in children: in search of the holy grail". Expert Review of Anticancer Therapy. 7 (5): 663–74. doi:10.1586/14737140.7.5.663. PMID 17492930.
- ^ a b c "Recurrence/Relapse – DIPG Registry". Archived from the original on 9 April 2015. Retrieved 20 December 2018.
- ^ "Getting into the brain: approaches to enhance brain drug delivery". Just One More Day. Archived from the original on 1 July 2012.
- ^ a b Patel MM, Goyal BR, Bhadada SV, Bhatt JS, Amin AF (2009). "Getting into the brain: approaches to enhance brain drug delivery". CNS Drugs. 23 (1): 35–58. doi:10.2165/0023210-200923010-00003. PMID 19062774.
- ^ "MOA Video". Archived from the original on 2010-05-05. Retrieved 2015-04-13.
- ^ Hall WA, Doolittle ND, Daman M, Bruns PK, Muldoon L, Fortin D, Neuwelt EA (May 2006). "Osmotic blood-brain barrier disruption chemotherapy for diffuse pontine gliomas". Journal of Neuro-oncology. 77 (3): 279–84. doi:10.1007/s11060-005-9038-4. PMID 16314949.
- ^ Lonser RR, Warren KE, Butman JA, Quezado Z, Robison RA, Walbridge S, et al. (July 2007). "Real-time image-guided direct convective perfusion of intrinsic brainstem lesions. Technical note". Journal of Neurosurgery. 107 (1): 190–197. doi:10.3171/JNS-07/07/0190. PMID 17639894.
- ^ Hansen JR (2005). First Man: The Life of Neil A. Armstrong. New York: Simon & Schuster. pp. 161–164. ISBN 978-0-7432-5631-5. OCLC 937302502.
- ^ "Home". thecurestartsnow.org.
- ^ "Home". notesleftbehind.com.
- ^ Gibson C (14 November 2013). "Federal pediatric medical research act named for Gabriella Miller". The Washington Post. Retrieved 3 February 2021.
- ^ "Our Story". Smashing Walnuts Foundation. Retrieved 3 February 2021.
- ^ "Cure Starts Now reaches $2.2M goal in honor of Lauren Hill". Local 12. January 2016. Retrieved 2021-05-03.
- ^ Cannonballs For Kayne Foundation. Support Research. A DIPG Research Foundation
