Anterior longitudinal ligament
| Anterior longitudinal ligament | |
|---|---|
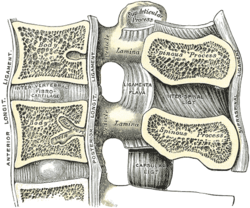 Median sagittal section of two lumbar vertebræ and their ligaments. (Anterior longitudinal ligament runs vertically at center left.) | |
 Anterior atlantooccipital membrane and atlantoaxial ligament. (Anterior longitudinal ligament runs vertically at bottom center.) | |
| Details | |
| System | skeletal |
| From | inferior basilar portion of occipital bone |
| To | sacrum |
| Identifiers | |
| Latin | ligamentum longitudinale anterius |
| TA98 | A03.2.01.007 |
| TA2 | 1679 |
| FMA | 31893 |
| Anatomical terminology | |
The anterior longitudinal ligament is a ligament that extends across the anterior/ventral aspect of the vertebral bodies and intervertebral discs the spine.
It may be partially cut to treat certain abnormal curvatures in the vertebral column, such as kyphosis.
Anatomy
[edit]The anterior longitudinal ligament extends superoinferiorly between the basiocciput of the skull and the anterior tubercle of the atlas (cervical certebra C1) superiorly, and the superior part of the sacrum inferiorly;[1] inferiorly, it ends at the sacral promontory.[2] It broadens inferiorly.[1] Inferiorly, it becomes continuous with the anterior sacrococcygeal ligament.[3] Superiorly, between the skull and atlas, the ligament is continuous laterally with the anterior atlantooccipital membrane.[4]
The ligament is thick and slightly more narrow over the vertebral bodies and thinner but slightly wider over the intervertebral discs.[5]
It tends to be narrower and thicker around thoracic vertebrae, and wider and thinner around cervical vertebrae and lumbar vertebrae.[5]
Structure
[edit]The anterior longitudinal ligament adheres strongly to the periosteum of the vertebral bodies, but is less strongly connected with the intervertebral discs.[1]
It has three layers: superficial, intermediate and deep. The superficial layer traverses 3 – 4 vertebrae, the intermediate layer covers 2 – 3 and the deep layer is only between individual vertebrae.[citation needed]
Clinical significance
[edit]The anterior longitudinal ligament may become calcified, causing back pain.[6]
Surgical release
[edit]The anterior longitudinal ligament may be "released", or partially cut, between two adjacent vertebrae.[7] This may be done to treat abnormal curvature in the vertebral column, such as kyphosis.[7] Osteoporosis, some infections, and past back surgery may prevent this surgery.[7]
Additional images
[edit]-
E:Anterior longitudinal ligament
-
Median sagittal section through the occipital bone and first three cervical vertebræ.
-
Costovertebral articulations. Anterior view.
See also
[edit]References
[edit]- ^ a b c Sinnatamby C (2011). Last's Anatomy (12th ed.). p. 424. ISBN 978-0-7295-3752-0.
- ^ Kadasne, D. K. (2009). Kadasne's Textbook of Anatomy (1st ed.). New Delhi: Jaypee Brothers Medical Publishers. p. 371. ISBN 978-81-8448-455-7. OCLC 682534511.
- ^ "anterior sacrococcygeal ligament". TheFreeDictionary.com. Retrieved 2023-06-08.
- ^ Moore, Keith L.; Dalley, Arthur F.; Agur, Anne M. R. (2018). Clinically Oriented Anatomy (8th ed.). Wolters Kluwer. p. 99. ISBN 978-1-4963-4721-3.
- ^ a b Kayalioglu, Gulgun (2009). "3 - The Vertebral Column and Spinal Meninges". The spinal cord : a Christopher and Dana Reeve Foundation text and atlas (1st ed.). Amsterdam: Elsevier / Academic Press. pp. 17–36. doi:10.1016/B978-0-12-374247-6.50007-9. ISBN 978-0-08-092138-9. OCLC 500570905.
- ^ Giles, Lynton G. F. (2009). "Case 92 - Post-traumatic anterior longitudinal ligament calcification". 100 challenging spinal pain syndrome cases (2nd ed.). Edinburgh: Elsevier / Churchill Livingstone. pp. 425–427. doi:10.1016/B978-0-443-06716-7.00092-X. ISBN 978-0-7020-4271-3. OCLC 460883276.
- ^ a b c Sardar, Zeeshan M.; Baron, Eli M.; Davis, Timothy; Anand, Neel (2018). "Procedure 41 - The Transpsoas Approach for Thoracolumbar Interbody Fusion". Operative Techniques: Spine surgery (3rd ed.). Philadelphia: Elsevier. pp. 358–370. doi:10.1016/B978-0-323-40066-4.00041-2. ISBN 978-0-323-48391-9. OCLC 964627490.
External links
[edit]- Atlas image: back_bone25 at the University of Michigan Health System - "Vertebral Column, Dissection, Anterior & Posterior Views"
- lesson7 at The Anatomy Lesson by Wesley Norman (Georgetown University)
- Diagram at spineuniverse.com



