Clinical trial
In health care, a clinical trial is a comparison test of a medication or other medical treatment (such as a medical device), versus a placebo (inactive look-a-like), other medications or devices, or the standard medical treatment for a patient's condition. Clinical trials vary greatly in size: from a single researcher in one hospital or clinic to an international multicenter study with several hundred participating researchers on several continents. The number of patients tested can range from as few as 30 to several thousands.
In a clinical trial, the investigator first identifies the medication or device to be tested. Then the investigator decides what to compare it with (one or more existing treatments or a placebo), and what kind of patients might benefit from the medication/device. If the investigator cannot obtain enough patients with this specific disease or condition at his or her own location, then he or she assembles investigators at other locations who can obtain the same kind of patients to receive the treatment. During the clinical trial, the investigators: recruit patients with the predetermined characteristics, administer the treatment(s), and collect data on the patients' health for a defined time period. (These data include things like vital signs, amount of study drug in the blood, and whether the patient's health gets better or not.) The researchers send the data to the trial sponsor, who then analyzes the pooled data using statistical tests.
Some examples of what a clinical trial may be designed to do:
- assess the safety and effectiveness of a new medication or device on a specific kind of patient (e.g., patients who have been diagnosed with Alzheimer's disease for less than one year)
- assess the safety and effectiveness of a different dose of a medication than is commonly used (e.g., 10 mg dose instead of 5 mg dose)
- assess the safety and effectiveness of an already marketed medication or device on a new kind of patient (who is not yet approved by regulatory authorities to be given the medication or device)
- assess whether the new medication or device is more effective for the patient's condition than the already used, standard medication or device ("the gold standard" or "standard therapy")
- compare the effectiveness in patients with a specific disease of two or more already approved or common interventions for that disease (e.g., Device A vs. Device B, Therapy A vs. Therapy B)
Note that while most clinical trials compare two medications or devices, some trials compare three or four medications, doses of medications, or devices against each other.
Except for very small trials limited to a single location, the clinical trial design and objectives are written into a document called a clinical trial protocol. The protocol is the 'operating manual' for the clinical trial, and ensures that researchers in different locations all perform the trial in the same way on patients with the same characteristics. (This uniformity is designed to allow the data to be pooled.) A protocol is always used in multicenter trials.
Because the researchers test hypotheses and observe what happens, clinical trials can be seen as the application of the scientific method to understanding human or animal biology.
Synonyms for 'clinical trials' include clinical studies, research protocols and medical research.
The most commonly performed clinical trials evaluate new drugs, medical devices (like a new catheter), biologics, psychological therapies, or other interventions. Clinical trials may be required before the national regulatory authority[1] will approve marketing of the drug or device, or a new dose of the drug, for use on patients.
History
Clinical trials were first introduced in Avicenna's The Canon of Medicine in the 1020s, in which he laid down rules for the experimental use and testing of drugs and wrote a precise guide for practical experimentation in the process of discovering and proving the effectiveness of medical drugs and substances.[2] He laid out the following rules and principles for testing the effectiveness of new drugs and medications, which still form the basis of modern clinical trials:[3][4]
- "The drug must be free from any extraneous accidental quality."
- "It must be used on a simple, not a composite, disease."
- "The drug must be tested with two contrary types of diseases, because sometimes a drug cures one disease by Its essential qualities and another by its accidental ones."
- "The quality of the drug must correspond to the strength of the disease. For example, there are some drugs whose heat is less than the coldness of certain diseases, so that they would have no effect on them."
- "The time of action must be observed, so that essence and accident are not confused."
- "The effect of the drug must be seen to occur constantly or in many cases, for if this did not happen, it was an accidental effect."
- "The experimentation must be done with the human body, for testing a drug on a lion or a horse might not prove anything about its effect on man."
One of the most famous clinical trials was James Lind's demonstration in 1754 that citrus fruits cure scurvy.[5] He compared the effects of various different acidic substances, ranging from vinegar to cider, on groups of afflicted sailors, and found that the group who were given oranges and lemons had largely recovered from scurvy after 6 days.
Types
One way of classifying clinical trials is by the way the researchers behave.
- In an observational study, the investigators observe the subjects and measure their outcomes. The researchers do not actively manage the experiment. This is also called a natural experiment). An example is the Nurses' Health Study.
- In an interventional study, the investigators give the research subjects a particular medicine or other intervention. (Usually they compare the treated subjects to subjects who receive no treatment or standard treatment.) Then the researchers measure how the subjects' health changes.
Another way of classifying trials is by their purpose. The U.S. National Institutes of Health (NIH) organizes trials into five (5) different types:
- Treatment trials: test experimental treatments, new combinations of drugs, or new approaches to surgery or radiation therapy.
- Prevention trials: look for better ways to prevent disease in people who have never had the disease or to prevent a disease from returning. These approaches may include medicines, vitamins, vaccines, minerals, or lifestyle changes.
- Diagnostic trials: conducted to find better tests or procedures for diagnosing a particular disease or condition.
- Screening trials: test the best way to detect certain diseases or health conditions.
- Quality of Life: trials (or Supportive Care trials) explore ways to improve comfort and the quality of life for individuals with a chronic illness.
Design
A fundamental distinction in evidence-based medicine is between observational studies and randomized controlled trials. Types of observational studies in epidemiology such as the cohort study and the case-control study provide less compelling evidence than the randomized controlled trial. In observational studies, the investigators only observe associations (correlations) between the treatments experienced by participants and their health status or diseases.
A randomized controlled trial is the study design that can provide the most compelling evidence that the study treatment causes the expected effect on human health.
Currently, some Phase II and most Phase III drug trials are designed as randomized, double blind, and placebo-controlled.
- Randomized: Each study subject is randomly assigned to receive either the study treatment or a placebo.
- Blind: The subjects involved in the study do not know which study treatment they receive. If the study is double-blind, the researchers also do not know which treatment is being given to any given subject. This 'blinding' is to prevent biases, since if a physician knew which patient was getting the study treatment and which patient was getting the placebo, he/she might be tempted to give the (presumably helpful) study drug to a patient who could more easily benefit from it. In addition, a physician might give extra care to only the patients who receive the placebos to compensate for their ineffectiveness. A form of double-blind study called a "double-dummy" design allows additional insurance against bias or placebo effect. In this kind of study, all patients are given both placebo and active doses in alternating periods of time during the study.
- Placebo-controlled: The use of a placebo (fake treatment) allows the researchers to isolate the effect of the study treatment.
Of note, during the last ten years or so it has become a common practice to conduct "active comparator" studies (also known as "active control" trials). In other words, when a treatment exists that is clearly better than doing nothing for the subject (i.e. giving them the placebo), the alternate treatment would be a standard-of-care therapy. The study would compare the 'test' treatment to standard-of-care therapy.
Although the term "clinical trials" is most commonly associated with large, randomized studies, many clinical trials are small. They may be "sponsored" by single physicians or a small group of physicians, and are designed to test simple questions. Other clinical trials require large numbers of participants (who may be followed over long periods of time), and the trial sponsor is a private company, a government health agency, or an academic research body such as a university.
In designing a clinical trial, a sponsor must decide on the target number of patients who will participate. The sponsor's goal usually is to obtain a statistically significant result showing a significant difference in outcome (e.g., number of deaths after 28 days in the study) between the groups of patients who receive the study treatments. The number of patients required to give a statistically significant result depends on the question the trial wants to answer. (For example, to show the effectiveness of a new drug in a non-curable disease as metastatic kidney cancer requires many fewer patients than in a highly curable disease as seminoma).
The number of patients enrolled in a study has a large bearing on the ability of the study to reliably detect the size of the effect of the study intervention. This is described as the "power" of the trial. The larger the sample size or number of participants in the trial, the greater the statistical power. However, in designing a clinical trial, this consideration must be balanced with the fact that more patients make for a more expensive trial.[6]
Phases
Clinical trials involving new drugs are commonly classified into four phases.Each phase of the drug approval process is treated as a separate clinical trial. The drug-development process will normally proceed through all four phases over many years. If the drug successfully passes through Phases I, II, and III, it will usually be approved by the national regulatory authority for use in the general population. Phase IV are 'post-approval' studies.
Before pharmaceutical companies start clinical trials on a drug, they conduct extensive pre-clinical studies.
Pre-clinical studies
Pre-clinical studies involve in vitro (i.e., test tube or laboratory) studies and trials on animal populations. Wide-ranging dosages of the study drug are given to the animal subjects or to an in-vitro substrate in order to obtain preliminary efficacy, toxicity and pharmacokinetic information and to assist pharmaceutical companies in deciding whether it is worthwhile to go ahead with further testing.
Phase 0
Phase 0 is a recent designation for exploratory, first-in-human trials conducted in accordance with the U.S. Food and Drug Administration’s (FDA) 2006 Guidance on Exploratory Investigational New Drug (IND) Studies.[7] Phase 0 trials are designed to speed up the development of promising drugs or imaging agents by establishing very early on whether the drug or agent behaves in human subjects as was anticipated from preclinical studies. Distinctive features of Phase 0 trials include the administration of single subtherapeutic doses of the study drug to a small number of subjects (10 to 15) to gather preliminary data on the agent's pharmacokinetics (how the body processes the drug) and pharmacodynamics (how the drug works in the body).
Phase I
Phase I trials are the first stage of testing in human subjects. Normally, a small (20-80) group of healthy volunteers will be selected. This phase includes trials designed to assess the safety (pharmacovigilance), tolerability, pharmacokinetics, and pharmacodynamics of a drug. These trials are often conducted in an inpatient clinic, where the subject can be observed by full-time staff. The subject who receives the drug is usually observed until several half-lives of the drug have passed. Phase I trials also normally include dose-ranging, also called dose escalation, studies so that the appropriate dose for therapeutic use can be found. The tested range of doses will usually be a fraction of the dose that causes harm in animal testing. Phase I trials most often include healthy volunteers. However, there are some circumstances when real patients are used, such as patients who have end-stage disease and lack other treatment options. This exception to the rule most often occurs in oncology (cancer) and HIV drug trials.
There are different kinds of Phase I trials:
- SAD
- Single Ascending Dose studies are those in which small groups of patients are given a single dose of the drug while they are observed and tested for a period of time. If they do not exhibit any adverse side effects, and the pharmacokinetic data is roughly in line with predicted safe values, the dose is escalated, and a new group of patients is then given a higher dose. This is continued until pre-calculated pharmacokinetic safety levels are reached, or intolerable side effects start showing up (at which point the drug is said to have reached the Maximum tolerated dose (MTD).
- MAD
- Multiple Ascending Dose studies are conducted to better understand the pharmacokinetics & pharmacodynamics of multiple doses of the drug. In these studies, a group of patients receives multiple low doses of the drug, whilst samples (of blood, and other fluids) are collected at various time points and analyzed to understand how the drug is processed within the body. The dose is subsequently escalated for further groups, up to a predetermined level.
- Food effect
- a short trial designed to investigate any differences in absorption of the drug by the body, caused by eating before the drug is given. These studies are usually run as a crossover study, with volunteers being given two identical doses of the drug on different occasions; one while fasted, and one after being fed.
Phase II
Once the initial safety of the study drug has been confirmed in Phase I trials, Phase II trials are performed on larger groups (20-300) and are designed to assess how well the drug works, as well as to continue Phase I safety assessments in a larger group of volunteers and patients. When the development process for a new drug fails, this usually occurs during Phase II trials when the drug is discovered not to work as planned, or to have toxic effects.
Phase II studies are sometimes divided into Phase IIA and Phase IIB. Phase IIA is specifically designed to assess dosing requirements (how much drug should be given), whereas Phase IIB is specifically designed to study efficacy (how well the drug works at the prescribed dose(s)).
Some trials combine Phase I and Phase II, and test both efficacy and toxicity.
Trial design
Some Phase II trials are designed as case series, demonstrating a drug's safety and activity in a selected group of patients. Other Phase II trials are designed as randomized clinical trials, where some patients receive the drug/device and others receive placebo/standard treatment. Randomized Phase II trials have far fewer patients than randomized Phase III trials.
Phase III
Phase III studies are randomized controlled multicenter trials on large patient groups (300–3,000 or more depending upon the disease/medical condition studied) and are aimed at being the definitive assessment of how effective the drug is, in comparison with current 'gold standard' treatment. Because of their size and comparatively long duration, Phase III trials are the most expensive, time-consuming and difficult trials to design and run, especially in therapies for chronic medical conditions.
It is common practice that certain Phase III trials will continue while the regulatory submission is pending at the appropriate regulatory agency. This allows patients to continue to receive possibly lifesaving drugs until the drug can be obtained by purchase. Other reasons for performing trials at this stage include attempts by the sponsor at "label expansion" (to show the drug works for additional types of patients/diseases beyond the original use for which the drug was approved for marketing), to obtain additional safety data, or to support marketing claims for the drug. Studies in this phase are by some companies categorised as "Phase IIIB studies."[8][9]
While not required in all studies, it is typically expected that there be at least two successful Phase III trials, demonstrating a drug's safety and efficacy, in order to obtain approval from the appropriate regulatory agencies (FDA (USA), TGA (Australia), EMEA (European Union), etc.).
Once a drug has proved satisfactory after Phase III trials, the trial results are usually combined into a large document containing a comprehensive description of the methods and results of human and animal studies, manufacturing procedures, formulation details, and shelf life. This collection of information makes up the "regulatory submission" that is provided for review to the appropriate regulatory authorities[1] in different countries. They will review the submission, and, it is hoped, give the sponsor approval to market the drug.
Most drugs undergoing Phase III clinical trials can be marketed under FDA norms with proper recommendations and guidelines, but in case of any adverse effects being reported anywhere, the drugs need to be recalled immediately from the market. While most pharmaceutical companies refrain from this practice, it is not abnormal to see many drugs undergoing Phase III clinical trials in the market.[citation needed]
Phase IV
Phase IV trials involve the safety surveillance (pharmacovigilance) and ongoing technical support of a drug after it receives permission to be sold. Phase IV studies may be required by regulatory authorities or may be undertaken by the sponsoring company for competitive (finding a new market for the drug) or other reasons (for example, the drug may not have been tested for interactions with other drugs, or on certain population groups such as pregnant women, who are unlikely to subject themselves to trials). The safety surveillance is designed to detect any rare or long-term adverse effects over a much larger patient population and longer time period than was possible during the Phase I-III clinical trials. Harmful effects discovered by Phase IV trials may result in a drug being no longer sold, or restricted to certain uses: recent examples include cerivastatin (brand names Baycol and Lipobay), troglitazone (Rezulin) and rofecoxib (Vioxx).
Length
Clinical trials are only a small part of the research that goes into developing a new treatment. Potential drugs, for example, first have to be discovered, purified, characterized, and tested in labs (in cell and animal studies) before ever undergoing clinical trials. In all, about 1,000 potential drugs are tested before just one reaches the point of being tested in a clinical trial. For example, a new cancer drug has, on average, at least 6 years of research behind it before it even makes it to clinical trials. But the major holdup in making new cancer drugs available is the time it takes to complete clinical trials themselves. On average, about 8 years pass from the time a cancer drug enters clinical trials until it receives approval from regulatory agencies for sale to the public. Drugs for other diseases have similar timelines.
Some reasons a clinical trial might last several years:
- For chronic conditions like cancer, it takes months, if not years, to see if a cancer treatment has an effect on a patient.
- For drugs that are not expected to have a strong effect (meaning a large number of patients must be recruited to observe any effect), recruiting enough patients to test the drug's effectiveness (i.e., getting statistical power) can take several years.
- Only certain people who have the target disease condition are eligible to take part in each clinical trial. Researchers who treat these particular patients must participate in the trial. Then they must identify the desirable patients and obtain consent from them or their families to take part in the trial.
The biggest barrier to completing studies is the shortage of people who take part. All drug and many device trials target a subset of the population, meaning not everyone can participate. Some drug trials require patients to have unusual combinations of disease characteristics. It is a challenge to find the appropriate patients and obtain their consent, especially when they may receive no direct benefit (because they are not paid, the study drug is not yet proven to work, or the patient may receive a placebo). In the case of cancer patients, fewer than 5% of adults with cancer will participate in drug trials. According to the Pharmaceutical Research and Manufacturers of America (PhRMA), about 400 cancer medicines were being tested in clinical trials in 2005. Not all of these will prove to be useful, but those that are may be delayed in getting approved because the number of participants is so low.[10]
Clinical trials that do not involve a new drug usually have a much shorter duration. (Exceptions are epidemiological studies like the Nurses' Health Study.)
Administration
Clinical trials designed by a local investigator and (in the U.S.) federally funded clinical trials are almost always administered by the researcher who designed the study and applied for the grant. Small-scale device studies may be administered by the sponsoring company. Phase III and Phase IV clinical trials of new drugs are usually administered by a contract research organization (CRO) hired by the sponsoring company. (The sponsor provides the drug and medical oversight.) A CRO is a company that is contracted to perform all the administrative work on a clinical trial. It recruits participating researchers, trains them, provides them with supplies, coordinates study administration and data collection, sets up meetings, monitors the sites for compliance with the clinical protocol, and ensures that the sponsor receives 'clean' data from every site. Recently, site management organizations have also been hired to coordinate with the CRO to ensure rapid IRB/IEC approval and faster site initiation and patient recruitment.
At a participating site, one or more research assistants (often nurses) do most of the work in conducting the clinical trial. The research assistant's job can include some or all of the following: providing the local Institutional Review Board (IRB) with the documentation necessary to obtain its permission to conduct the study, assisting with study start-up, identifying eligible patients, obtaining consent from them or their families, administering study treatment(s), collecting data, maintaining data files, and communicating with the IRB, as well as the sponsor (if any) and CRO (if any).
Ethical conduct
Clinical trials are closely supervised by appropriate regulatory authorities. All studies that involve a medical or therapeutic intervention on patients must be approved by a supervising ethics committee before permission is granted to run the trial. The local ethics committee has discretion on how it will supervise noninterventional studies (observational studies or those using already collected data). In the U.S., this body is called the Institutional Review Board (IRB). Most IRBs are located at the local investigator's hospital or institution, but some sponsors allow the use of a central (independent/for profit) IRB for investigators who work at smaller institutions.
To be ethical, researchers must obtain the full and informed consent of participating human subjects. (One of the IRB's main functions is ensuring that potential patients are adequately informed about the clinical trial.) If the patient is unable to consent for him/herself, researchers can seek consent from the patient's legally authorized representative. In California, the state has prioritized the individuals who can serve as the legally authorized representative.
In some U.S. locations, the local IRB must certify researchers and their staff before they can conduct clinical trials. They must understand the federal patient privacy (HIPAA) law and good clinical practice. International Conference of Harmonisation Guidelines for Good Clinical Practice (ICH GCP) is a set of standards used internationally for the conduct of clinical trials. The guidelines aim to ensure that the "rights, safety and well being of trial subjects are protected".
Safety
Responsibility for the safety of the subjects in a clinical trial is shared between the sponsor, the local site investigators (if different from the sponsor), the various IRBs that supervise the study, and (in some cases, if the study involves a marketable drug or device) the regulatory agency for the country where the drug or device will be sold.
Sponsor
- For safety reasons, many clinical trials of drugs are designed to exclude women of childbearing age, pregnant women, and/or women who become pregnant during the study. In some cases the male partners of these women are also excluded or required to take birth control measures.
- Throughout the clinical trial, the sponsor is responsible for accurately informing the local site investigators of the true historical safety record of the drug, device or other medical treatments to be tested, and of any potential interactions of the study treatment(s) with already approved medical treatments. This allows the local investigators to make an informed judgment on whether to participate in the study or not.
- The sponsor is responsible for monitoring the results of the study as they come in from the various sites, as the trial proceeds. In larger clinical trials, a sponsor will use the services of a Data Monitoring Committee (DMC, known in the U.S. as a Data Safety Monitoring Board). This is an independent group of clinicians and statisticians. The DMC meets periodically to review the unblinded data that the sponsor has received so far. The DMC has the power to recommend termination of the study based on their review, for example if the study treatment is causing more deaths than the standard treatment, or seems to be causing unexpected and study-related serious adverse events.
- The sponsor is responsible for collecting adverse event reports from all site investigators in the study, and for informing all the investigators of the sponsor's judgment as to whether these adverse events were related or not related to the study treatment. This is an area where sponsors can slant their judgment to favor the study treatment.
- The sponsor and the local site investigators are jointly responsible for writing a site-specific informed consent that accurately informs the potential subjects of the true risks and potential benefits of participating in the study, while at the same time presenting the material as briefly as possible and in ordinary language.
Local site investigators
- A physician's first duty is to his/her patients, and if a physician investigator believes that the study treatment may be harming subjects in the study, the investigator can stop participating at any time. On the other hand, investigators often have a financial interest in recruiting subjects, and can act unethically in order to obtain and maintain their participation.
- The local investigators are responsible for conducting the study according to the study protocol, and supervising the study staff throughout the duration of the study.
- The local investigator or his/her study staff are responsible for ensuring that potential subjects in the study understand the risks and potential benefits of participating in the study; in other words, that they (or their legally authorized representatives) give truly informed consent.
- The local investigators are responsible for reviewing all adverse event reports sent by the sponsor. (These adverse event reports contain the opinion of both the investigator at the site where the adverse event occurred, and the sponsor, regarding the relationship of the adverse event to the study treatments). The local investigators are responsible for making an independent judgment of these reports, and promptly informing the local IRB of all serious and study-treatment-related adverse events.
- When a local investigator is the sponsor, there may not be formal adverse event reports, but study staff at all locations are responsible for informing the coordinating investigator of anything unexpected.
- The local investigator is responsible for being truthful to the local IRB in all communications relating to the study.
IRBs
Approval by an IRB, or ethics board, is necessary before all but the most informal medical research can begin.
- In commercial clinical trials, the study protocol is not approved by an IRB before the sponsor recruits sites to conduct the trial. However, the study protocol and procedures have been tailored to fit generic IRB submission requirements. In this case, and where there is no independent sponsor, each local site investigator submits the study protocol, the consent(s), the data collection forms, and supporting documentation to the local IRB. Universities and most hospitals have in-house IRBs. Other researchers (such as in walk-in clinics) use independent IRBs.
- The IRB scrutinizes the study for both medical safety and protection of the patients involved in the study, before it allows the researcher to begin the study. It may require changes in study procedures or in the explanations given to the patient. A required yearly "continuing review" report from the investigator updates the IRB on the progress of the study and any new safety information related to the study.
Regulatory agencies
- If a clinical trial concerns a regulated drug or medical device, the appropriate regulatory agency for the country where the trial is conducted is supposed to review all study data before allowing the drug/device to proceed to the next phase, or to be marketed. However, if the sponsor withholds negative data, or misrepresents data it has acquired from clinical trials, the regulatory agency may make the wrong decision.
- In the U.S., the FDA can audit the files of local site investigators after they have finished participating in a study, to see if they were correctly following study procedures. This audit may be random, or for cause (because the investigator is suspected of fraudulent data). Avoiding an audit is an incentive for investigators to follow study procedures.
Accidents
In March 2006 the drug TGN1412 caused catastrophic systemic failure in the individuals receiving the drug during its first human clinical trials (Phase I) in Great Britain. Following this, an Expert Group on Phase One Clinical Trials published a report.[11]
Economics
Sponsor
The cost of a study depends on many factors, especially the number of sites that are conducting the study, the number of patients required, and whether the study treatment is already approved for medical use. Clinical trials follow a standardized process.
The costs to a pharmaceutical company of administering a Phase III or IV clinical trial may include, among others:
- manufacturing the drug(s)/device(s) tested
- staff salaries for the designers and administrators of the trial
- payments to the contract research organization, the site management organization (if used) and any outside consultants
- payments to local researchers (and their staffs) for their time and effort in recruiting patients and collecting data for the sponsor
- study materials and shipping
- communication with the local researchers, including onsite monitoring by the CRO before and (in some cases) multiple times during the study
- one or more investigator training meetings
- costs incurred by the local researchers such as pharmacy fees, IRB fees and postage.
- any payments to patients enrolled in the trial (all payments are strictly overseen by the IRBs to ensure that patients do not feel coerced to take part in the trial by overly attractive payments)
These costs are incurred over several years.
In the U.S. there is a 50% tax credit for sponsors of certain clinical trials.[12]
National health agencies such as the U.S. National Institutes of Health offer grants to investigators who design clinical trials that attempt to answer research questions that interest the agency. In these cases, the investigator who writes the grant and administers the study acts as the sponsor, and coordinates data collection from any other sites. These other sites may or may not be paid for participating in the study, depending on the amount of the grant and the amount of effort expected from them.
Investigators
Many clinical trials do not involve any money. However, when the sponsor is a private company or a national health agency, investigators are almost always paid to participate. These amounts can be small, just covering a partial salary for research assistants and the cost of any supplies (usually the case with national health agency studies), or be substantial and include 'overhead' that allows the investigator to pay the research staff during times in between clinical trials.
Patients
In Phase I drug trials, participants are paid because they give up their time (sometimes away from their homes) and are exposed to unknown risks, without the expectation of any benefit. In most other trials, however, patients are not paid, in order to ensure that their motivation for participating is the hope of getting better or contributing to medical knowledge, without their judgment being skewed by financial considerations. However, they are often given small reimbursements for study-related expenses like travel.
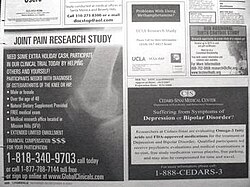
Acquiring participants
Phase 0 and Phase I drug trials seek healthy volunteers. Most other clinical trials seek patients who have a specific disease or medical condition. Depending on the kind of participants required, sponsors use various recruitment strategies, including patient databases, newspaper and radio advertisements, flyers, posters in places the patients might go (such as doctor's offices), and personal conversations with the investigator. Various resources are available for individuals who want to participate in a clinical trial. A patient may ask their physician about clinical trials available for their condition or contact other clinics directly. The US government, World Health Organization and commercial organizations provide online clinical trial resources.
See also
- Fermish Clinical Technologies Pvt. Ltd
- Clinical Trials in India
- Clinical Research Organization
- Academic clinical trials
- CIOMS Guidelines
- Clinical trial management
- Clinical data acquisition
- Clinical Data Interchange Standards Consortium
- Clinical site
- Community-based clinical trial
- Contract Research Organization
- Data Monitoring Committees
- Drug development
- European Medicines Agency
- FDA Special Protocol Assessment
- IFPMA
- Investigational Device Exemption
- Interactive voice response
- Medical ethics
- Nocebo
- Orphan drug
- Randomized controlled trial
- Remote Data Entry
- World Medical Association
Notes
- ^ a b The regulatory authority in the USA is the Food and Drug Administration; in Canada, Health Canada; in the EU, the European Medicines Agency; in Japan, the Ministry of Health, Labour and Welfare; the Health Sciences Authority (HSA) in Singapore.
- ^ Toby E. Huff (2003), The Rise of Early Modern Science: Islam, China, and the West, p. 218. Cambridge University Press, ISBN 0521529948.
- ^ David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", Heart Views 4 (2).
- ^ D. Craig Brater and Walter J. Daly (2000), "Clinical pharmacology in the Middle Ages: Principles that presage the 21st century", Clinical Pharmacology & Therapeutics 67 (5), p. 447-450 [448].
- ^ "James Lind: A Treatise of the Scurvy (1754)". 2001. Retrieved 2007-09-09.
{{cite web}}: Check date values in:|date=(help) - ^ The power of a trial is not a single, unique value; it estimates the ability of a trial to detect a difference of a particular size (or larger) between the treated (tested drug/device) and control (placebo or standard treatment) groups. For example, a trial of a lipid-lowering drug versus placebo with 100 patients in each group might have a power of .90 to detect a difference between patients receiving study drug and patients receiving placebo of 10 mg/dL or more, but only have a power of .70 to detect a difference of 5 mg/dL.
- ^ "Guidance for Industry, Investigators, and Reviewers Exploratory IND Studies". Food and Drug Administration. January 2006. Retrieved 2007-05-01.
- ^ "Guidance for Institutional Review Boards and Clinical Investigators". FDA. 1999-03-16. Retrieved 2007-03-27.
{{cite web}}: Check date values in:|date=(help) - ^ "Periapproval Services (Phase IIIb and IV programs)". Covance Inc. 2005. Retrieved 2007-03-27.
- ^ Web Site Editor (2007). "Clinical Trials - What Your Need to Know". American Cancer Society.
{{cite journal}}:|author=has generic name (help) - ^ Expert Group on Phase One Clinical Trials (Chairman: Professor Gordon W. Duff) (2006-12-07). "Expert Group on Phase One Clinical Trials: Final report". The Stationery Office. Retrieved 2007-05-24.
{{cite web}}: Check date values in:|date=(help) - ^ "Tax Credit for Testing Expenses for Drugs for Rare Diseases or Conditions". FDA. 2001-04-17. Retrieved 2007-03-27.
{{cite web}}: Check date values in:|date=(help)
References
- Rang HP, Dale MM, Ritter JM, Moore PK (2003). Pharmacology 5 ed. Edinburgh: Churchill Livingstone. ISBN 0-443-07145-4
- Finn R, (1999). Cancer Clinical Trials: Experimental Treatments and How They Can Help You., Sebastopol: O'Reilly & Associates. ISBN 1-56592-566-1
- Chow S-C and Liu JP (2004). Design and Analysis of Clinical Trials : Concepts and Methodologies, ISBN 0-471-24985-8
- Pocock SJ (2004), Clinical Trials: A Practical Approach, John Wiley & Sons, ISBN 0-471-90155-5
