Pulmonary alveolus
This article needs additional citations for verification. (December 2007) |

An alveolus (plural: alveoli, from Latin alveolus, "little cavity") is an anatomical structure that has the form of a hollow cavity. Found in the lung, the pulmonary alveoli are spherical outcroppings of the respiratory bronchioles and are the primary sites of gas exchange with the blood. Alveoli are particular to mammalian lungs. Different structures are involved in gas exchange in other vertebrates. However, not invertebrates.[1]
Location
The alveoli are found in the respiratory zone of the lungs, providing a total surface area of about 75 m2[2]. The blood brings carbon dioxide from the rest of the body for release into the alveoli, and the oxygen in the alveoli is taken up by the blood in the alveolar blood vessels, to be transported to all the cells in the body.
Anatomy
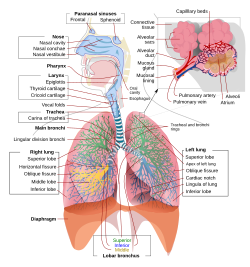
Each human lung contains about 150 million alveoli. Each alveolus is wrapped in a fine mesh of capillaries covering about 70% of its area. An adult alveolus has an average diameter of 0.2-0.3 mm, with an increase in diameter during inhalation.[citation needed]
The alveoli consist of an epithelial layer and extracellular matrix surrounded by capillaries. In some alveolar walls there are pores between alveoli called pores of Kohn.
There are three major alveolar cell types in the alveolar wall (pneumocytes):
- Type I (Squamous Alveolar) cells that form the structure of an alveolar wall
- Type II (Great Alveolar) cells that secrete pulmonary surfactant to lower the surface tension of water and allows the membrane to separate, thereby increasing the capability to exchange gases. Surfactant is continuously released by exocytosis. It forms an underlying aqueous protein-containing hypophase and an overlying phospholipid film composed primarily of dipalmitoyl phosphatidylcholine.
- Macrophages that destroy foreign material, such as bacteria.
Reinflation of the alveoli following exhalation is made easier by pulmonary surfactant, which is a phospholipid and protein mixture that reduces surface tension in the thin fluid coating within all alveoli. The fluid coating is produced by the body in order to facilitate the transfer of gases between blood and alveolar air. The surfactant is produced by great alveolar cells (granular pneumonocytes, a cuboidal epithelia), which are the most numerous cells in the alveoli, yet do not cover as much surface area as the squamous alveolar cells (a squamous epithelium).
Great alveolar cells also repair the endotheilium of the alveolus when it becomes damaged. Insufficient pulmonary surfactant in the alveoli can contribute to atelectasis (collapse of part or all of the lung). Without pulmonary surfactant, atelectasis is a certainty; however, there are other causes of lung collapse such as trauma (pneumothorax), COPD, and pleuritis.[3]
Diseases
- Acute respiratory distress syndrome (ARDS) is a severe inflammatory disease of the lung. Usually triggered by other pulmonary pathology, the uncontrolled inflammation leads to impaired gas exchange, alveolar flooding and/or collapse, and systemic inflammatory response syndrome. It usually requires mechanical ventilation in an intensive care unit setting.
- Infant respiratory distress syndrome (IRDS) is a syndrome caused by lack of surfactant in the lungs of premature infants.
- In asthma, the bronchioles, or the "bottle-necks" into the sac are restricted, causing the amount of air flow into the lungs to be greatly reduced. It can be triggered by irritants in the air, photochemical smog for example, as well as substances that a person is allergic to.
- Emphysema is another disease of the lungs, whereby the elastin in the walls of the alveoli is broken down by an imbalance between the production of neutrophil elastase (elevated by cigarette smoke) and alpha-1-antitrypsin (the activity varies due to genetics or reaction of a critical methionine residue with toxins including cigarette smoke). The resulting loss of elasticity in the lungs leads to prolonged times for exhalation, which occurs through passive recoil of the expanded lung. This leads to a smaller volume of gas exchanged per breath.
- Chronic bronchitis occurs when an abundance of mucus is produced by the lungs. The production of this substance occurs naturally when the lung tissue is exposed to irritants. In chronic bronchitis, the air passages into the alveoli, the broncholiotes, become clogged with mucus. This causes increased coughing in order to remove the mucus, and is often a result of extended periods of exposure to cigarette smoke.
- Cystic fibrosis is a genetic condition caused by the dysfunction of a transmembrane protein responsible for the transport of chloride ions. This causes huge amounts of mucus to clog the bronchiolites, similar to chronic bronchitis. The result is a persistent cough and reduced lung capacity.
- Lung cancer is a common form of cancer causing the uncontrolled growth of cells in the lung tissue. Due to the sensitivity of lung tissue, such malignant growth is often hard to treat effectively.
- Pneumonia is an infection of the alveoli, which can be caused by both viruses and bacteria. Toxins and fluids are released from the virus, causing the effective surface area of the lungs to be greatly reduced. If this happens to such a degree that the patient cannot draw enough oxygen from his environment, then the victim may need supplemental oxygen.
- Cavitary pneumonia is a process in which the alveoli are destroyed and produce a cavity. As the alveoli are destroyed, the surface area for gas exchange to occur becomes reduced. Further changes in blood flow can lead to decline in lung function.
- Pulmonary contusion is a bruise of the lung tissue.
Additional images
-
Bronchial anatomy
-
Microscopic slide
References
- ^ Daniels, Christopher B. and Orgeig, Sandra (2003). "Pulmonary Surfactant: The Key to the Evolution of Air Breathing". News in Physiological Sciences. 18 (4): 151–157.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alveoli: Gas Exchange and Host Defense, ISBN:978-3-211-83564-7 (Print) 978-3-211-26392-1 (Online[1])
- ^ Saladin Anatomy and Physiology: the unity of form and function 4th ed. McGraw Hill, NY,NY 2007
External links
- Pulmonary+Alveoli at the U.S. National Library of Medicine Medical Subject Headings (MeSH)

