Cervical cap
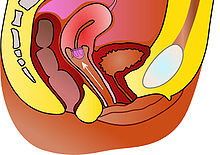
The cervical cap is a form of barrier contraception. A cervical cap fits over the cervix and blocks sperm from entering the uterus through the external orifice of the uterus, called the os.
Terminology
The term cervical cap has been used to refer to a number of barrier contraceptives, including the Prentif, Dumas, Vimule, and Oves devices.[1] In the United States, Prentif was the only brand available for several decades (Prentif was withdrawn from the U.S. market in 2005).[1] During this time, it was common to use the term cervical cap to refer exclusively to the Prentif brand.[2][3]
The Lea's Shield was a cervical barrier device which was discontinued as of 2008. Some sources use cervical cap to refer to the FemCap and Lea's Shield.[4][5] Other sources include FemCap in the term cervical cap, but classified the Lea's Shield as a distinct device.[1][6]
Cervical caps or conception caps have also been designed as a form of assisted reproductive technology, used to help people experiencing infertility.[7]
History
Ancient
The idea of blocking the cervix to prevent pregnancy is thousands of years old. Various cultures have used cervix-shaped devices such as oiled paper cones or lemon halves. Others made sticky mixtures that included honey or cedar rosin, to be applied to the os.[8] The modern idea of a cervical cap as a fitted device that seals itself against the vaginal walls is of more recent origin; it emerged within the past century.
19th century
In 1838, German gynecologist Friedrich Wilde created the first modern cervical cap by making custom-made rubber molds of the cervix for some of his patients.[8] These caps were probably short-lived, as uncured rubber degrades fairly quickly. An important precursor to the invention of more lasting caps was the rubber vulcanization process, patented by Charles Goodyear in 1844. An occlusive pessary marketed in the United States as the "womb veil" seems to have been an early form of diaphragm or cervical cap.[9]
Over the next several decades, the cervical cap became the most widely used barrier contraceptive method in Western Europe and Britain. Although the diaphragm was always more popular in the United States than the cervical cap, the cap was also common.[10]
20th century
Many designs were developed in the later 19th and early 20th century. The Vimule cap became available as early as 1927. A book by Vimule and Co., published in 1898, advertises the Vimule Cap.[11] The Prentif brand cap was introduced in the early 1930s.[12] The Dumas cap was initially made of plastic, and was available by the 1940s.[13] Lamberts (Dalston) Ltd. of the UK manufactured these three cap types.[14] Other types of caps had stems to hold them in place in the cervix; some of the stems actually extended into the uterus. These stem pessaries became precursors to the modern intrauterine device.
Use of all barrier methods, but especially cervical barriers, dropped dramatically after the 1960s introduction of the combined oral contraceptive pill and the intrauterine device. In 1976, the U.S. government enacted the Medical Device Amendment. This law required all manufacturers of medical devices to provide the United States Food and Drug Administration (FDA) with data on the safety and efficacy of those devices. Lamberts (Dalston) Ltd., the only manufacturer at that time, failed to provide this information, and the FDA banned the use of cervical caps in the United States.[10]
In the late 1970s, the FDA reclassified the cervical cap as an investigational device, and it regained limited availability.[15] Within a few years, the FDA withdrew investigational status from the Vimule cap, following a study that associated its use with vaginal lacerations.[10][16] In 1988, the Prentif cap gained FDA approval.[17] The feminist movement played a large role in re-introducing the cervical cap to the United States. One paper called its involvement at all steps of the FDA approval process "unprecedented."[18]
Types

Several brands of caps were manufactured during the late 20th and early 21st centuries. They can be divided into two types: cavity rim caps, and other caps. Cavity rim caps adhere to the cervix, while other caps adhere to the vaginal walls around the cervix.
The cavity rim caps are Prentif, made of latex, and the disposable cap Oves, made of silicone. There are four sizes of Prentif: 22, 25, 28, and 31 mm. There are three sizes of Oves: 26, 28, and 30 mm. Unique among cervical caps, it adheres to the cervix by surface tension, rather than by suction.[1]
The other devices are the latex Dumas and Vimule, and the silicone FemCap, Lea's Shield, and Shanghai Lily. There are five sizes of Dumas: 50, 55, 60, 65, and 75 mm. There are three sizes of Vimule: 42, 48, and 52 mm. There are three sizes of FemCap: 22, 26, and 30 mm. There are four sizes of Shanghai Lily: 54, 58, 62, and 66 mm. Lea's Shield is manufactured in a single size. Unlike the other caps, Lea's Shield has a one-way air valve that helps it seal to the vaginal walls. The valve also allows the passage of cervical mucus. FemCap does not have such a valve and as such can be used to collect cervical mucus to support the billings method.[19] Both Lea's Shield and FemCap have loops to assist in removal.[1]
Shanghai Lily is only available in China.[1] As of 2008, many of the other devices are no longer being manufactured: Prentif, Vimule, and Dumas have been discontinued.[20] Oves is only being sold as a conception cap, not as a birth control device.[citation needed] As of February 2009, FemCap was the only brand of cervical cap available in the United States.[21] FemCap is also available in the UK via the NHS on prescription and is often distributed free from Family Planning Clinics depending on the health authority.[22] Lea's Shield is only available as the German brand LEA contraceptivum.[23]
Fitting
Individuals who wish to use a cervical cap are screened by a health care provider to determine if a cervical cap, or one brand of cap, is appropriate for them. If a cap is determined to be appropriate, the provider will determine the proper size. The user must be refitted after any duration of pregnancy, whether the pregnancy is aborted, miscarried, or carried to term through vaginal childbirth or caesarean section.[24]
Several factors may make a cap inappropriate for a particular woman. Women who have given birth may have scar tissue or irregularly shaped cervixes that interfere with the cap forming a good seal.[25] For some women, available sizes of cervical caps do not provide a correct fit. Also, cavity rim caps are not recommended for women with an anteflexed uterus.[26]
In some countries, some devices (such as the Lea's Shield) are available without a prescription.[27]
Use
The first step in inserting or removing a cervical cap is handwashing, to avoid introducing harmful bacteria into the vaginal canal.[24] The cap is inserted prior to sexual intercourse;[1] some sources state that insertion prior to sexual arousal decreases the risk of incorrect placement.[28] Most sources recommend the use of spermicide with the cap,[1][24][28][29] but some sources say spermicide use is optional.[25][30]
The cap remains in the vagina for a minimum of 6[28][29] - 8[1][30] hours after the last intravaginal ejaculation. It is recommended the cap be removed within 72 hours (within 48 hours is recommended in the U.S.)[1] Other than the disposable Oves cap, cervical caps can be washed and stored for reuse.[4] Silicone devices may be boiled to sterilize them.[31] Reusable caps may last for one[32] or two[24] years.
Effectiveness
The effectiveness of cervical caps, as with most other forms of contraception, can be assessed two ways: method effectiveness and actual effectiveness. The method effectiveness is the proportion of couples correctly and consistently using the method who do not become pregnant. Actual effectiveness is the proportion of couples who intended that method as their sole form of birth control and do not become pregnant; it includes couples who sometimes use the method incorrectly, or sometimes not at all. Rates are generally presented for the first year of use. Most commonly the Pearl Index is used to calculate effectiveness rates, but some studies use decrement tables.
Contraceptive Technology reports that the method failure rate of the Prentif cervical cap with spermicide is 9% per year for nulliparous women (women who have never given birth), and 26% per year for parous women.[2] The actual pregnancy rates among Prentif users vary depending on the population being studied, with yearly rates of 11%[33] to 32%[2] being reported.
Little data is available on the effectiveness of the Oves cap and Femcap. The Oves manufacturer cites one small study of 17 users.[34] The Femcap website does not cite any data on the current version of the Femcap; but lists data for an older version which is no longer approved by the FDA.[32]
The only effectiveness trial of Lea's Shield was too small to determine method effectiveness. The actual pregnancy rate was 15% per year. Of the women in the trial, 85% were parous (had given birth). The study authors estimate that for nulliparous women (those who have never given birth) the pregnancy rate in typical use may be lower, around 5% per year.[35]
Acceptability
The Oves cap and the new version of the Femcap performed poorly in user acceptability studies.[36][37] The study on the Femcap concluded that the modifications to the FemCap significantly increased pain and discomfort among female users and their male sex partners, and that the modifications decreased acceptability of the device compared with the earlier version. The study of the Oves cap reported that few women indicated that they would use the cap in the future.
A pilot study conducted in Britain prior to the Lea's Shield's approval concluded that the Lea's Shield "may be acceptable to a highly select minority of women".[38]
As of 2002, the cervical cap was one of the least common methods of contraception in the United States. A 2002 study indicated that of sexually active American women, 0.6% are currently using either the cervical cap, contraceptive sponge, or female condom as their primary method of contraception, and fewer than 1% have ever used a cervical cap.[39]
References
- ^ a b c d e f g h i j "Cervical Caps". Cervical Barrier Advancement Society. March 2005. Retrieved 2008-04-26. Cite error: The named reference "CBAS" was defined multiple times with different content (see the help page).
- ^ a b c Hatcher, RA; Trussel J; et al. (2000). Contraceptive Technology (18th ed.). New York: Ardent Media. ISBN 0-9664902-6-6.[page needed]
- ^ "FDA Approves Lea's Shield". The Contraception Report. Contraception Online. June 2002. Archived from the original on 2008-04-28. Retrieved 2008-04-26.
- ^ a b "Cervical Cap". Feminist Women's Health Center. September 2006. Retrieved 2008-04-26. Cite error: The named reference "fwhc" was defined multiple times with different content (see the help page).
- ^ "Cervical Cap" (PDF). University of Chicago Student Care Center. 2006. Retrieved 2008-04-26. [dead link]
- ^ "Birth Control Guide". U.S. Food and Drug Administration. December 2003. Retrieved 2008-04-26.
- ^ http://www.fda.gov/cdrh/pdf6/K063227.pdf[permanent dead link]
- ^ a b "A History of Birth Control Methods". Planned Parenthood. June 2002. Archived from the original on May 17, 2008. Retrieved 2006-07-05.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Janet Farrell Brodie, Contraception and Abortion in Nineteenth-Century America (Cornell University Press, 1994), p. 216 online; Andrea Tone, Devices and Desires: A History of Contraceptives in America (MacMillan, 2001), p. 14.
- ^ a b c Weiss, BD; Bassford, T; Davis, T (1991). "The cervical cap". American Family Physician. 43 (2): 517–23. PMID 1990736.
- ^ "the Vimule permanent sheath, as purveyed by Lamberts of London, 1927". Condom pictures. Retrieved 2006-11-12.
- ^ <Please add first missing authors to populate metadata.> (Winter 2002). "Cervical Cap Newsletter" (PDF). Internet Archive. Archived from the original (PDF) on 2004-02-25. Retrieved 2007-07-22.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Grafenberg, E; Dickinson, RL (1944). "Conception control by plastic cervix cap". Western Journal of Surgery, Obstetrics, and Gynecology. 12 (8): 335–40. PMID 12233290.
- ^ "96/281/2 Contraceptive cervical cap, 'Vimule' cap". Powerhouse Museum Collection. 1995. Retrieved 2006-11-12.
- ^ Fairbanks, B; Scharfman, B (1980). "The cervical cap: Past and current experience". Women & Health. 5 (3): 61–80. doi:10.1300/j013v05n03_06. PMID 7018094.
- ^ Bernstein, Gerald S.; Kilzer, Linda H.; Coulson, Anne H.; Nakamura, Robert M.; Smith, Grace C.; Bernstein, Ruth; Frezieres, Ron; Clark, Virginia A.; Coan, Carl (1982). "Studies of cervical caps: I. Vaginal lesions associated with use of the vimule cap". Contraception. 26 (5): 443–56. doi:10.1016/0010-7824(82)90143-3. PMID 7160179.
- ^ United States. Food and Drug Administration FDA (1988). "Notice, 11 July 1988". Annual Review of Population Law. 15: 19. PMID 12289360.
- ^ Gallagher, Dana; Richwald, Gary (1989). "Feminism and Regulation Collide". Women & Health. 15 (2): 87. doi:10.1300/J013v15n02_07.
- ^ "Archived copy". Archived from the original on 2010-08-16. Retrieved 2010-10-12.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ Prentif: "Birth control options: the Cedar River Clinic's Birth Control Chart". Women's Health Activist. AccessMyLibrary.com. 2007-07-01. Retrieved 2008-07-11.
The Prentif cap is no longer being manufactured, but some clinics still have it in stock.
Prentif, Vimule, and Dumas: "Portio Kappen". Kessel-Marketing. 2007. Archived from the original on April 23, 2008. Retrieved 2008-07-10.Prentif, Vimule und Dumas sind nicht mehr verfügbar. (Prentif, Vimule and Dumas are no longer available.)
- ^ Planned Parenthood (2008-05-16). "Cervical Cap (FemCap)". Retrieved 2009-02-03.
- ^ "Archived copy". Archived from the original on 2010-08-15. Retrieved 2010-10-12.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ http://www.barriermethods.com/
- ^ a b c d Johnson, Jennifer (December 1, 2005). "Diaphragm, Cervical Cap and Shield". Planned Parenthood. Archived from the original on March 25, 2008. Retrieved 2008-04-19.
- ^ a b "Cervical Cap - Q&A". Feminist Women's Health Center. January 2006. Retrieved 2008-04-19.
- ^ <Please add first missing authors to populate metadata.> (1989). "Uncertainty exists on availability of cervical cap, distributor says". Contracept Technol Update. 10 (4): 57–8. PMID 12342202.
- ^ Summary of Safety and Effectiveness Data Archived 2008-09-12 at the Wayback Machine
- ^ a b c "Directions for use". FemCap. 2007. Archived from the original on March 10, 2008. Retrieved 2008-04-19.
- ^ a b "Instructions for Use". Veos PLC. 2003. Retrieved 2008-04-19.
- ^ a b "Cervical Cap". Family Practice Notebook. 2000. Archived from the original on September 30, 2007. Retrieved 2008-04-19.
- ^ Instructional video
- ^ a b "Frequently Asked Questions". FemCap. 2007. Retrieved 2008-04-19.
- ^ Richwald, GA; Greenland, S; Gerber, MM; Potik, R; Kersey, L; Comas, MA (1989). "Effectiveness of the cavity-rim cervical cap: Results of a large clinical study". Obstetrics and Gynecology. 74 (2): 143–8. PMID 2664609.
- ^ Oves Medical Data
- ^ Mauck, Christine; Glover, Lucinda H.; Miller, Eric; Allen, Susan; Archer, David F.; Blumenthal, Paul; Rosenzweig, Bruce A.; Dominik, Rosalie; Sturgen, Kim (1996). "Lea's Shield®: A study of the safety and efficacy of a new vaginal barrier contraceptive used with and without spermicide". Contraception. 53 (6): 329–35. doi:10.1016/0010-7824(96)00081-9. PMID 8773419.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (help) - ^ Roizen, Judith; Richardson, Sue; Tripp, John; Hardwicke, Hilary; Lam, Tran Quang (2002). "Oves® contraceptive cap: Short-term acceptability, aspects of use and user satisfaction". Journal of Family Planning and Reproductive Health Care. 28 (4): 188–92. doi:10.1783/147118902101196829. PMID 12419058.
- ^ Mauck, CK; Weiner, DH; Creinin, MD; Archer, DF; Schwartz, JL; Pymar, HC; Ballagh, SA; Henry, DM; Callahan, MM (2006). "FemCap™ with removal strap: ease of removal, safety and acceptability". Contraception. 73 (1): 59–64. doi:10.1016/j.contraception.2005.06.074. PMC 2876188. PMID 16371297.
- ^ Bounds, W; Guillebaud, J (1999). "Lea's Shield contraceptive device: Pilot study of its short-term patient acceptability and aspects of use". The British Journal of Family Planning. 24 (4): 117–20. PMID 10023094.
- ^ Chandra, A; Martinez, GM; Mosher, WD; Abma, JC; Jones, J (2005). "Fertility, family planning, and reproductive health of U.S. Women: Data from the 2002 National Survey of Family Growth" (PDF). Vital and Health Statistics. Series 23, Data from the National Survey of Family Growth (25): 1–160. PMID 16532609. See Table 53 and 56.
External links
- Cervical Barrier Advancement Society
- Diaphragms and Caps (Yahoo Group)
- Femcap website
- Oves website

