Posterior cruciate ligament
| Posterior cruciate ligament | |
|---|---|
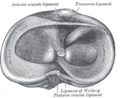
 Diagram of the knee | |
| Details | |
| From | antero-medial aspect of medial femoral condyle |
| To | posterolateral aspect of proximal tibia |
| Identifiers | |
| Latin | ligamentum cruciatum posterius genus |
| MeSH | D016119 |
| TA98 | A03.6.08.008 |
| TA2 | 1891 |
| FMA | 44617 |
| Anatomical terminology | |
The posterior cruciate ligament (or PCL) is one of the four major ligaments of the knee. It connects the posterior intercondylar area of the tibia to the medial condyle of the femur. This configuration allows the PCL to resist forces pushing the tibia posteriorly relative to the femur.
The PCL is an intracapsular ligament along with the anterior cruciate ligament (ACL) because it lies deep within the knee joint. They are both isolated from the fluid-filled synovial cavity, with the synovial membrane wrapped around them. The PCL gets its name by attaching to the posterior portion of the tibia.[1]
Structure
The PCL is located within the knee joint where it stabilizes the articulating bones, particularly the femur and the tibia, during movement. It originates from the lateral edge of the medial femoral condyle and the roof of the intercondyle notch [2] then stretches, at a posterior and lateral angle, toward the posterior of the tibia just below its articular surface.[3][4][5][6]

Function
Although each PCL is a unified unit, they are described as separate anterolateral and posteromedial sections based off where each section's attachment site and function.[7] During knee joint movement, the PCL rotates [6][8] such that the anterolateral section stretches in knee flexion but not in knee extension and the posteromedial bundle stretches in extension rather than flexion.[4][9]
The function of the PCL is to prevent the femur from sliding off the anterior edge of the tibia and to prevent the tibia from displacing posterior to the femur. The posterior cruciate ligament is located within the knee. Ligaments are sturdy bands of tissues that connect bones. Similar to the anterior cruciate ligament, the PCL connects the femur to the tibia.
Clinical significance
Common causes of injuries are direct blows to the flexed knee, such as the knee hitting the dashboard in a car accident or falling hard on the knee, both instances displacing the tibia posterior to the femur.[10]
An additional test of posterior cruciate ligament injury is the posterior sag test, where, in contrast to the drawer test, no active force is applied. Rather, the person lies supine with the leg held by another person so that the hip is flexed to 90 degrees and the knee 90 degrees.[11] The main parameter in this test is step-off, which is the shortest distance from the femur to a hypothetical line that tangents the surface of the tibia from the tibial tuberosity and upwards. Normally, the step-off is approximately 1 cm, but is decreased (Grade I) or even absent (Grade II) or inverse (Grade III) in injuries to the posterior cruciate ligament.[12] The posterior drawer test is one of the tests used by doctors and physiotherapists to detect injury to the PCL. Patients who are suspected to have a posterior cruciate ligament injury should always be evaluated for other knee injuries that often occur in combination with an PCL injuries. These include cartilage/meniscus injuries, bone bruises, ACL tears, fractures, posterolateral injuries and collateral ligament injuries.
There are four different grades of classification in which medical doctor’s classify a PCL injury: Grade I, the PCL has a slight tear. Grade II, the PCL ligament is minimally torn and becomes loose. Grade III, the PCL is torn completely and the knee can now be categorized as unstable. Grade IV, the ligament is damaged along with another ligament housed in the knee (i.e. ACL). With these grades of PCL injuries, there are different treatments available for such injuries.[citation needed]

Mechanism

In this position, the PCL functions to prevent movement of the tibia in the posterior direction [4][13] and to prevent the tilting or shifting of the patella.[14] However, the respective laxity of the two sections makes the PCL susceptible to injury during hyperflexion, hyperextension,[15] and in a mechanism known as a dashboard injury.[6] Because ligaments are viscoelastic[16]) they can handle higher amounts of stress only when the load is increased slowly.[17] When hyperflexion and hyperextension occur suddenly in combination with this viscoelastic behavior, the PCL deforms or tears.[15] In the third and most common mechanism, the dashboard injury mechanism, the knee experiences impact in a posterior direction during knee flexion toward the space above the tibia.[7][15] These mechanisms occur in excessive external tibial rotation and during falls that induce a combination of extension and adduction of the tibia, which is referred to as varus-extension stress,[7] or that occur while the knee is flexed.[15]
Treatment
It is possible for the PCL to heal on its own. Surgery is usually required in complete tears of the ligament. Surgery usually takes place after a few weeks, in order to allow swelling to decrease and regular motion to return to the knee. A procedure called ligament reconstruction is used to replace the torn PCL with a new ligament, which is usually a graft taken from the hamstring or Achilles tendon from a host cadaver. An arthroscope allows a complete evaluation of the entire knee joint, including the knee cap (patella), the cartilage surfaces, the meniscus, the ligaments (ACL & PCL), and the joint lining. Then, the new ligament is attached to the bone of the thigh and lower leg with screws to hold it in place.[18] Surgery to repair the posterior cruciate ligament is controversial due to its placement and technical difficulty.[19]
It is possible for the PCL to heal on its own without surgery when it is in Grades I and II. PCL injuries that are diagnosed in these categories can have their recovery times reduced by performing certain rehabilitative exercises. Fernandez and Pugh(2012) found that following a PCL grade II diagnosis, a multimodal treatment that spanned over the course of 8 weeks consisting of chiropractic lumbopelvic manipulation, physiotherapy, and implementing an exercise program that emphasized in eccentric muscle contraction (lunges, 1-leg squats, and trunk stabilization) which proved to be an effective way to recover from the PCL injury.[20] For Grades III and IV, operative surgery is recommended or is usually needed. Grafts is the method when addressing PCL injuries that are in need of operative surgery. With grafts, there are different methods such as the tibial inlay or tunnel method.[21]
Other animals
In the quadruped stifle (analogous to the human knee), based on its anatomical position, it is referred to as the caudal cruciate ligament.[22]
Additional images
-
Head of right tibia seen from above, showing menisci and attachments of ligaments.
-
Capsule of right knee-joint (distended). Posterior aspect.
-
Magnetic resonance imaging evaluation demonstrating normal signal of both anterior and posterior cruciate ligaments (arrows).
-
Anterior view of knee.
-
Knee joint. Deep dissection. Anterior view
References
- ^ Saladin, K. S. 2010. Anatomy & Physiology: 5th edition. McGraw-Hill[page needed]
- ^ Amis, AA.; Gupte, CM.; Bull, AM.; Edwards, A. (Mar 2006). "Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments". Knee Surg Sports Traumatol Arthrosc. 14 (3): 257–63. doi:10.1007/s00167-005-0686-x. PMID 16228178.
- ^ Girgis, FG.; Marshall, JL.; Monajem, A. "The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis". Clin Orthop Relat Res. 106: 216–31. doi:10.1097/00003086-197501000-00033. PMID 1126079.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ a b c Chandrasekaran, S.; Ma, D.; Scarvell, JM.; Woods, KR.; Smith, PN. (Dec 2012). "A review of the anatomical, biomechanical and kinematic findings of posterior cruciate ligament injury with respect to non-operative management". Knee. 19 (6): 738–45. doi:10.1016/j.knee.2012.09.005. PMID 23022245.
- ^ Edwards, A.; Bull, AM.; Amis, AA. (Mar 2007). "The attachments of the fiber bundles of the posterior cruciate ligament: an anatomic study". Arthroscopy. 23 (3): 284–90. doi:10.1016/j.arthro.2006.11.005. PMID 17349472.
- ^ a b c Voos, JE.; Mauro, CS.; Wente, T.; Warren, RF.; Wickiewicz, TL. (Jan 2012). "Posterior cruciate ligament: anatomy, biomechanics, and outcomes". Am J Sports Med. 40 (1): 222–31. doi:10.1177/0363546511416316. PMID 21803977.
- ^ a b c Malone, AA.; Dowd, GS.; Saifuddin, A. (Jun 2006). "Injuries of the posterior cruciate ligament and posterolateral corner of the knee". Injury. 37 (6): 485–501. doi:10.1016/j.injury.2005.08.003. PMID 16360655.
- ^ DeFrate, LE.; Gill, TJ.; Li, G. (Dec 2004). "In vivo function of the posterior cruciate ligament during weightbearing knee flexion". Am J Sports Med. 32 (8): 1923–8. doi:10.1177/0363546504264896. PMID 15572322.
- ^ Race, A.; Amis, AA. (Jan 1994). "The mechanical properties of the two bundles of the human posterior cruciate ligament". J Biomech. 27 (1): 13–24. doi:10.1016/0021-9290(94)90028-0. PMID 8106532.
- ^ MedlinePlus Encyclopedia: Posterior cruciate ligament (PCL) injury
- ^ Posterior Sag Test From The University of West Alabama, Athletic Training & Sports Medicine Center. Retrieved Feb 2011
- ^ Cole, Brian; Miller, Mark J. (2004). Textbook of arthroscopy. Philadelphia: Saunders. p. 719. ISBN 0-7216-0013-1.
- ^ Castle, Thomas H; Noyes, Frank R; Grood, Edward S (1992). "Posterior Tibial Subluxation of the Posterior Cruciate-Deficient Knee". Clinical Orthopaedics and Related Research (284): 193–202. doi:10.1097/00003086-199211000-00027. PMID 1395293.
- ^ von Eisenhart-Rothe, Ruediger; Lenze, Ulrich; Hinterwimmer, Stefan; Pohlig, Florian; Graichen, Heiko; Stein, Thomas; Welsch, Frederic; Burgkart, Rainer (2012). "Tibiofemoral and patellofemoral joint 3D-kinematics in patients with posterior cruciate ligament deficiency compared to healthy volunteers". BMC Musculoskeletal Disorders. 13: 231. doi:10.1186/1471-2474-13-231. PMC 3517747. PMID 23181354.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d Janousek, Andreas T.; Jones, Deryk G.; Clatworthy, Mark; Higgins, Laurence D.; Fu, Freddie H. (1999). "Posterior Cruciate Ligament Injuries of the Knee Joint". Sports Medicine. 28 (6): 429–41. doi:10.2165/00007256-199928060-00005. PMID 10623985.
- ^ Hamill, Joseph; Knutzen, Kathleen (2009). Biomechanical basis of human movemen. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins. p. 50. ISBN 978-0-7817-9128-1.
- ^ Hamill, Joseph; Knutzen, Kathleen (2009). Biomechanical basis of human movemen. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins. p. 30. ISBN 978-0-7817-9128-1.
- ^ http://www.orthspec.com/pdfs/PCL-injuries.pdf[full citation needed]
- ^ Jonathan Cluett, M.D. (2003-08-05). "Injuries to the posterior cruciate ligament (PCL)". about.com. Retrieved 2006-11-11.
- ^ Fernandez, Matthew; Pugh, David (2012). "Multimodal and interdisciplinary management of an isolated partial tear of the posterior cruciate ligament: a case report". Journal of Chiropractic Medicine. 11 (2): 84–93. doi:10.1016/j.jcm.2011.10.005. PMC 3368977. PMID 23204951.
- ^ Wind, William M.; Bergfeld, John A.; Parker, Richard D. (2004). "Evaluation and Treatment of Posterior Cruciate Ligament Injuries: Revisited". American Journal of Sports Medicine. 32 (7): 1765–75. doi:10.1177/0363546504270481. PMID 15494347.
- ^ Blood, Douglas C.; Studdert, Virginia P.; Gay, Clive C., eds. (2007). "Cruciate". Saunders Comprehensive Veterinary Dictionary (3rd ed.). Elsevier. ISBN 978-0-7020-2788-8. Retrieved September 8, 2009.
External links
- lljoints at The Anatomy Lesson by Wesley Norman (Georgetown University) (antkneejointopenflexed)
- Dealing with Torn Ligament in the Knee
- http://www.orthspec.com/pdfs/PCL-injuries.pdf