Tonsillectomy


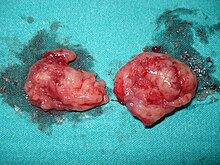
A tonsillectomy is a surgical procedure in which the tonsils are removed. Sometimes the adenoids are removed at the same time.
Reasons for tonsillectomy
Tonsillectomy may be indicated when the patient:
- Experiences frequent bouts of acute tonsillitis. The number requiring tonsillectomy varies with the severity of the episodes. One case, even severe, is generally not enough for most surgeons to decide tonsillectomy is necessary.
- Has chronic tonsillitis, consisting of persistent, moderate-to-severe throat pain.
- Has multiple bouts of peritonsillar abscess.
- Has sleep apnea (stopping or obstructing breathing at night due to enlarged tonsils or adenoids)
- Has difficulty eating or swallowing due to enlarged tonsils (very unusual reason for tonsillectomy)
- Produces tonsilloliths in the back of their mouth.
- Has abnormally large tonsils with crypts (Craters or impacts in the tonsils)
Common causes and demographics
Infections requiring tonsillectomy are often a result of Streptococcus ("strep throat"), but some may be due to other bacteria, such as Staphylococcus, or viruses. However, the etiology of the condition is largely irrelevant in determining whether tonsillectomy is required [1].
Most tonsillectomies are performed on children, although many are also performed on teenagers and adults. The number of tonsillectomies in the United States has dropped significantly from several million in the 1970s to approximately 600,000 in the late 1990s[citation needed]. This has been due in part to more stringent guidelines for tonsillectomy and adenoidectomy (see tonsillitis and adenoid). Still, debate about the usefulness of tonsillectomies continues. Not surprisingly, the otolaryngology literature is usually pro-tonsillectomy, whereas the pediatric literature has the opposing view [citation needed]. Enlarged tonsils are removed more often among adults and children for sleep apnea (airway obstruction while sleeping), snoring, and upper airway obstruction. Children who have sleep apnea can do poorly in school, are tired during the day, may be bed wetters beyond what is normal, and have some links to ADHD [2] [3].
Tonsillectomy in adults is more painful [citation needed] than in children, although each patient will have a different experience. Post-operative recovery can take from 10 up to 20 days, during which narcotic analgesics are typically prescribed. Advice on post-operative food intake varies around the world. Patients in the United States and Canada are usually advised not to eat "crunchy" or "rough" food (toast, biscuits, cookies & crackers) as they may scrape the back of the throat, increasing the risk of bleeding or infection after the operation. On the other hand, patients in the United Kingdom are often encouraged to eat rough foods to keep the tonsillar beds clean and to avoid the throat becoming lined with slough. Similarly, some believe that dairy products tend to coat the throat causing an increase in possible infection and therefore discourage their use. Spicy and acidic foods are irritating and should be avoided. Proper hydration is also very important during this time, since dehydration can increase throat pain, leading to a vicious cycle of poor fluid intake. At some point, most commonly 7-11 days after the surgery (but occasionally as long as two weeks (14 days) after), bleeding can occur when scabs begin sloughing off from the surgical sites. The overall risk of bleeding is approximately 1-2% higher in adults [4]. Approximately 3% of adult patients develop significant bleeding at this time. The bleeding might naturally stop quickly, or else mild intervention (e.g., gargling cold water) could be needed (but ask the doctor before gargling because it might bruise the area of the skin that has been cauterized). Otherwise, a surgeon must repair the bleeding immediately by cauterization, which presents all the risks associated with emergency surgery (most having to do with the administration of anesthesia on a patient whose stomach is not empty). Various procedures are available to remove tonsils, each with different advantages and disadvantages. Children and teenagers sometimes exhibit a noticeable change in voice [5] after the operation [6].
Methods of tonsil removal
The first report of tonsillectomy was made by the Roman encyclopedist Celsus in 30 AD. He described scraping the tonsils and tearing them out or picking them up with a hook and excising them with a scalpel. Today, the scalpel is still the preferred surgical instrument of many ear, nose, and throat specialists. However, there are other procedures available – the choice may be dictated by the extent of the procedure (complete tonsil removal versus partial tonsillectomy) and other considerations such as pain and post-operative bleeding. A quick review of each procedure follows:
- Dissection and snare method: Removal of the tonsils by use of a forceps and scissors with a wire loop called a 'snare' is the most common method practiced by otolaryngologists today. The procedure requires the patient to undergo general anesthesia; the tonsils are completely removed and the skin is cauterized. The patient will leave with minimal post-operative bleeding.
- Electrocautery: Electrocautery burns the tonsillar tissue and assists in reducing blood loss through cauterization. Research has shown that the heat of electrocautery (400°C) results in thermal injury to surrounding tissue. This may result in more discomfort during the postoperative period.
- Harmonic scalpel: This medical device uses ultrasonic energy to vibrate its blade at 55kHz. Invisible to the naked eye, the vibration transfers energy to the tissue, providing simultaneous cutting and coagulation. The temperature of the surrounding tissue reaches 80°C. Proponents of this procedure assert that the end result is precise cutting with minimal thermal damage.
- Radiofrequency ablation: Monopolar radiofrequency thermal ablation transfers radiofrequency energy to the tonsil tissue through probes inserted in the tonsil. The procedure can be performed in an office (outpatient) setting under light sedation or local anesthesia. After the treatment is performed, scarring occurs within the tonsil causing it to decrease in size over a period of several weeks. The treatment can be performed several times. The advantages of this technique are minimal discomfort, ease of operations, and immediate return to work or school. Tonsillar tissue remains after the procedure but is less prominent. This procedure is recommended for treating enlarged tonsils and not chronic or recurrent tonsillitis.
- Thermal Welding: A new technology which uses pure thermal energy to seal and divide the tissue. The absence of thermal spread means that the temperature of surrounding tissue is only 2-3 °C higher than normal body temperature. Clinical papers show patients with minimal post-operative pain (no requirement for narcotic pain-killers), zero edema (swelling) plus almost no incidence of bleeding. Hospitals in the US are advertising this procedure as "Painless Tonsillectomy". Also known as Tissue Welding.
- Carbon dioxide laser: Laser tonsil ablation (LTA) finds the otolaryngologist employing a hand-held CO2 or KTP laser to vaporize and remove tonsil tissue. This technique reduces tonsil volume and eliminates recesses in the tonsils that collect chronic and recurrent infections. This procedure is recommended for chronic recurrent tonsillitis, chronic sore throats, severe halitosis, or airway obstruction caused by enlarged tonsils. The LTA is performed in 15 to 20 minutes in an office setting under local anesthesia. The patient leaves the office with minimal discomfort and returns to school or work the next day. Post-tonsillectomy bleeding may occur in 2-5% of patients. Previous research studies state that laser technology provides significantly less pain during the post-operative recovery of children, resulting in less sleep disturbance, decreased morbidity, and less need for medications. On the other hand, some believe that children are adverse to outpatient procedures without sedation.
- Microdebrider: The microdebrider is a powered rotary shaving device with continuous suction often used during sinus surgery. It is made up of a cannula or tube, connected to a hand piece, which in turn is connected to a motor with foot control and a suction device. The endoscopic microdebrider is used in performing a partial tonsillectomy, by partially shaving the tonsils. This procedure entails eliminating the obstructive portion of the tonsil while preserving the tonsillar capsule. A natural biologic dressing is left in place over the pharyngeal muscles, preventing injury, inflammation, and infection. The procedure results in less post-operative pain, a more rapid recovery, and perhaps fewer delayed complications. However, the partial tonsillectomy is suggested for enlarged tonsils – not those that incur repeated infections.
- Bipolar Radiofrequency Ablation (see Coblation tonsillectomy): This procedure produces an ionized saline layer that disrupts molecular bonds without using heat. As the energy is transferred to the tissue, ionic dissociation occurs. This mechanism can be used to remove all or only part of the tonsil. It is done under general anesthesia in the operating room and can be used for enlarged tonsils and chronic or recurrent infections. This causes removal of tissue with a thermal effect of 45-85 °C. It has been claimed that this technique results in less pain, faster healing, and less post operative care [7]. However, review of 21 studies gives conflicting results about levels of pain, and its comparative safety has yet to be confirmed [8].
See also
References
- ^ http://www.ivillage.com/topics/health/0,,232762,00.html
- ^ Avior G, Fishman G, Leor A, Sivan Y, Kaysar N, Derowe A (2004). "The effect of tonsillectomy and adenoidectomy on inattention and impulsivity as measured by the Test of Variables of Attention (TOVA) in children with obstructive sleep apnea syndrome". Otolaryngol Head Neck Surg. 131 (4): 367–71. doi:10.1016/j.otohns.2004.04.015. PMID 15467601.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ray RM, Bower CM (2005). "Pediatric obstructive sleep apnea: the year in review". Curr Opin Otolaryngol Head Neck Surg. 13 (6): 360–5. doi:10.1097/01.moo.0000186076.53986.71. PMID 16282765.
- ^ Windfuhr JP, Chen YS, Remmert S (2005). "Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients". Otolaryngol Head Neck Surg. 132 (2): 281–6. doi:10.1016/j.otohns.2004.09.007. PMID 15692542.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tonsillectomy and Adenoidectomy for Obstructive Sleep Apnea
- ^ MedlinePlus: Tonsils and Adenoids
- ^ Friedman M, LoSavio P, Ibrahim H, Ramakrishnan V (2003). "Radiofrequency tonsil reduction: safety, morbidity, and efficacy". Laryngoscope. 113 (5): 882–7. doi:10.1097/00005537-200305000-00020. PMID 12792327.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Windfuhr JP (2007). "[Coblation tonsillectomy: a review of the literature.]". HNO. 55: 337. doi:10.1007/s00106-006-1523-3. PMID 17431570.
{{cite journal}}: Unknown parameter|month=ignored (help)
