User:MendozaLine99/sandbox
Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord.[1][2] Neurogenic means that the problem originates with the nervous system. Claudication, from the Latin word for to limp, refers to painful cramping or weakness in the legs.[3] NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.
NC may involve one or both lower extremities and usually presents as some combination of discomfort, pain, numbness, or weakness in the calves, buttocks, and/or thighs that is precipitated by walking and prolonged standing. The pain is classically relieved by a change in position or flexion of the waist.[4] Therefore, patients with NC have less disability in climbing steps, pushing carts, and cycling.[1]
The term neurogenic claudication is sometimes used interchangeably with spinal stenosis. However, the former is a clinical term, while the latter more specifically describes the finding of spinal narrowing on imaging.[5] The International Association for the Study of Pain defines neurogenic claudication as, "pain from intermittent compression and/or ischemia of a single or multiple nerve roots within an intervertebral foramen or the central spinal canal."[5] This definition reflects the current hypotheses for the pathophysiology of NC, which is thought to be related to compression of lumbosacral nerve roots by surrounding structures such as hypertrophied facet joints or ligamentum flavum, bone spurs, scar tissue, and bulging or herniated discs.[6]
Diagnosis of neurogenic claudication is based off of typical clinical features, the physical exam, and findings of spinal stenosis on imaging.[1] In addition to vascular claudication, diseases affecting the spine and musculoskeletal system should be considered in the differential diagnosis.[4] Treatment options for NC may be nonsurgical or surgical. Nonsurgical interventions include drugs, physical therapy, and spinal injections.[7] Spinal decompression is the main surgical intervention and is the most common back surgery in patients over 65.[1]
Signs and symptoms
[edit]Neurogenic claudication describes pain, weakness, fatigue, and/or paresthesias that extend into the lower extremities.[4] These symptoms may involve only one leg, but they usually involve both. Leg pain is usually more significant than back pain in individuals who have both.[8] NC is classically distinguished by symptoms improving or worsening with certain activities and maneuvers. Pain may occur with walking, standing, and/or back extension. Sitting and bending or leaning forward tend to provide relief. Patients may also report that pain is worse while walking down stairs and improved while walking up stairs or using a bicycle or shopping cart.[1] A positive "shopping cart sign" refers to the worsening of pain with spinal extension and improvement with spinal flexion.[7]
On physical exam, patients with NC have normal peripheral pulses.[1] The neurologic exam, straight leg raise, and femoral nerve stretch are typically normal. Abnormal signs may be revealed if the patient is observed walking until they exhibit NC. For example, a positive "stoop test" is observed if bending forward or stooping while walking relieves symptoms.[2] Occasionally, patients may have other signs such as sensory loss or gait changes.[4]
Causes
[edit]Neurogenic claudication is the fundamental clinical feature of lumbar spinal stenosis, which may be congenital or acquired. The causes of LSS are most commonly acquired and include degenerative changes such as degenerative disc disease and spinal osteoarthritis. LSS may also be acquired from changes due to spinal surgery such as excess scar tissue or bone formation.[6] Other secondary causes include space-occupying lesions, ankylosing spondylitis, rheumatoid arthritis, and Paget's disease. Less commonly, the cause of spinal stenosis may be present at birth as seen in achondroplasia, spina bifida, and certain mucopolysaccharidoses.[9]
Risk factors for LSS include[10][9]:
- Age
- Degenerative changes of the spine
- Obesity
- Family history of spinal stenosis
- Tobacco use
- Occupation involving repetitive mechanical stress on the spine
Diagnosis and Evaluation
[edit]Neurogenic claudication is one subtype of the clinical syndrome of lumbar spinal stenosis (LSS).[4] No gold standard diagnostic criteria currently exist, but evaluation and diagnosis is generally based on the patient history, physical exam, and medical imaging.[1] The accuracy of a diagnosis of NC increases with each additional suggestive clinical finding. Therefore, a combination of signs and symptoms may be more helpful in diagnosing NC than any single feature of the history or physical exam. These signs and symptoms include pain triggered by standing, pain relieved by sitting, symptoms above the knees, and a positive "shopping cart sign".[5] Specific questions that may aid diagnosis include[7]:
- "Does the patient have leg or buttock pain while walking?"
- "Does the patient flex forward to relieve symptoms?"
- "Does patient feel relief when using a shopping cart or bicycle?"
- "Does the patient have motor or sensory disturbance while walking?"
- "Are the pulses in the foot present and symmetric?"
- "Does the patient have lower extremity weakness?"
- "Does the patient have low back pain?"
The physical exam may include observation, evaluation of pulses in the foot, lumbar spine range of motion, and components of a neurological exam.[1]
Helpful imaging may include x-rays, computed tomography (CT), CT myelogram, and magnetic resonance imaging (MRI), but MRI is preferred.[1] Abnormal MRI findings may be present in two-thirds of asymptomatic individuals, and imaging findings of spinal stenosis do not correlate well with symptom severity. Therefore, imaging findings must be considered in the context of a patient's history and physical exam when seeking a diagnosis.[2] The evidence for using objective imaging findings to define neurogenic claudication has been conflicting.[8]
Differential diagnosis
[edit]Neurogenic claudication must be differentiated from other causes of leg pain, which may be present in a number of conditions involving the spine and musculoskeletal system. The differential diagnosis for NC includes:[4]
- Vascular claudication
- Lumbosacral radicular pain secondary to lumbar disc herniation
- Referred pain from spinal structures, hip or sacroiliac joint, myofascia, or viscera
- Trochanteric bursitis
- Piriformis syndrome
- Muscle pain
- Vertebral compression fracture
- Compartment syndrome
- Peripheral neuropathy
Neurogenic vs vascular claudication
[edit]| Clinical feature | Neurogenic | Vascular |
|---|---|---|
| Pain worse with | Standing, walking | Walking |
| Pain relieved by | Spinal flexion, sitting | Standing |
| Timing of relief | Within minutes | Immediately |
| Location | Above the knees | Below the knees |
| Radiation of pain | Extends down legs | Extends up legs |
| Quality of pain | Sharp | Cramping, dull |
| Back pain | Common | Sometimes |
| Peripheral pulses | Present | May be absent |
Both neurogenic claudication and vascular claudication manifest as leg pain with walking, but several key features help distinguish between these conditions.[6] In contrast to NC, vascular claudication does not vary with changes in posture.[4] Patients with vascular claudication may experience relief with standing, which may provoke symptoms in NC. The walking distance necessary to produce pain in vascular claudication is more consistent than in neurogenic claudication.[8]
Pathophysiology
[edit]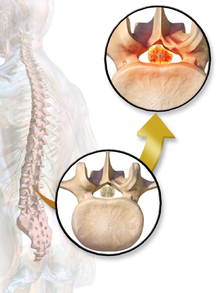
Degenerative disc disease (DDD) may trigger the pathogenesis of neurogenic claudication. When intervertebral discs degenerate and change shape in DDD, the normal movements of the spine are interrupted. This results in spinal instability and more degenerative changes in spinal structures including facet joints, ligamentum flavum, and intervertebral discs. These pathologic changes result in narrowing of the vertebral canal and neurovascular compression at the lumbosacral nerve roots.[1][11] However, because the severity of symptoms does not correlate well with the degree of stenosis and nerve root compression, a clear understanding of the specific pathogenesis remains challenging.[6]
It is currently unknown what exactly causes the pain of NC. The two main proposed mechanisms agree that neurovascular compression plays a role. The ischemic theory proposes that poor blood supply to the spinal nerve roots results in NC. In contrast, the venous stasis theory proposes that a combination of low oxygen levels and metabolite buildup are responsible due to venous backup at the cauda equina.[6] Pain with walking may be partially explained by the corresponding increase in nerve root oxygen requirements.[9]
These changes in blood flow may occur during back extension when shifts in vertebral structures and ligaments narrow the spinal canal and compress the neurovasculature.[9] Compared to a neutral position, extended spines exhibit 15% less cross-sectional area of the intervertebral foramina, and nerve root compression is present one-third of the time.[7] These dynamic changes in the shape of the spinal canal are more pronounced in individuals with spinal stenosis. The amount of narrowing may be 67% in LSS compared to 9% in healthy spines.[1]
Treatment
[edit]
Decreased walking ability due to neurogenic claudication is the primary disabling feature of lumbar spinal stenosis (LSS).[11] It is therefore the target of most treatments, which may be grouped broadly into nonsurgical and surgical options.[11][6] Nonsurgical treatments include medications, physical therapy, and spinal injections. Medication options for neurogenic claudication have included non-steroidal anti-inflammatory drugs (NSAIDs), prostaglandins, gabapentin, and methylcobalamin. However, the quality of evidence supporting their use is not high enough for specific recommendations. Physical therapy is commonly prescribed to patients, but the quality of evidence supporting its use for neurogenic claudication is also low.[7] One quarter of all epidural injections are administered to treat symptoms of LSS.[11] Preparations may contain lidocaine and/or steroids. They may be considered for short-term pain relief or to delay surgery, but their benefit is considered small.[1]
Symptoms of LSS, including neurogenic claudication, are the most common reason patients 65 and older undergo spinal surgery. Surgery is generally reserved for patients whose symptoms do not improve with nonsurgical treatments.[7] Spinal decompression is considered the mainstay of surgical treatment.[2] Alternative surgical options include the use of interspinous process spacers, minimally invasive lumbar decompression (MILD) procedure, and placement of a spinal cord stimulator. The MILD procedure aims to relieve spinal cord compression by percutaneous removal of portions of the ligamentum flavum and lamina.[7] The use of interspinous spacers is associated with increased costs and rates of reoperation, while evidence comparing effectiveness of the MILD procedure to spinal decompression is insufficient.[6] While studies show that surgery improves walking ability, comparisons between the efficacy of surgical and nonsurgical treatment of LSS have yielded mixed results.[11][6]
Prognosis
[edit]Individuals with lumbar spinal stenosis (LSS) may be asymptomatic for many years before developing symptoms such as neurogenic claudication.[1] Because those with LSS often seek treatment, the prognosis of untreated LSS is not known. However, estimates suggest that symptoms remain stable in most patients and may improve in one-third. Rapid worsening of symptoms in mild to moderate cases of LSS is unlikely.[6]
Epidemiology
[edit]Neurogenic claudication (NC) is associated with increasing age and mostly affects individuals over the age of 60. It is also more likely present in individuals with other spinal comorbidities.[1] NC may be present in greater than 90% of patients with spinal stenosis, which is present in almost half of patients with low back pain and affects over 200,000 people in the United States.[2][1][6]
Roughly 1 in 10 elderly men experience leg pain in combination with low back pain, and the proportion of those affected is doubled in retirement communities.[4] As the global life expectancy increases, the impact of spinal disease symptoms such as NC is likely to increase.[9]
See Also
[edit]References
[edit]- ^ a b c d e f g h i j k l m n o Deer, Timothy; Sayed, Dawood; Michels, John; Josephson, Youssef; Li, Sean; Calodney, Aaron K (2019-12-01). "A Review of Lumbar Spinal Stenosis with Intermittent Neurogenic Claudication: Disease and Diagnosis". Pain Medicine. 20 (Supplement_2): S32–S44. doi:10.1093/pm/pnz161. ISSN 1526-2375. PMC 7101166. PMID 31808530.
{{cite journal}}: CS1 maint: PMC format (link) - ^ a b c d e f Lee, Seung Yeop; Kim, Tae-Hwan; Oh, Jae Keun; Lee, Seung Jin; Park, Moon Soo (2015). "Lumbar Stenosis: A Recent Update by Review of Literature". Asian Spine Journal. 9 (5): 818. doi:10.4184/asj.2015.9.5.818. ISSN 1976-1902. PMC 4591458. PMID 26435805.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Pearce, J.M.S. (2005). "(Neurogenic) Claudication". European Neurology. 54 (2): 118–119. doi:10.1159/000088648. ISSN 0014-3022.
- ^ a b c d e f g h Suri, Pradeep; Rainville, James; Kalichman, Leonid; Katz, Jeffrey N. (2010-12-15). "Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis?". JAMA. 304 (23): 2628–2636. doi:10.1001/jama.2010.1833. ISSN 1538-3598. PMC 3260477. PMID 21156951.
- ^ a b c d Vining, Robert D.; Shannon, Zacariah K.; Minkalis, Amy L.; Twist, Elissa J. (2019-11). "Current Evidence for Diagnosis of Common Conditions Causing Low Back Pain: Systematic Review and Standardized Terminology Recommendations". Journal of Manipulative and Physiological Therapeutics. 42 (9): 651–664. doi:10.1016/j.jmpt.2019.08.002.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g h i j Lurie, Jon; Tomkins-Lane, Christy (2016-01-04). "Management of lumbar spinal stenosis". BMJ (Clinical research ed.). 352: h6234. doi:10.1136/bmj.h6234. ISSN 1756-1833. PMC 6887476. PMID 26727925.
- ^ a b c d e f g h Messiah, Shadi; Tharian, Antony R.; Candido, Kenneth D.; Knezevic, Nebojsa Nick (2019-05). "Neurogenic Claudication: a Review of Current Understanding and Treatment Options". Current Pain and Headache Reports. 23 (5): 32. doi:10.1007/s11916-019-0769-x. ISSN 1531-3433.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Genevay, Stephane; Atlas, Steven J. (2010-04). "Lumbar Spinal Stenosis". Best Practice & Research Clinical Rheumatology. 24 (2): 253–265. doi:10.1016/j.berh.2009.11.001. PMC 2841052. PMID 20227646.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b c d e S, Munakomi; La, Foris; M, Varacallo (2020 Jan). "Spinal Stenosis And Neurogenic Claudication". PubMed. PMID 28613622. Retrieved 2020-06-19.
{{cite web}}: Check date values in:|date=(help) - ^ Bagley, Carlos; MacAllister, Matthew; Dosselman, Luke; Moreno, Jessica; Aoun, Salah G; El Ahmadieh, Tarek Y (2019-01-31). "Current concepts and recent advances in understanding and managing lumbar spine stenosis". F1000Research. 8: 137. doi:10.12688/f1000research.16082.1. ISSN 2046-1402. PMC 6357993. PMID 30774933.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ a b c d e Ammendolia, Carlo; Stuber, Kent; Tomkins-Lane, Christy; Schneider, Michael; Rampersaud, Y. Raja; Furlan, Andrea D.; Kennedy, Carol A. (2014-06). "What interventions improve walking ability in neurogenic claudication with lumbar spinal stenosis? A systematic review". European Spine Journal. 23 (6): 1282–1301. doi:10.1007/s00586-014-3262-6. ISSN 0940-6719.
{{cite journal}}: Check date values in:|date=(help)
 | This is a user sandbox of MendozaLine99. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
