User:Mr. Ibrahem/Aortic dissection
| Aortic dissection | |
|---|---|
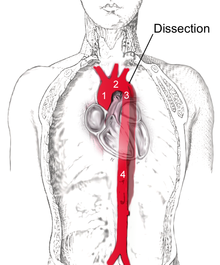 | |
| Dissection of the descending part of the aorta (3), which starts from the left subclavian artery and extends to the abdominal aorta (4). The ascending aorta (1) and aortic arch (2) are not involved in this image. | |
| Specialty | Vascular surgery, cardiothoracic surgery |
| Symptoms | severe chest or back pain, vomiting, sweating, lightheadedness[1][2] |
| Complications | Stroke, mesenteric ischemia, myocardial ischemia, aortic rupture[2] |
| Usual onset | Sudden[1][2] |
| Risk factors | High blood pressure, Marfan syndrome, Turner syndrome, bicuspid aortic valve, previous heart surgery, major trauma, smoking[1][2][3] |
| Diagnostic method | Medical imaging[1] |
| Prevention | Blood pressure control, not smoking [1] |
| Treatment | Depends on the type[1] |
| Prognosis | Mortality without treatment 10% (type B), 50% (type A)[3] |
| Frequency | 3 per 100,000 per year[3] |
Aortic dissection (AD) occurs when an injury to the innermost layer of the aorta allows blood to flow between the layers of the aortic wall, forcing the layers apart.[3] In most cases, this is associated with a sudden onset of severe chest or back pain, often described as "tearing" in character.[1][2] Also, vomiting, sweating, and lightheadedness may occur.[2] Other symptoms may result from decreased blood supply to other organs, such as stroke or mesenteric ischemia.[2] Aortic dissection can quickly lead to death from not enough blood flow to the heart or complete rupture of the aorta.[2]
It is more common in those with a history of high blood pressure, a number of connective tissue diseases that affect blood vessel wall strength including Marfan syndrome and Ehlers Danlos syndrome, a bicuspid aortic valve, and previous heart surgery.[2][3] Major trauma, smoking, cocaine use, pregnancy, a thoracic aortic aneurysm, inflammation of arteries, and abnormal lipid levels are also associated with an increased risk.[1][2] The diagnosis is suspected based on symptoms with medical imaging, such as computed tomography, magnetic resonance imaging, or ultrasound used to confirm and further evaluate the dissection.[1] The two main types are Stanford type A, which involves the first part of the aorta, and type B, which does not.[1]
Prevention is by blood pressure control, not smoking, and repair of thoracic aortic aneurysms.[1][4] Management depends on the part of the aorta involved.[1] Dissections that involve the first part of the aorta usually require surgery.[1][2] Surgery may be done either by an opening in the chest or from inside the blood vessel.[1] Dissections that involve the second part of the aorta can typically be treated with medications that lower blood pressure and heart rate, unless there are complications.[1][2]
Aortic dissection is relatively rare, occurring at an estimated rate of three per 100,000 people per year.[1][3] It is more common in men than women.[1] The typical age at diagnosis is 63, with about 10% of cases occurring before the age of 40.[1][3] Without treatment, about half of people with Stanford type A dissections die within three days and about 10% of people with Stanford type B dissections die within one month.[3] The first case of AD was described in the examination of King George II of Great Britain following his death in 1760.[3] Surgery for AD was introduced in the 1950s by Michael E. DeBakey.[3]
References[edit]
- ^ a b c d e f g h i j k l m n o p q r Nienaber, CA; Clough, RE (28 February 2015). "Management of acute aortic dissection". Lancet. 385 (9970): 800–11. doi:10.1016/s0140-6736(14)61005-9. PMID 25662791.
- ^ a b c d e f g h i j k l White, A; Broder, J; Mando-Vandrick, J; Wendell, J; Crowe, J (2013). "Acute aortic emergencies--part 2: aortic dissections". Advanced Emergency Nursing Journal. 35 (1): 28–52. doi:10.1097/tme.0b013e31827145d0. PMID 23364404.
- ^ a b c d e f g h i j Criado FJ (2011). "Aortic dissection: a 250-year perspective". Tex Heart Inst J. 38 (6): 694–700. PMC 3233335. PMID 22199439.
- ^ Isselbacher, Eric M. (15 February 2005). "Thoracic and Abdominal Aortic Aneurysms". Circulation. 111 (6): 816–828. doi:10.1161/01.CIR.0000154569.08857.7A.
