Urinalysis: Difference between revisions
→Urinalysis: do people do cells counts on spun urine ?? |
→Crystals: certainly not always pathological.... |
||
| Line 79: | Line 79: | ||
=====Crystals===== |
=====Crystals===== |
||
{{main|Crystalluria}} |
|||
[[File:UricAcid (cropped).jpg|thumb|[[Uric acid]] crystals in urine]] |
[[File:UricAcid (cropped).jpg|thumb|[[Uric acid]] crystals in urine]] |
||
Various compounds in the urine can [[Precipitation (chemistry)|precipitate]] to form crystals. The composition of crystals can be identified based on their appearance and the pH of the urine (many types preferentially form at an acidic or alkaline pH).{{r|McPherson2017|p=467}} Crystals that can be found in normal urine include [[uric acid]], monosodium urate, triple phosphate ([[ammonium magnesium phosphate]]), [[calcium oxalate]], and [[calcium carbonate]].{{r|nancy|pp=161–2}} Crystals can also appear as poorly defined aggregates of granular material, termed amorphous urates or amorphous phosphates (urates form in acid urine while phosphates form in alkaline urine). These are of no clinical significance, but they can interfere with microscopy by obscuring other elements (especially bacteria).{{r|cap|p=234–5}} Some drugs, such as [[sulfonamides]], may form crystals when excreted in the urine, and ammonium biurate crystals commonly occur in aged samples.{{r|nancy|pp=161–2}} Certain types of crystals are characteristically associated with disease states. [[Leucine]] and [[tyrosine]] crystals may be observed in liver disease,<ref name="echeverry">{{cite journal|last1=Echeverry|first1=G.|last2=Hortin|first2=G.L.|last3=Rai|first3=A.J.|title=Introduction to urinalysis: historical perspectives and clinical application.|journal=[[Methods in Molecular Biology]]|date=2010|volume=641|pages=1-12|doi=10.1007/978-1-60761-711-2_1}}</ref> and [[cystine]] crystals indicate [[cystinuria]] (although they look identical to hexagonal variants of uric acid crystals, and can only be distinguished with further testing).{{r|cap|p=290}} [[Cholesterol]] crystals may rarely be seen in [[nephrotic syndrome]] and [[chyluria]].{{r|cap|p=299}} |
|||
* [[Crystalluria|Crystals]] – associated with [[acute urate nephropathy]] (or acute uric acid nephropathy, AUAN) |
|||
** [[Calcium oxalate|Calcium oxalatin]] – associated with [[ethylene glycol]], [[kidney stone disease]] |
|||
=====Organisms===== |
=====Organisms===== |
||
Revision as of 17:57, 10 July 2022
| Urinalysis | |
|---|---|
 White blood cells seen under a microscope from a urine sample. | |
| Specialty | clinical pathology |
| MeSH | D016482 |
| Other codes | LOINC Codes for Urinalysis panels |
| MedlinePlus | 003579 |
Clinical urine tests are examinations of the physical and chemical properties of urine and its microscopic appearance to aid in medical diagnosis.[1] The term urinalysis—a portmanteau of the words urine and analysis[2]—generally refers to the gross (macroscopic) examination of the urine, chemical evaluation using urine test strips, and microscopic examination. Macroscopic examination targets parameters such as color, clarity, odor, and specific gravity; urine test strips measure chemical properties such as pH, glucose concentration, and protein levels; and light microscopy is performed to identify elements such as cells, urinary casts, crystals, and organisms.[3]: 441–3 Other analyses routinely performed on urine samples include urine electrolyte levels, drug testing, pregnancy testing and microbiological culture.
Methods
Urinalysis

Urinalysis involves assessment of the physical properties of urine, such as color and clarity; chemical analysis using a urine test strip; and microscopic examination.[3]: 441 Microscopic examination is not always included: it may be reserved for samples that have abnormal results on preliminary examinations or performed at the healthcare provider's request.[4]: 413 Test strips contain pads impregnated with chemical compounds that change color when they interact with specific elements in the urine; for example, nitrite, a compound produced by some bacteria that cause urinary tract infections, and leukocyte esterase, an enzyme found in white blood cells (WBCs) which acts as an indicator of the number of WBCs in the urine.[4]: 397–406
If microscopy is necessary, the urine is first centrifuged to concentrate the solid elements so that they can be viewed more easily. A drop of the concentrated sample is placed under a coverslip and examined, typically using the 10x and 40x objective lenses.[4]: 414–5 If it is necessary to determine the exact number of cells or casts in the sample, the unconcentrated urine can be placed in a counting chamber called a hemocytometer.[3]: 461 Urine is traditionally examined by light microscopy, but some laboratories use phase-contrast microscopes, which improve the visualization of elements such as urinary casts and mucus.[4]: 414–5 There are also automated systems that use fluorescence flow cytometry technology or pattern recognition to identify microscopic elements in the urine.[5]
Macroscopic examination
Color and clarity

Normal urine has a yellow hue, which is primarily caused by the pigment urochrome. The color can range from pale yellow to amber based on the individual's hydration status. Urine can develop a variety of abnormal colors, which in some cases may suggest disease.[6]: 38−9 A total lack of color indicates that the urine is extremely dilute, which may be caused by excessive fluid intake, diabetes insipidus, or diabetes mellitus. An unusually bright yellow color can occur after consumption of B vitamin supplements,[7]: 70 and dark yellow-brown urine may indicate a high concentration of bilirubin (bilirubinuria). Red urine often indicates the presence of red blood cells or hemoglobin (hematuria), but can also be caused by the consumption of foods containing red pigments,[6]: 38−9 such as beets. Myoglobin, a product of muscle breakdown, can give urine a red to reddish-brown color.[3]: 443 Purple urine occurs in purple urine bag syndrome.[8] The following are examples of some urine colors and their causes (not a complete listing).
- Orange: Insufficient fluid intake for conditions; intake of orange substances; intake of phenazopyridine for urinary symptoms.
- Dark:
- Reddish-orange: Intake of certain medications or other substances.
- Rusty-yellow to reddish-brown: Intake of certain medications or other substances.
- Dark brown: Intake of certain medications or other substances; damaged muscle (myoglobinuria due to rhabdomyolysis) from extreme exercise or other widespread damage, possibly medication related; altered blood; bilirubinuria; intake of phenolic substances; inadequate porphyrin metabolism; melanin from melanocytic tumors; presence of an abnormal form of hemoglobin, methemoglobin.
- Brownish-black to black: Intake of substances or medications; altered blood; a problem with homogentisic acid metabolism (alkaptonuria), which can also cause dark whites of the eyes and dark-colored internal organs and tissues (ochronosis); Lysol (a product that contains phenols) poisoning; melanin from melanocytic tumors). Paraphenylenediamine is a highly toxic ingredient of hair dye formulations that can cause acute kidney injury and result in black urine.[8]
- Magenta to purple-red: Presence of phenolphthalein, a stimulant laxative previously found in Ex-Lax.[9]
- Green, or dark with a greenish hue: Jaundice (bilirubinuria); problem with bile metabolism. Recent surgery requiring high doses of propofol infusion.[8] The use of a medication (Uribel) that is similar to phenazopyridine for the relief of urinary symptoms.
- Other colors: Various substances ingested in food or drink, particularly up to 48 hours prior to the presence of colored urine.[10]
The clarity of urine is also recorded during urinalysis. Urine is typically clear; materials such as crystals, cells, bacteria, and mucus can impart a cloudy appearance.[6]: 38−9 A milky appearance can be caused by a very high concentration of white blood cells or fats, or by chyluria (the presence of lymphatic fluid in the urine).[3]: 444–5
Smell
The odor (scent) of urine can normally vary from odorless (when very light colored and dilute) to a much stronger odor when the subject is dehydrated and the urine is concentrated.[11] The term urinoid denotes the normal odor of urine.[12] Transient changes in urine odor can occur after consuming certain foods, most notably asparagus. The urine of diabetics experiencing ketoacidosis (urine containing high levels of ketone bodies) may have a fruity or sweet smell, while urine from individuals with urinary tract infections often has a foul smell. Some inborn errors of metabolism cause characteristic odors, such as maple syrup urine disease (which takes its name from the urine scent) and phenylketonuria (which causes a "mousey" smell).[6]: 39
Urine test strip

A urine test strip can quantify:
- Leukocytes – with presence in urine known as leukocyturia
- Nitrite – with presence in urine known as nitrituria
- Protein – with presence in urine known as proteinuria, albuminuria, or microalbuminuria
- Erythrocytes – with presence in urine known as hematuria
- Specific gravity
- Glucose - with presence in urine known as glucosuria
- Bilirubin - with presence in urine known as bilirubinuria
- Ketones - with presence in urine known as ketonuria
Microscopic examination
The numbers and types of cells and/or material such as urinary casts can yield a great detail of information and may suggest a specific diagnosis. The microscopic components of urine are reported according to the amount present in the microscope's field of view at low magnification (reported as /lpf, meaning low-power field) and high magnification (/hpf for high-power field). Some elements such as crystals or bacteria are typically reported in a qualitative format, using terms such as "few" or "many" or grades from 1+ to 4+. Others, such as cells or casts, are reported using numerical ranges.[7]: 130
Elements that can be observed on microscopic examination include:
Cells
- Red blood cells
- Under the microscope, normal red blood cells (RBCs) appear as small concave discs. Their numbers are reported per high-power field.[7]: 137 In highly concentrated urine they may shrivel and develop a spiky shape, which is termed crenation, while in dilute urine they can swell and lose their hemoglobin, creating a faint outline known as a ghost cell. A small quantity of red blood cells (0–2 or 3/hpf) in the urine is considered normal.[3]: 461 [7]: 138
- An increased level of RBCs is termed hematuria. Microscopic hematuria is sometimes observed in healthy people after vigorous exercise[12] or as a consequence of contamination of the sample with menstrual blood.[7]: 138 Pathologic causes of hematuria are diverse and include trauma to the urinary tract, kidney stones, urinary tract infections, drug toxicity, cancers of the urinary system and prostate, and a variety of other renal and systemic diseases.[3]: 461 [7]: 139 [12] Abnormally shaped red blood cells with blob-like protrusions of the cell membrane, called dysmorphic RBCs, are thought to represent damage to the glomerulus.[7]: 137–8 [14]
- White blood cells
- Typically, most white blood cells (WBCs) in urine are neutrophils. They are round, larger than RBCs, possess a cell nucleus, and have a granular appearance. A few white blood cells can normally be found in the urine of healthy individuals (approximately <5/hpf, with females having slightly more). An increased number of WBCs is termed pyuria or leukocyturia and is associated with infection or inflammation of the urinary tract. WBCs can also appear in the urine following exercise or fever.[3]: 461–2
- Eosinophils – associated with allergic interstitial nephritis, atheroembolic disease
- Typically, most white blood cells (WBCs) in urine are neutrophils. They are round, larger than RBCs, possess a cell nucleus, and have a granular appearance. A few white blood cells can normally be found in the urine of healthy individuals (approximately <5/hpf, with females having slightly more). An increased number of WBCs is termed pyuria or leukocyturia and is associated with infection or inflammation of the urinary tract. WBCs can also appear in the urine following exercise or fever.[3]: 461–2

- Epithelial cells
- Epithelial cells form the lining of the urinary tract. Three types may occur in urine: squamous epithelial cells, transitional epithelial cells and renal tubular epithelial cells. Some laboratories do not distinguish between the three types of cells and simply report "epithelial cells" in general.[15]: 115–6
- Squamous epithelial cells line the urethra, as well as the vagina and the outer layer of the skin. They are very large, flat, and thin, with irregular borders and a single, small nucleus. They may fold into various shapes. They are not considered clinically significant, but if they are seen in large numbers they can indicate contamination of the sample by vaginal secretions or the skin of the urogenital area.[4]: 420–1 [7]: 143–5
- Transitional epithelial cells, also known as urothelial cells, line the urinary tract from the renal pelvis through the ureters and bladder and, in males, the upper (proximal) portion of the urethra. They are smaller than squamous cells and their shape varies based on the layer of epithelium from which they are derived, but they are most commonly round or pear-shaped.[7]: 143–5 They may have one or two nuclei.[15]: 115–6 Small numbers of these cells are found in normal urine; larger numbers can be seen after invasive procedures like catheterization or cystoscopy or in conditions that irritate the urinary tract, such as urinary tract infections.[7]: 145 In the absence of recent trauma to the urinary tract, clusters and sheets of transitional cells in the urine may indicate malignancy, requiring further investigation.[3]: 462–3
- Renal tubular epithelial cells (RTEs) line the collecting ducts and the distal and proximal tubules of the kidney.[7]: 146–8 They can be difficult to identify in unstained urine, as they look similar to urothelial cells and WBCs;[4]: 421 however, they are generally larger than WBCs and smaller than urothelial cells,[15]: 115–6 and collecting duct cells, unlike urothelial cells, often have a flat edge.[4]: 421 The presence of RTEs in high numbers is a significant finding, as this indicates damage to the renal tubules. This may occur in conditions such as acute tubular necrosis, drug or heavy metal toxicity, acute glomerulonephritis, kidney transplant rejection, trauma, and sepsis.[7]: 146–8 [3]: 463
Casts
- Red blood cell casts – associated with glomerulonephritis, vasculitis, or malignant hypertension
- White blood cell casts – associated with acute interstitial nephritis, exudative glomerulonephritis, or severe pyelonephritis
- Waxy casts – associated with chronic renal disease
- (Heme) granular casts – associated with acute tubular necrosis
Crystals

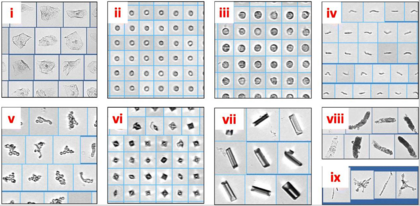
Various compounds in the urine can precipitate to form crystals. The composition of crystals can be identified based on their appearance and the pH of the urine (many types preferentially form at an acidic or alkaline pH).[3]: 467 Crystals that can be found in normal urine include uric acid, monosodium urate, triple phosphate (ammonium magnesium phosphate), calcium oxalate, and calcium carbonate.[7]: 161–2 Crystals can also appear as poorly defined aggregates of granular material, termed amorphous urates or amorphous phosphates (urates form in acid urine while phosphates form in alkaline urine). These are of no clinical significance, but they can interfere with microscopy by obscuring other elements (especially bacteria).[6]: 234–5 Some drugs, such as sulfonamides, may form crystals when excreted in the urine, and ammonium biurate crystals commonly occur in aged samples.[7]: 161–2 Certain types of crystals are characteristically associated with disease states. Leucine and tyrosine crystals may be observed in liver disease,[16] and cystine crystals indicate cystinuria (although they look identical to hexagonal variants of uric acid crystals, and can only be distinguished with further testing).[6]: 290 Cholesterol crystals may rarely be seen in nephrotic syndrome and chyluria.[6]: 299
Organisms
Microorganisms that can be observed in the urine include bacteria, yeast and Trichomonas vaginalis.[3]: 472 The urine of children with pinworm infections may contain Enterobius vermicularis eggs, and Schistosoma haematobium ova may be detected in urine samples from individuals with parasitic infestations.[7]: 176
Other elements
Mucus can occur in the urine, where it appears as translucent wavy strands under the microscope. The presence of mucus is not a clinically significant finding, but it can be confused with hyaline casts. Sperm may occasionally be observed in the urine of both males and females; in female children and vulnerable adults, this can indicate sexual abuse. Fat droplets and oval fat bodies may be present in a condition called lipiduria, which has various causes, most notably nephrotic syndrome. Contaminants from the outside environment, such as starch granules, hair, and clothing fibers, may be seen but are not reported.[7]: 176–80
Other methods
- Urine culture – a microbiological culture of urine samples, detecting bacteriuria, is indicated when a urinary tract infection is suspected.
- Ictotest – this test is used to detect the destruction of old red blood cells in the urine.
- Hemoglobin test – this tests for hemolysis in the blood vessels, a rupture in the capillaries of the glomerulus, or hemorrhage in the urinary system, which cause hemoglobin to appear in the urine.
Target parameters
Urine test results should always be interpreted using the reference range provided by the laboratory that performed the test, or using information provided by the test strip/device manufacturer.[17]
Ions and trace minerals
| Target | Lower limit | Upper limit | Unit | Comments | LOINC Codes |
|---|---|---|---|---|---|
| Nitrite | n/a | The presence of nitrites in urine, termed nitrituria, indicates the presence of coliform bacteria. | |||
| Sodium (Na) – per day | 150[19] | 300[19] | mmol / 24 h | A urinalysis is frequently ordered during the workup of acute kidney injury. Full kidney function can be detected through the simple dipstick method. | 2956-1 |
| Potassium (K) – per day | 40[19] | 90[19] | mmol / 24 h | Urine K may be ordered in the workup of hypokalemia. In case of gastrointestinal loss of K, the urine K will be low. In case of renal loss of K, the urine K levels will be high. Decreased levels of urine K are also seen in hypoaldosteronism and adrenal insufficiency. | 2829-0 |
| Urinary calcium (Ca) – per day | 2,5 | 6,25 | mmol / 24 h | An abnormally high level is called hypercalciuria and an abnormally low rate is called hypocalciuria. | 14637-3 |
| 100[20] | 250[20] | mg / 24 hours | 6874-2 | ||
| Phosphate (P) – per day | n/a[19] | 38[19] | mmol / 24 h | Phosphaturia is the hyperexcretion of phosphate in the urine. This condition is divided into primary and secondary types. Primary hyperphosphaturia is characterized by direct excess excretion of phosphate by the kidneys, as from primary kidney dysfunction, and also the direct action of many classes of diuretics on the kidneys. Additionally, secondary causes, including both types of hyperparathyroidism, cause hyperexcretion of phosphate in the urine. | 14881-7 |
A sodium-related parameter is fractional sodium excretion, which is the percentage of the sodium filtered by the kidney which is excreted in the urine. It is a useful parameter in acute kidney failure and oliguria, with a value below 1% indicating a prerenal disease and a value above 3%[21] indicating acute tubular necrosis or other kidney damage.
Proteins and enzymes
| Target | Lower limit | Upper limit | Unit | Comments |
|---|---|---|---|---|
| Protein | 0 | trace amounts[18] / 20 |
mg/dl | Proteins may be measured with the Albustix test. Since proteins are very large molecules (macromolecules), they are not normally present in measurable amounts in the glomerular filtrate or in the urine. The detection of protein in urine, called proteinuria, may indicate the permeability of the glomerulus is increased. This may be caused by renal infections or by other diseases that have secondarily affected the kidneys, such as hypertension, diabetes mellitus, jaundice, or hyperthyroidism. |
| Human chorionic gonadotropin (hCG) | – | 50[22] | U/l | This hormone appears in the urine of pregnant women. It also appears in cases of testicular cancer in men. Home pregnancy tests commonly detect this substance. |
Blood cells
| Target | Lower limit | Upper limit | Unit | Comments |
|---|---|---|---|---|
| Red blood cells (RBCs) / erythrocytes |
0[18][23] | 2[18] – 3[23] | per High Power Field (HPF) |
May be present as intact RBCs, which indicate bleeding. Even a trace amount of blood is enough to give the entire urine sample a red/pink hue, with difficulty in judging the amount of bleeding from a gross examination. Hematuria may be due to a generalized bleeding diathesis or a urinary tract-specific problem (trauma, stone...urolithiasis, infection, malignancy, etc.) or artifact of catheterization in case the sample is taken from a collection bag, in which case a fresh urine sample should be sent for a repeat test.
If the RBCs are of renal or glomerular origin (due to glomerulonephritis), the RBCs incur mechanical damage during the glomerular passage, and then osmotic damage along the tubules, so dysmorphic features appear. The dysmorphic RBCs in urine most characteristic of glomerular origin are called "G1 cells", doughnut-shaped rings with protruding round blebs sometimes looking like Mickey Mouse's head (with ears). Painless hematuria of nonglomerular origin may be a sign of urinary tract malignancy, which may warrant a more thorough cytological investigation. |
| RBC casts | n/a | 0 / negative[18] | ||
| White blood cells (WBCs) / leukocytes / (pus cells) |
0[18] | 2[18] / negative[18] | ||
| – | 10 | per µl or mm3 |
"Significant pyuria" at greater than or equal to 10 leucocytes per microlitre (µl) or cubic millimeter (mm3) | |
| "Blood" / (actually hemoglobin) |
n/a | 0 / negative[18] | dip-stick qualitative scale of 0 to 4+ | Hemoglobinuria is suggestive of in vivo hemolysis, but must be distinguished from hematuria. In case of hemoglobinuria, a urine dipstick shows presence of blood, but no RBCs are seen on microscopic examination. If hematuria is followed by artefactual ex vivo or in vitro hemolysis in the collected urine, then the dipstick test also will be positive for hemoglobin and will be difficult to interpret. The urine color may also be red due to excretion of reddish pigments or drugs. |
Other molecules
| Target | Lower limit | Upper limit | Unit | Comments |
|---|---|---|---|---|
| Glucose | n/a | 0 / negative[18] | Glucose can be measured with Benedict's test. Although glucose is easily filtered in the glomerulus, it is not present in the urine because all of the glucose filtered is normally reabsorbed from the renal tubules back into the blood. Presence of glucose in the urine is called glucosuria. | |
| Ketone bodies | n/a | 0 / negative[18] | With carbohydrate deprivation, such as starvation or high-protein diets, the body relies increasingly on the metabolism of fats for energy. This pattern is also seen in people with diabetes mellitus, when a lack of the hormone insulin prevents the body cells from using the large amounts of glucose available in the blood. This happens because insulin is necessary for the transport of glucose from the blood into the body cells. The metabolism of fat proceeds in a series of steps. First, triglycerides are hydrolyzed to fatty acids and glycerol. Second, the fatty acids are hydrolyzed into smaller intermediate compounds (acetoacetic acid, betahydroxybutyric acid, and acetone). Thirdly, the intermediate products are used in aerobic cellular respiration. When the production of the intermediate products of fatty acid metabolism (collectively known as ketone bodies) exceeds the ability of the body to metabolize these compounds, they accumulate in the blood and some end up in the urine (ketonuria). | |
| Bilirubin | n/a | 0 / negative[18] | The fixed phagocytic cells of the spleen and bone marrow destroy old red blood cells and convert the heme groups of hemoglobin to the pigment bilirubin. The bilirubin is secreted into the blood and carried to the liver, where it is bonded to (conjugated with) glucuronic acid, a derivative of glucose. Some of the conjugated bilirubin is secreted into the blood and the rest is excreted in the bile as bile pigment that passes into the small intestine. The blood normally contains a small amount of free and conjugated bilirubin. An abnormally high level of blood bilirubin may result from an increased rate of red blood cell destruction, liver damage (as in hepatitis and cirrhosis), and obstruction of the common bile duct, as with gallstones. An increase in blood bilirubin results in jaundice, a condition characterized by a brownish-yellow pigmentation of the skin and of the sclera of the eyes. | |
| Urobilinogen | 0.2[18] | 1.0[18] | Ehrlich units or mg/dL | |
| Creatinine | 4.8[19] | 19[19] | mmol / 24 h | |
| Urea | 12 | 20 | g / 24 h | |
| Uric acid | 250 | 750 | mg / 24 h | |
| Free catecholamines, dopamine – per day |
90[24] | 420[24] | μg / 24 hours | |
| Free cortisol | 28[25] or 30[26] | 280[25] or 490[26] | nmol/24 h | Values below threshold indicate Addison's disease, while values above indicate Cushing's syndrome. A value smaller than 200 nmol/24 h (72 µg/24 h[27]) strongly indicates absence of Cushing's syndrome.[26] |
| 10[28] or 11[27] | 100[28] or 176[27] | µg/24 h | ||
| Phenylalanine | 30.0 | mg/L[29] | In neonatal screening, a value above the upper limit defines phenylketonuria.[29] |
Other urine parameters
| Test | Lower limit | Upper limit | Unit | Comments | |
|---|---|---|---|---|---|
| Urine specific gravity | 1.003[12][18] | 1.030[12][18] | g/cc | This test detects the ion concentration of urine. Small amounts of protein or ketoacidosis tend to elevate the urine's specific gravity (SG). This value is measured using a urinometer and indicates hydration or dehydration. If the SG is under 1.010, the patient is hydrated; an SG value above 1.020 indicates dehydration. | |
| Osmolality | 400[19] | n/a[19] | mOsm/kg | Urine osmolality testing can be used in conjunction with Plasma osmolality tests to confirm diagnosis of SIADH[30] | |
| pH | 5[18] | 7[18] | (unitless) | ||
| Bacterial cultures | by urination | – | 100,000 | colony forming units per millilitre (CFU/mL) | Bacteriuria can be confirmed if a single bacterial species is isolated in a concentration greater than 100,000 CFU/ml of urine in clean-catch midstream urine specimens (one for men, two consecutive specimens with the same bacterium for women). |
| by bladder catheterisation | – | 100 | For urine collected via bladder catheterisation, the threshold is 100 CFU/ml of a single species. | ||
Drugs
Urine may be tested to determine whether an individual has engaged in recreational drug use. In this case, the urinalysis would be designed to detect whatever marker indicates drug use.[citation needed]
History
Helen Murray Free and her husband, Alfred Free, pioneered dry reagent urinalysis, resulting in the 1956 development of Clinistix (also known as Clinistrip), the first dip-and-read test for glucose in urine for patients with diabetes.[31] This breakthrough led to additional dip-and-read tests for proteins and other substances.[32] The invention was named a National Historic Chemical Landmark by the American Chemical Society in May 2010.[33]
See also
- Uroscopy, the ancient form of this analysis
- Urinary casts
- Proteinuria
- Urine test strip
- Urine collection device
- Pregnancy test, measures hCG levels in urine
References
- ^ Roxe, DM (1990), "A5417", Urinalysis (3rd ed.), Boston: Butterworths, PMID 21250145
- ^ Harper, Douglas. "Urinalysis". Online Etymology Dictionary. Archived from the original on 21 August 2012. Retrieved 26 September 2011.
- ^ a b c d e f g h i j k l McPherson, RA; Pincus, MR (2017). Henry's Clinical Diagnosis and Management by Laboratory Methods (23 ed.). Elsevier Health Sciences. ISBN 978-0-323-41315-2.
- ^ a b c d e f g Turgeon, ML (2016). Linné & Ringsrud's Clinical Laboratory Science: Concepts, Procedures, and Clinical Applications (7 ed.). Elsevier Mosby. ISBN 978-0-323-22545-8.
- ^ Oyaert, Matthijs; Delanghe, Joris (2019). "Progress in Automated Urinalysis". Annals of Laboratory Medicine. 39 (1): 15–22. doi:10.3343/alm.2019.39.1.15. ISSN 2234-3806. PMC 6143458. PMID 30215225.
- ^ a b c d e f g Haber, M.H.; Blomberg, D.; Galagan, K.; Glassy, E.F.; Ward, P.C.J. (2010). Color Atlas of the Urinary Sediment: An Illustrated Field Guide Based on Proficiency Testing. College of American Pathologists. ISBN 978-0-930304-87-4.
- ^ a b c d e f g h i j k l m n o p Brunzel, N.A. (2018). Fundamentals of Urine and Body Fluid Analysis (4 ed.). Elsevier. ISBN 978-0-323-37479-8.
- ^ a b c https://reference.medscape.com/slideshow/discolored-urine-6008332?src=wnl_critimg_171117_mscpref_v2&uac=20524DV&impID=1486503&faf=1#18 Archived 2018-04-30 at the Wayback Machine Medscape, 12 Causes of Discolored Urine.
- ^ Murphy, James (6 May 2009). "Movement Away From Phenolphthalein in Laxatives". JAMA. 301 (17): 1770. doi:10.1001/jama.2009.585. PMID 19417193.
- ^ "Urine color - Symptoms and causes". mayoclinic.org. Archived from the original on 14 September 2017. Retrieved 30 April 2018.
- ^ "Urine odor Causes". mayoclinic.org. Archived from the original on 9 January 2018. Retrieved 30 April 2018.
- ^ a b c d e Simerville JA, Maxted WC, Pahira JJ (March 2005). "Urinalysis: a comprehensive review". American Family Physician. 71 (6): 1153–62. PMID 15791892. Archived from the original on 2005-06-02.
- ^ Lehmann, R. (2021). "From bedside to bench-practical considerations to avoid pre-analytical pitfalls and assess sample quality for high-resolution metabolomics and lipidomics analyses of body fluids". Analytical and Bioanalytical Chemistry. 413 (22): 5567–5585. doi:10.1007/s00216-021-03450-0.
- ^ Peterson, L.M.; Reed, H.S. (2019). "Hematuria". Primary Care: Clinics in Office Practice. 46 (2). doi:10.1016/j.pop.2019.02.008.
- ^ a b c Mundt, L.A.; Shanahan, K. (2016). Graff's Textbook of Urinalysis and Body Fluids (3 ed.). Wolters Kluwer. ISBN 978-1-4963-2016-2.
- ^ Echeverry, G.; Hortin, G.L.; Rai, A.J. (2010). "Introduction to urinalysis: historical perspectives and clinical application". Methods in Molecular Biology. 641: 1–12. doi:10.1007/978-1-60761-711-2_1.
- ^ "Reference Ranges and What They Mean". Lab Tests Online (USA). Archived from the original on 28 August 2013. Retrieved 22 June 2013.
- ^ a b c d e f g h i j k l m n o p q r Normal Reference Range Table Archived December 25, 2011, at the Wayback Machine from The University of Texas Southwestern Medical Center at Dallas. Used in Interactive Case Study Companion to Pathologic basis of disease.
- ^ a b c d e f g h i j Reference range list from Uppsala University Hospital ("Laborationslista"). Artnr 40284 Sj74a. Issued on April 22, 2008
- ^ a b medscape.com - Urine Calcium: Laboratory Measurement and Clinical Utility Archived 2011-09-06 at the Wayback Machine By Kevin F. Foley, PhD, DABCC; Lorenzo Boccuzzi, DO. Posted: 12/26/2010; Laboratory Medicine. 2010;41(11):683–686. © 2010 American Society for Clinical Pathology. In turn citing:
- Wu HBA. Tietz Guide to Clinical Laboratory Tests. 4th ed. St. Louis, MO: Saunders, Elsevier; 2006.
- ^ "MedlinePlus Medical Encyclopedia: Fractional excretion of sodium". Archived from the original on 2009-05-03. Retrieved 2009-05-02.
- ^ Ajubi NE, Nijholt N, Wolthuis A (2005). "Quantitative automated human chorionic gonadotropin measurement in urine using the Modular Analytics E170 module (Roche)". Clinical Chemistry and Laboratory Medicine. 43 (1): 68–70. doi:10.1515/CCLM.2005.010. PMID 15653445. S2CID 42575043.
- ^ a b "medical.history.interview: Lab Values". Archived from the original on 2012-12-12. Retrieved 2008-10-21.
- ^ a b "University of Colorado Laboratory Reference Ranges". Archived from the original on 2008-05-07. Retrieved 2008-10-21.
- ^ a b Converted from µg/24 h, using molar mass of 362.460 g/mol
- ^ a b c Görges R, Knappe G, Gerl H, Ventz M, Stahl F (1999). "Diagnosis of Cushing's syndrome: Re-evaluation of midnight plasma cortisol vs urinary free cortisol and low-dose dexamethasone suppression test in a large patient group". Journal of Endocrinological Investigation. 22 (4): 241–249. doi:10.1007/bf03343551. PMID 10342356. S2CID 1239611.
- ^ a b c Converted from nmol/24h, using molar mass of 362.460 g/mol
- ^ a b MedlinePlus - Cortisol – urine Archived 2016-05-29 at the Wayback Machine. Update Date: 11/23/2009. Updated by: Ari S. Eckman. Also reviewed by David Zieve.
- ^ a b Kim NH, Jeong JS, Kwon HJ, Lee YM, Yoon HR, Lee KR, Hong SP (2010). "Simultaneous diagnostic method for phenylketonuria and galactosemia from dried blood spots using high-performance liquid chromatography-pulsed amperometric detection". Journal of Chromatography B. 878 (21): 1860–1864. doi:10.1016/j.jchromb.2010.04.038. PMID 20494631.
- ^ William C. Wilson; Christopher M. Grande; David B. Hoyt (2007-02-05). Trauma: Critical Care. CRC Press. pp. 179–. ISBN 978-1-4200-1684-0.
- ^ "Helen M. Free". American Chemical Society. Archived from the original on 13 November 2016. Retrieved 13 November 2016.
- ^ "The Development of Diagnostic Test Strips" (PDF). American Chemical Society. Archived (PDF) from the original on 7 February 2017. Retrieved 13 November 2016.
- ^ "Al and Helen Free and the development of diagnostic test strips". American Chemical Society. Archived from the original on 13 November 2016. Retrieved 13 November 2016.
