C-peptide: Difference between revisions
m →Function: |pmid=18493738 |doi=10.1007/s00125-008-1032-x |
m →Function: pmid=11508275 |doi=10.1007/s001250100570 |
||
| Line 35: | Line 35: | ||
'''Cellular effects of C-peptide:''' |
'''Cellular effects of C-peptide:''' |
||
C-peptide has been shown to bind to the surface of a number of cell types such as neuronal, endothelial, fibroblast and renal tubular, at nanomolar concentrations to a receptor that is likely G-protein coupled. The signal activates Ca^2+ dependent intracellular signaling pathways such as MAPK, PLCγ and PKC, leading to upregulation of a range of transcription factors as well as eNOS and Na+K+ATPase activities.<ref>{{cite journal |author=Hills CE, Brunskill NJ |title=Intracellular signalling by C-peptide |journal=Exp Diabetes Res |volume=2008 |issue= |pages=635158 |year=2008 |pmid=18382618 |pmc=2276616 |doi=10.1155/2008/635158 |url=}}</ref> The latter two enzymes are known to have reduced activities in patients with type I diabetes and have been implicated in the development of long-terms complications of type I diabetes such as peripheral and autonomic neuropathy. |
C-peptide has been shown to bind to the surface of a number of cell types such as neuronal, endothelial, fibroblast and renal tubular, at nanomolar concentrations to a receptor that is likely G-protein coupled. The signal activates Ca^2+ dependent intracellular signaling pathways such as MAPK, PLCγ and PKC, leading to upregulation of a range of transcription factors as well as eNOS and Na+K+ATPase activities.<ref>{{cite journal |author=Hills CE, Brunskill NJ |title=Intracellular signalling by C-peptide |journal=Exp Diabetes Res |volume=2008 |issue= |pages=635158 |year=2008 |pmid=18382618 |pmc=2276616 |doi=10.1155/2008/635158 |url=}}</ref> The latter two enzymes are known to have reduced activities in patients with type I diabetes and have been implicated in the development of long-terms complications of type I diabetes such as peripheral and autonomic neuropathy. |
||
In vivo studies in animal models of type 1 diabetes have established that C-peptide administration results in significant improvements in nerve and kidney function. Thus, in animals with early signs of diabetes-induced neuropathy, C peptide treatment in replacement dosage results in improved peripheral nerve function, as evidenced by increased nerve conduction velocity, increased nerve Na+,K+ ATPase activity, and significant amelioration of nerve structural changes.<ref>Sima |
In vivo studies in animal models of type 1 diabetes have established that C-peptide administration results in significant improvements in nerve and kidney function. Thus, in animals with early signs of diabetes-induced neuropathy, C peptide treatment in replacement dosage results in improved peripheral nerve function, as evidenced by increased nerve conduction velocity, increased nerve Na+,K+ ATPase activity, and significant amelioration of nerve structural changes.<ref>{{cite journal |author=Sima AA, Zhang W, Sugimoto K, ''et al.'' |title=C-peptide prevents and improves chronic Type I diabetic polyneuropathy in the BB/Wor rat |journal=[[Diabetologia]] |volume=44 |issue=7 |pages=889–97 |year=2001 |month=July |pmid=11508275 |doi=10.1007/s001250100570 |url=}}</ref> Likewise, C-peptide administration in animals that had C-peptide deficiency (type 1 model) with nephropathy improves renal function and structure; it decreases urinary albumin excretion and prevents or decreases diabetes-induced glomerular changes secondary to mesangial matrix expansion.<ref>{{cite journal |author=Samnegård B, Jacobson SH, Jaremko G, Johansson BL, Sjöquist M |title=Effects of C-peptide on glomerular and renal size and renal function in diabetic rats |journal=Kidney Int. |volume=60 |issue=4 |pages=1258–65 |year=2001 |month=October |pmid=11576340 |doi=10.1046/j.1523-1755.2001.00964.x |url=}}</ref><ref>{{cite journal |author=Samnegård B, Jacobson SH, Jaremko G, ''et al.'' |title=C-peptide prevents glomerular hypertrophy and mesangial matrix expansion in diabetic rats |journal=Nephrol. Dial. Transplant. |volume=20 |issue=3 |pages=532–8 |year=2005 |month=March |pmid=15665028 |doi=10.1093/ndt/gfh683 |url=}}</ref><ref>{{cite journal |author=Nordquist L, Brown R, Fasching A, Persson P, Palm F |title=Proinsulin C-peptide reduces diabetes-induced glomerular hyperfiltration via efferent arteriole dilation and inhibition of tubular sodium reabsorption |journal=Am. J. Physiol. Renal Physiol. |volume=297 |issue=5 |pages=F1265–72 |year=2009 |month=November |pmid=19741019 |pmc=2781335 |doi=10.1152/ajprenal.00228.2009 |url=}}</ref><ref>{{cite journal |author=Nordquist L, Wahren J |title=C-Peptide: the missing link in diabetic nephropathy? |journal=Rev Diabet Stud |volume=6 |issue=3 |pages=203–10 |year=2009 |pmid=20039009 |pmc=2827272 |doi=10.1900/RDS.2009.6.203 |url=}}</ref> C-peptide also has been reported to have anti-inflammatory effects as well as aid repair of smooth muscle cells.<ref>{{cite journal |author=Luppi P, Cifarelli V, Tse H, Piganelli J, Trucco M |title=Human C-peptide antagonises high glucose-induced endothelial dysfunction through the nuclear factor-kappaB pathway |journal=[[Diabetologia]] |volume=51 |issue=8 |pages=1534–43 |year=2008 |month=August |pmid=18493738 |doi=10.1007/s00125-008-1032-x |url=}}</ref><ref>{{cite journal |author=Mughal RS, Scragg JL, Lister P, ''et al.'' |title=Cellular mechanisms by which proinsulin C-peptide prevents insulin-induced neointima formation in human saphenous vein |journal=[[Diabetologia]] |volume=53 |issue=8 |pages=1761–71 |year=2010 |month=August |pmid=20461358 |pmc=2892072 |doi=10.1007/s00125-010-1736-6 |url=}}</ref> |
||
==Uses== |
==Uses== |
||
Revision as of 10:11, 26 April 2011
| |
| Identifiers | |
|---|---|
| MeSH | C-Peptide |
PubChem CID
|
|
| Properties | |
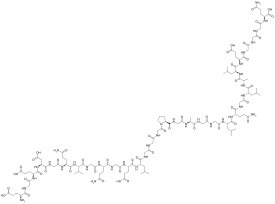
| C112H179N35O46 | |
| Molar mass | 3020.29 g/mol |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Proinsulin C-peptide was first described in 1967 in connection with the discovery of the insulin biosynthesis.[2] It serves as an important linker between the A- and the B- chains of insulin and facilitates the efficient assembly, folding, and processing of insulin in the endoplasmic reticulum. Equimolar amounts of C-peptide and insulin are then stored in secretory granules of the pancreatic beta cells and both are eventually released to the portal circulation. Initially, the sole interest in C-peptide was as a marker of insulin secretion and has as such been of great value in furthering the understanding of the pathophysiology of type 1 and type 2 diabetes. The first documented use of the C-peptide test was in 1972. During the past decade, however, C-peptide has been found to be a bioactive peptide in its own right, with effects on microvascular blood flow and tissue health.
C-peptide should not be confused with c-reactive protein or Protein C.
Function
Cellular effects of C-peptide: C-peptide has been shown to bind to the surface of a number of cell types such as neuronal, endothelial, fibroblast and renal tubular, at nanomolar concentrations to a receptor that is likely G-protein coupled. The signal activates Ca^2+ dependent intracellular signaling pathways such as MAPK, PLCγ and PKC, leading to upregulation of a range of transcription factors as well as eNOS and Na+K+ATPase activities.[3] The latter two enzymes are known to have reduced activities in patients with type I diabetes and have been implicated in the development of long-terms complications of type I diabetes such as peripheral and autonomic neuropathy. In vivo studies in animal models of type 1 diabetes have established that C-peptide administration results in significant improvements in nerve and kidney function. Thus, in animals with early signs of diabetes-induced neuropathy, C peptide treatment in replacement dosage results in improved peripheral nerve function, as evidenced by increased nerve conduction velocity, increased nerve Na+,K+ ATPase activity, and significant amelioration of nerve structural changes.[4] Likewise, C-peptide administration in animals that had C-peptide deficiency (type 1 model) with nephropathy improves renal function and structure; it decreases urinary albumin excretion and prevents or decreases diabetes-induced glomerular changes secondary to mesangial matrix expansion.[5][6][7][8] C-peptide also has been reported to have anti-inflammatory effects as well as aid repair of smooth muscle cells.[9][10]
Uses
- Newly diagnosed diabetes patients often get their C-peptide levels measured as a means of distinguishing type 1 diabetes and type 2 diabetes. C-peptide levels are measured instead of insulin levels because insulin concentration in the portal vein ranges from two to ten times higher than in the peripheral circulation. The liver extracts about half the insulin reaching it in the plasma, but this varies with the nutritional state. The pancreas of patients with type 1 diabetes is unable to produce insulin and therefore they will usually have a decreased level of C-peptide, whereas C-peptide levels in type 2 patients are normal or higher than normal. Measuring C-peptide in patients injecting synthetic insulin can help to determine how much of their own natural insulin these patients are still producing, of if they produce any at all.
- C-peptide is also used for determining the possibility of gastrinomas associated with Multiple Endocrine Neoplasm syndromes (MEN 1). Since a significant number of gastrinomas are associated with MEN involving other hormone producing organs (pancreas, parathyroids, and pituitary), higher levels of C-peptide together with the presence of a gastrinoma suggest that organs besides the stomach may harbor neoplasms.
- C-peptide levels are checked in women with Polycystic Ovarian Syndrome (PCOS) to determine degree of insulin resistance.
Both excess body weight and a high plasma concentration of C-peptide predispose men with a subsequent diagnosis of prostate cancer to an increased likelihood of dying of the disease, according to the results of a long-term survival analysis reported in the October 6, 2008 Online First issue of Lancet Oncology.
Therapeutics
Several physiological effects have been observed in several Phase 1 and exploratory Phase 2 studies in almost 300 type 1 diabetes patients, who lacked endogenous C-peptide. Improvements were seen on diabetic peripheral neuropathy, nephropathy and other decrements associated with long-term complications of type I diabetes.[11] [12] [13] [14] [15] [16] [17] [18] .[19] So far, dosing with C-peptide has shown to be safe and there were no effects of C-peptide demonstrated in healthy subjects (who make their own C-peptide).
A company based in La Jolla, California called Cebix Incorporated has secured manufacturing and other patents in a number of countries for C-peptide, and aims to commercialize it as a therapeutic for diabetic neuropathy, retinopathy and nephropathy. Cebix acquired Creative Peptides AB of Sweden which was founded in 1996 by leading scientists in the field of research at the Karolinska Institute and the Royal Institute of Technology in Stockholm. Creative Peptides conducted a majority of the preliminary research on biosynthetic C-peptide as a treatment therapeutic. The peptide is currently being formulated into a once-weekly subcutaneous use and a pivotal phase 2b study in diabetic neuropathy will be initiated late 2011.
External links
www.cebix.com [1]
References
- ^ C-Peptide - Compound Summary, PubChem.
- ^ Steiner D.F., Cunningham D., Spigelman L., Aten B. (1967). "Insulin Biosynthesis: Evidence for a Precursor". Science. 157 (789): 697–700. doi:10.1126/science.157.3789.697. PMID 4291105.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hills CE, Brunskill NJ (2008). "Intracellular signalling by C-peptide". Exp Diabetes Res. 2008: 635158. doi:10.1155/2008/635158. PMC 2276616. PMID 18382618.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Sima AA, Zhang W, Sugimoto K; et al. (2001). "C-peptide prevents and improves chronic Type I diabetic polyneuropathy in the BB/Wor rat". Diabetologia. 44 (7): 889–97. doi:10.1007/s001250100570. PMID 11508275.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Samnegård B, Jacobson SH, Jaremko G, Johansson BL, Sjöquist M (2001). "Effects of C-peptide on glomerular and renal size and renal function in diabetic rats". Kidney Int. 60 (4): 1258–65. doi:10.1046/j.1523-1755.2001.00964.x. PMID 11576340.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Samnegård B, Jacobson SH, Jaremko G; et al. (2005). "C-peptide prevents glomerular hypertrophy and mesangial matrix expansion in diabetic rats". Nephrol. Dial. Transplant. 20 (3): 532–8. doi:10.1093/ndt/gfh683. PMID 15665028.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nordquist L, Brown R, Fasching A, Persson P, Palm F (2009). "Proinsulin C-peptide reduces diabetes-induced glomerular hyperfiltration via efferent arteriole dilation and inhibition of tubular sodium reabsorption". Am. J. Physiol. Renal Physiol. 297 (5): F1265–72. doi:10.1152/ajprenal.00228.2009. PMC 2781335. PMID 19741019.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nordquist L, Wahren J (2009). "C-Peptide: the missing link in diabetic nephropathy?". Rev Diabet Stud. 6 (3): 203–10. doi:10.1900/RDS.2009.6.203. PMC 2827272. PMID 20039009.
- ^ Luppi P, Cifarelli V, Tse H, Piganelli J, Trucco M (2008). "Human C-peptide antagonises high glucose-induced endothelial dysfunction through the nuclear factor-kappaB pathway". Diabetologia. 51 (8): 1534–43. doi:10.1007/s00125-008-1032-x. PMID 18493738.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mughal RS, Scragg JL, Lister P; et al. (2010). "Cellular mechanisms by which proinsulin C-peptide prevents insulin-induced neointima formation in human saphenous vein". Diabetologia. 53 (8): 1761–71. doi:10.1007/s00125-010-1736-6. PMC 2892072. PMID 20461358.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Johansson BL, Borg K, Fernqvist-Forbes E, Kernell A, Odergren T, Wahren J (2000). "Beneficial effects of C-peptide on incipient nephropathy and neuropathy in patients with Type 1 diabetes mellitus". Diabet. Med. 17 (3): 181–9. doi:10.1046/j.1464-5491.2000.00274.x. PMID 10784221.
Respiratory heart rate variability increased by 21 +/- 9% (P < 0.05) during treatment with C-peptide [...] C-peptide ameliorates autonomic and sensory nerve dysfunction in patients with Type 1 diabetes mellitus.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Marques RG, Fontaine MJ, Rogers J (2004). "C-peptide: much more than a byproduct of insulin biosynthesis". Pancreas. 29 (3): 231–8. PMID 15367890.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Wahren J, Ekberg K, Samnegård B, Johansson BL (2001). "C-peptide: a new potential in the treatment of diabetic nephropathy". Curr. Diab. Rep. 1 (3): 261–6. doi:10.1007/s11892-001-0044-4. PMID 12643208.
Administration of C-peptide to physiologic concentrations in patients with type 1 diabetes and incipient nephropathy for periods of 3 hours to 3 months is accompanied by reduced glomerular hyperfiltration and filtration fraction, and diminished urinary albumin excretion. C-peptide replacement together with insulin therapy may be beneficial in type 1 diabetes patients with nephropathy.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Wahren J (2004). "C-peptide: new findings and therapeutic implications in diabetes". Clin Physiol Funct Imaging. 24 (4): 180–9. doi:10.1111/j.1475-097X.2004.00558.x. PMID 15233831.
In patients with type 1 diabetes, beneficial effects have been demonstrated on sensory nerve conduction velocity, vibration perception and autonomic nerve function. C-peptide also augments blood flow in several tissues in type 1 diabetes via its stimulation of endothelial NO release, emphasizing a role for C-peptide in maintaining vascular homeostasis.
{{cite journal}}:|access-date=requires|url=(help) - ^ Kamiya H, Zhang W, Sima AA (2004). "C-peptide prevents nociceptive sensory neuropathy in type 1 diabetes". Ann. Neurol. 56 (6): 827–35. doi:10.1002/ana.20295. PMID 15497155.
we conclude that replacement of insulinomimetic C-peptide prevents abnormalities of neurotrophins, their receptors, and nociceptive neuropeptides in type 1 BB/Wor-rats, resulting in the prevention of C-fiber pathology and nociceptive sensory nerve dysfunction. The data indicate that perturbed insulin/C-peptide action plays an important pathogenetic role in nociceptive sensory neuropathy and that C-peptide replacement may be of benefit in treating painful diabetic neuropathy in insulin-deficient diabetic conditions.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Ziegler D (2004). "Polyneuropathy in the diabetic patient--update on pathogenesis and management". Nephrol. Dial. Transplant. 19 (9): 2170–5. doi:10.1093/ndt/gfh398. PMID 15252164. Retrieved 2008-01-07.
- ^ Wahren J, Ekberg K, Jörnvall H (2007). "C-peptide is a bioactive peptide". Diabetologia. 50 (3): 503–9. doi:10.1007/s00125-006-0559-y. PMID 17235526.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Wahren, J (2007). "C-peptide and Neuropathy in Type 1 Diabetes". Immunology, Endocrine & Metabolic Agents - Medicinal Chemistry. 7 (1): 69–77. doi:10.2174/187152207779802455. Retrieved 2008-01-07.
C-peptide corrects diabetes-induced reductions in endoneurial blood flow and in Na+,K+-ATPase activity. In vitro studies demonstrate that C-peptide binds specifically to cell membranes, activating a G-protein coupled receptor as well as Ca2+-, PKC- and MAPK-dependent signaling pathways, resulting in stimulation of Na+,K+-ATPase and endothelial nitric oxide synthase (eNOS). In addition, C-peptide activates transcription factors resulting in augmented eNOS mRNA and protein content of endothelial cells and modulation of neurotrophic factors as well as apoptotic phenomena in neuroblastoma cells. Combined, the results demonstrate that C-peptide is a bioactive peptide, possibly of importance in the treatment of neuropathy in type 1 diabetes.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Dan Ziegler. "New drugs to prevent or treat diabetic polyneuropathy" (pdf). Retrieved 2008-01-07. [dead link]
