Rapidly progressive glomerulonephritis
| Rapidly progressive glomerulonephritis | |
|---|---|
| Specialty | Nephrology |
Rapidly progressive glomerulonephritis (RPGN) is a syndrome of the kidney that is characterized by a rapid loss of renal function,[1][2] (usually a 50% decline in the glomerular filtration rate (GFR) within 3 months)[2] with glomerular crescent formation seen in at least 50%[2] or 75%[1] of glomeruli seen on kidney biopsies. If left untreated, it rapidly progresses into acute renal failure[3] and death within months. In 50% of cases, RPGN is associated with an underlying disease such as Goodpasture syndrome, systemic lupus erythematosus, or Wegener granulomatosis; the remaining cases are idiopathic. Regardless of the underlying cause, RPGN involves severe injury to the kidneys' glomeruli, with many of the glomeruli containing characteristic glomerular crescents (crescent-shaped scars).[4] Because of this microscopic feature, RPGN is also called crescentic glomerulonephritis.[5][4]
Presentation
Patients with RPGN have blood in the urine (hematuria), urinary protein (proteinuria), and occasionally high blood pressure (hypertension) and edema. The clinical picture is consistent with nephritic syndrome, although the degree of proteinuria may occasionally exceed 3 g/24 h, a range associated with nephrotic syndrome. Untreated disease may progress to decreased urinary volume (oliguria), which is associated with poor kidney function.
Treatment
Treatment depends on the underlying disease process. For example, plasmapheresis, corticosteroids, and cytotoxic drugs may promote recovery in Goodpasture syndrome, a cause of type I RPGN. Despite even early treatment, however, many patients with RPGN may ultimately require dialysis and possibly renal transplant.
Classification
RPGN can be classified into three types, based upon the immunofluorescence patterns.[6]
- In type I RPGN, which accounts for approximately 20% of RPGN cases, injury is caused by antibodies directed against the glomerular basement membrane.
- Type II RPGN accounts for roughly 25% of RPGN cases and is characterized by the deposition of immune complexes in the glomerulus.
- The remainder of RPGN cases are type III, or pauci-immune RPGN, which features antibodies directed against neutrophils (anti-neutrophil cytoplasmic antibodies, ANCA).
Type I
Accounting for approximately 20% of RPGN, type I RPGN is characterized by the presence of autoantibodies directed against the glomerular basement membrane (GBM). It is also called anti-GBM glomerulonephritis. The antibodies are directed against a particular protein found in the GBM, type IV collagen, specifically the noncollagenous region of its α3 chain.[7]
In addition to the anti-GBM antibodies, some cases of type I RPGN are also associated with antibodies directed against the basement membrane of lung alveoli, producing Goodpasture syndrome. The majority of type I disease, however, features anti-GBM antibodies alone; these cases are considered idiopathic.[7]
Type II
RPGN caused by the deposition of immune complexes accounts for 25% of RPGN and is classified as type II. Thus any immune complex disease that involves the glomerulus may progress to RPGN if severe enough. These diseases include systemic lupus erythematosus, acute proliferative glomerulonephritis, Henoch-Schönlein purpura, and IgA nephropathy.[7] While polyarteritis nodosa also involves vasculitis associated immune complex deposition that can lead to renal failure, it is not considered part of type-II RPGN because it mainly affects medium sized vessels and does not necessarily involve the kidneys.
Type III
Also known as pauci-immune RPGN, type III RPGN accounts for 55% of RPGN and features neither immune complex deposition nor anti-GBM antibodies. Instead, the glomeruli are damaged in an undefined manner, perhaps through the activation of neutrophils in response to anti-neutrophil cytoplasmic antibodies (ANCA). Type III RPGN may be isolated to the glomerulus (primary, or idiopathic) or associated with a systemic disease (secondary). In most cases of the latter, the systemic disease is an ANCA-associated vasculitis such as Wegener granulomatosis, microscopic polyangiitis, or Churg-Strauss syndrome.[7]
Classification of type III RPGN into primary or secondary may be unnecessary, as primary type III RPGN and secondary type III RPGN may represent a spectrum of the same disease process.[7]
The ANCA form may have a more favorable response to treatment than other forms.[8]
Type IV
Type 4 has features of both types 1 and 3. This is also called "double-antibody" positive disease.
Signs and symptoms
Most types of RPGN are characterized by severe and rapid loss of kidney function featuring severe hematuria (blood in the urine), red blood cell casts in the urine, and proteinuria (protein in the urine), sometimes exceeding 3 g protein/24 h, a range associated with nephrotic syndrome. Some patients also experience hypertension (high blood pressure) and edema. Severe disease is characterized by pronounced oliguria or anuria, which portends a poor prognosis.[7]
Serum analysis often aids in the diagnosis of a specific underlying disease. The presence of anti-GBM antibodies suggests type I RPGN; antinuclear antibodies (ANA) may support a diagnosis of systemic lupus erythematosus and type II RPGN; and type III and idiopathic RPGN are frequently associated with ANCA-positive serum.[7]
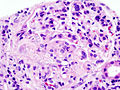
Crescent formation
Despite the wide variety of diseases that cause RPGN, all types of RPGN are characterized by glomeruluar injury and the formation of crescents. Severe injury and GBM rupture leads to the leakage of plasma proteins through the GBM. Of these proteins, fibrin is thought to contribute most strongly to crescent formation. Epithelial cells lining the Bowman capsule respond to the leaked fibrin and proliferate. Infiltrating white blood cells such as monocytes and macrophages may also proliferate. These proliferating cells surround and compress the glomerulus, forming a crescent-shaped scar that is readily visible on light microscopy of a renal biopsy.[7]
Additional images
-
Crescentic glomerulonephritis
References
- ^ a b TheFreeDictionary > rapidly progressive glomerulonephritis Citing: McGraw-Hill Concise Dictionary of Modern Medicine. 2002
- ^ a b c eMedicine > Glomerulonephritis, Crescentic Author: Malvinder S Parmar. Updated: Sep 25, 2008
- ^ "rapidly progressive glomerulonephritis" at Dorland's Medical Dictionary
- ^ a b "Renal Pathology". Retrieved 2008-11-25. Cite error: The named reference "urlRenal Pathology" was defined multiple times with different content (see the help page).
- ^ "iROCKET Learning Module: Glomerular Pathology, Case I".
- ^ Ghosh, Amit K. (2008). Mayo Clinic Internal Medicine Review: Eighth Edition (Mayo Clinic Internal Medicine Review). Informa Healthcare. p. 694. ISBN 1-4200-8478-X.
- ^ a b c d e f g h Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, MO: Elsevier Saunders. pp. pp976–8. ISBN 0-7216-0187-1.
{{cite book}}:|pages=has extra text (help)CS1 maint: multiple names: authors list (link) - ^ Alexopoulos E, Gionanlis L, Papayianni E, Kokolina E, Leontsini M, Memmos D (2006). "Predictors of outcome in idiopathic rapidly progressive glomerulonephritis (IRPGN)". BMC Nephrol. 7: 16. doi:10.1186/1471-2369-7-16. PMC 1660564. PMID 17078867.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link)